Constipation is a surprisingly common issue that affects millions of people worldwide. While occasional difficulty passing stool is normal, persistent trouble can disrupt daily life and signal underlying health concerns. Understanding why you can't poop—along with practical ways to find relief and knowing when it's time to consult a doctor—is essential for maintaining digestive wellness.
Common Causes of Constipation
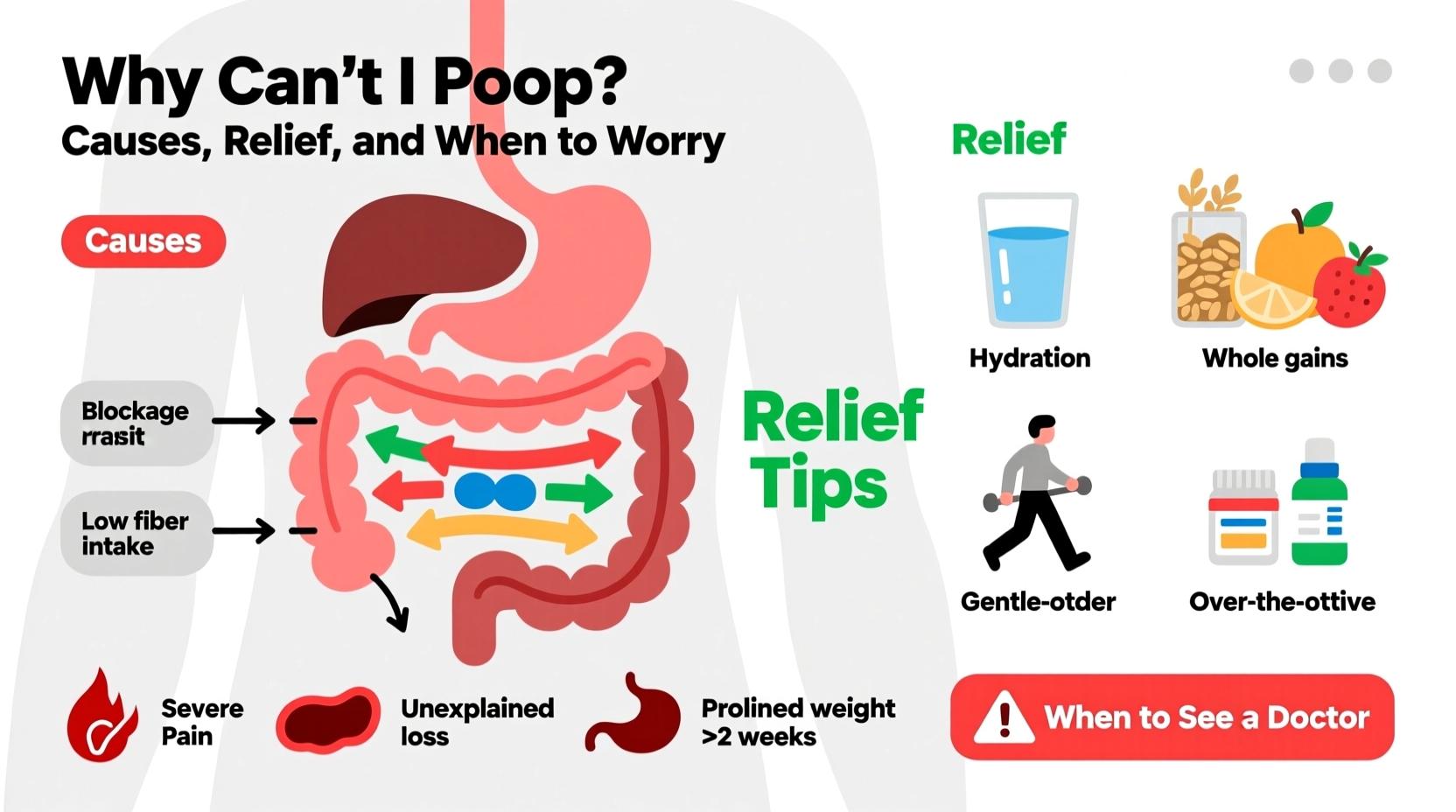
Several factors contribute to the inability to have a bowel movement. These range from lifestyle habits to medical conditions. Identifying the root cause is the first step toward effective treatment.
- Diet low in fiber: Insufficient intake of fruits, vegetables, whole grains, and legumes slows digestion.
- Inadequate fluid consumption: Dehydration hardens stool, making it difficult to pass.
- Lack of physical activity: Sedentary lifestyles reduce intestinal motility.
- Ignoring the urge to go: Delaying bowel movements regularly can weaken signals over time.
- Medications: Opioids, certain antidepressants, iron supplements, and antacids containing aluminum or calcium may cause constipation.
- Hormonal imbalances: Conditions like hypothyroidism or diabetes affect gut function.
- Intestinal disorders: Irritable bowel syndrome (IBS), colon cancer, or structural issues such as strictures or obstructions.
Natural Relief Strategies That Work
Before turning to medication, many individuals benefit significantly from simple lifestyle adjustments. These evidence-based methods support healthy digestion and promote regularity.
- Increase dietary fiber gradually: Aim for 25–30 grams per day from sources like oats, chia seeds, prunes, pears, and leafy greens. Sudden increases can cause bloating, so build up slowly.
- Stay hydrated: Drink at least 6–8 glasses of water daily. Warm liquids, especially in the morning, can trigger peristalsis—the wave-like muscle contractions that move stool through the intestines.
- Move your body: Even a 20-minute walk after meals enhances gastrointestinal transit time. Yoga poses like knees-to-chest or seated twists also aid digestion.
- Establish a bathroom routine: Try sitting on the toilet at the same time every day, preferably after breakfast, to train your body’s natural reflexes.
- Optimize toilet posture: Use a small footstool to elevate your knees above your hips, mimicking a squatting position. This straightens the anorectal angle and eases evacuation.
“The gut thrives on rhythm. Regular eating, sleeping, and elimination patterns are foundational to digestive health.” — Dr. Lena Torres, Gastroenterologist
When Home Remedies Aren’t Enough: Over-the-Counter Options
If lifestyle changes don’t bring improvement within a few days, short-term use of OTC laxatives may be appropriate. However, these should not be used long-term without medical supervision.
| Type | How It Works | Examples | Best For |
|---|---|---|---|
| Bulk-forming | Adds fiber to soften stool and increase bulk | Psyllium (Metamucil), methylcellulose (Citrucel) | Daily prevention; safest for long-term use |
| Osmotic | Draws water into the colon to loosen stool | Polyethylene glycol (MiraLAX), lactulose | Occasional relief; effective but may cause gas |
| Stimulant | Triggers intestinal contractions | Bisacodyl (Dulcolax), senna (Senokot) | Short-term use only; risk of dependency |
| Stool softeners | Mixes water into stool to prevent straining | Docusate sodium (Colace) | Post-surgery or during recovery |
Mini Case Study: Recovering Regularity After Surgery
Sarah, a 48-year-old office worker, underwent abdominal surgery and was prescribed opioid painkillers. Within two days, she stopped having bowel movements despite drinking extra water. She felt bloated and uncomfortable. Her primary care physician advised her to start MiraLAX and docusate, increase prune juice intake, and begin gentle walking three times daily. By day four, she passed soft stool without strain. Over the next two weeks, she phased out medications while maintaining high-fiber meals and consistent movement. Her case highlights how multiple factors—medication, reduced mobility, and post-op anxiety—can combine to cause temporary but distressing constipation.
Red Flags: When to Worry and Seek Medical Help
Most cases of constipation resolve with self-care. However, certain symptoms indicate a need for prompt medical evaluation.
- Severe abdominal pain or cramping
- This could suggest bowel obstruction or fecal impaction.
- Blood in stool
- May indicate hemorrhoids, anal fissures, or more serious conditions like colorectal cancer.
- Unintentional weight loss
- Especially when paired with changes in bowel habits, this warrants investigation.
- No bowel movement for over 10 days
- Chronic retention can lead to overflow diarrhea or megacolon.
- New onset after age 50
- First-time constipation later in life requires screening for tumors or metabolic disease.
Checklist: When to See a Doctor
- Constipation lasts longer than 3 weeks despite home efforts
- You experience vomiting along with no bowel movement
- There’s a noticeable change in bowel pattern without explanation
- You feel full quickly or lose appetite consistently
- You’re dependent on laxatives to have a bowel movement
Frequently Asked Questions
Can stress really stop me from pooping?
Yes. The gut and brain are closely linked via the gut-brain axis. High stress levels can slow digestion by activating the sympathetic nervous system, which reduces blood flow and motility in the intestines. Managing stress through mindfulness, breathing exercises, or therapy often improves bowel regularity.
Is it dangerous to hold in poop?
Occasionally delaying a bowel movement isn’t harmful, but doing so frequently can desensitize the rectum and lead to chronic constipation. Over time, this habit may result in stool buildup and harder-to-treat issues like fecal impaction.
Are probiotics helpful for constipation?
Some strains, particularly Bifidobacterium lactis and Lactobacillus casei, show modest benefits in improving stool frequency and consistency. Results vary by individual, but they’re generally safe to try alongside other interventions.
Conclusion: Take Control of Your Digestive Health
Not being able to poop is more than just uncomfortable—it can affect your energy, mood, and overall well-being. Most cases stem from manageable lifestyle factors and respond well to hydration, fiber, movement, and routine. But when symptoms persist or warning signs appear, professional guidance is crucial. Don’t dismiss ongoing changes in your bowel habits. Early action protects your long-term health and prevents complications.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?