Constipation affects millions of people worldwide, yet it’s often dismissed as a minor inconvenience. When bowel movements become infrequent, difficult, or incomplete, daily life can be disrupted—physically and emotionally. Understanding why you can’t poop normally is the first step toward restoring digestive health. This article explores the most common causes, science-backed relief methods, warning signs that require medical attention, and practical steps to regain regularity.
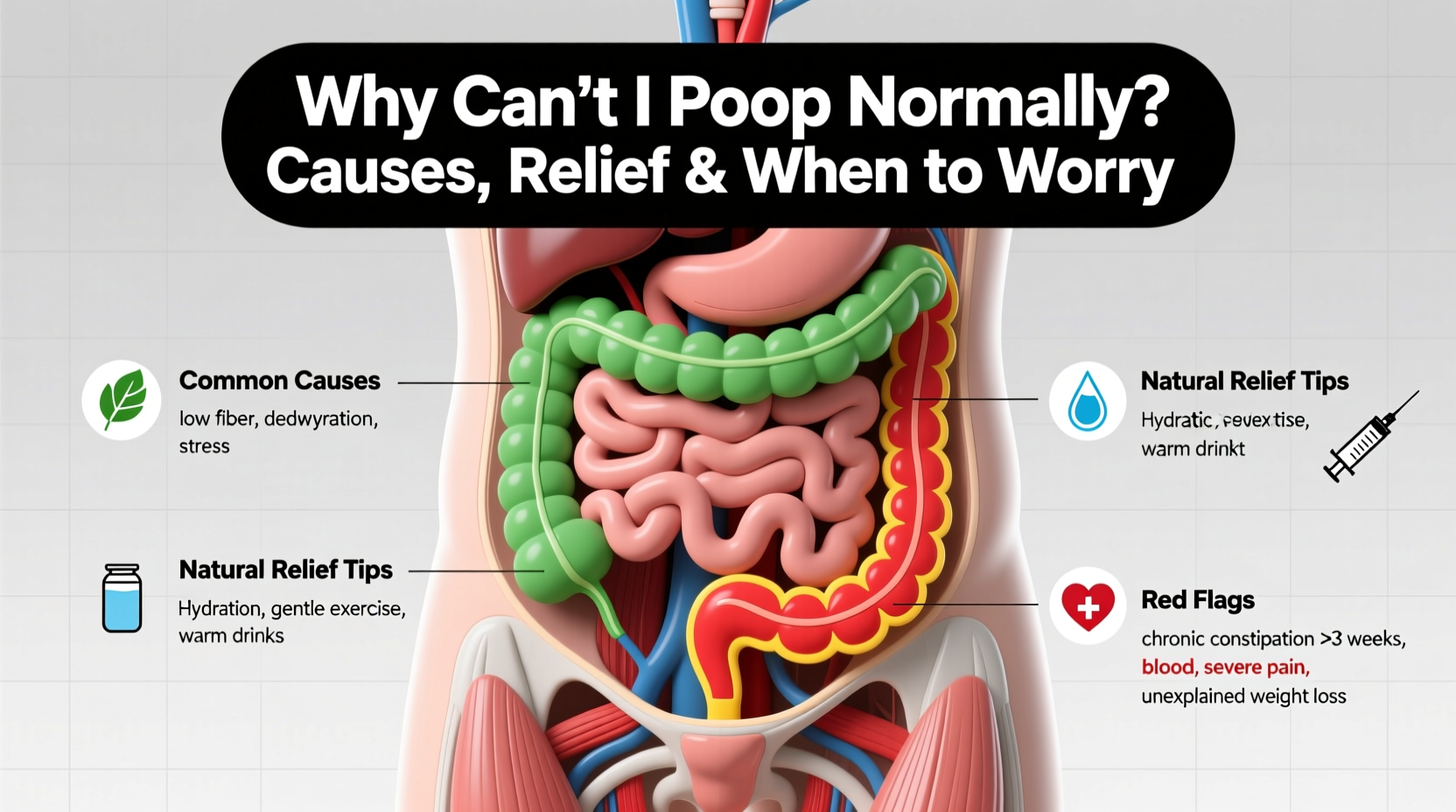
Common Causes of Difficulty Pooping
Infrequent or strained bowel movements are rarely due to a single factor. Instead, they usually result from a combination of lifestyle habits, underlying conditions, and physiological changes.
- Diet low in fiber: Fiber adds bulk to stool and helps it move smoothly through the intestines. Diets high in processed foods and low in fruits, vegetables, and whole grains are a leading cause of constipation.
- Inadequate hydration: Water softens stool. Without enough fluids, especially in high-fiber diets, stools become hard and dry, making them difficult to pass.
- Sedentary lifestyle: Physical activity stimulates intestinal contractions. A lack of movement slows digestion and contributes to sluggish bowels.
- Ignoring the urge: Regularly delaying bowel movements can weaken the body’s natural signals over time, reducing rectal sensitivity.
- Medications: Common drugs like opioids, antidepressants, antacids containing aluminum or calcium, and some blood pressure medications can slow gut motility.
- Hormonal imbalances: Conditions such as hypothyroidism, diabetes, and pregnancy alter hormone levels that affect intestinal function.
- Intestinal disorders: Irritable bowel syndrome (IBS), diverticulosis, colorectal strictures, or pelvic floor dysfunction can interfere with normal defecation.
Effective Relief Strategies for Constipation
Most cases of constipation respond well to simple lifestyle adjustments. The key is consistency and patience—changes may take 2–3 days to show results.
- Increase dietary fiber gradually: Aim for 25–30 grams per day from sources like oats, lentils, apples, broccoli, chia seeds, and prunes. Sudden increases can cause bloating, so build up slowly.
- Drink more water: Consume at least 6–8 glasses of water daily. Herbal teas like peppermint or ginger may also support digestion.
- Exercise regularly: Even 20–30 minutes of walking daily enhances colon motility and promotes timely bowel movements.
- Establish a routine: Try to go to the bathroom at the same time each day, preferably after meals when the gastrocolic reflex is strongest.
- Optimize toilet posture: Use a small footstool to elevate your knees above your hips. This straightens the anorectal angle, making evacuation easier.
| Relief Method | How It Helps | Time to Effect |
|---|---|---|
| Prune juice (4–8 oz) | Natural sorbitol draws water into the colon | 6–12 hours |
| Over-the-counter osmotic laxative (e.g., polyethylene glycol) | Retains water in stool to soften it | 24–72 hours |
| Bulk-forming fiber supplement (e.g., psyllium) | Adds volume and moisture to stool | 12–72 hours |
| Stimulant laxative (e.g., senna) | Triggers intestinal muscle contractions | 6–12 hours |
When to Worry: Red Flags That Require Medical Attention
While occasional constipation is normal, certain symptoms suggest a more serious condition and warrant prompt evaluation by a healthcare provider.
“Persistent changes in bowel habits lasting more than three weeks should never be ignored. They could indicate structural issues like colon obstruction or even malignancy.” — Dr. Alan Reyes, Gastroenterologist
Seek immediate medical advice if you experience any of the following:
- New-onset constipation after age 50
- Unintentional weight loss
- Rectal bleeding or blood in stool
- Severe abdominal pain or bloating
- Vomiting alongside inability to pass stool or gas
- Family history of colon cancer or inflammatory bowel disease
These may point to conditions such as bowel obstruction, colorectal cancer, or neurological disorders affecting gut function. Diagnostic tools like colonoscopy, imaging, or anorectal manometry may be needed.
Real-Life Example: Sarah’s Recovery from Chronic Constipation
Sarah, a 42-year-old office worker, struggled with infrequent bowel movements for over two years. She relied on stimulant laxatives weekly but felt increasingly bloated and fatigued. After consulting a gastroenterologist, she discovered she had pelvic floor dysfunction—her muscles weren’t relaxing properly during defecation.
With guidance from a pelvic floor therapist, Sarah learned proper breathing and muscle-relaxation techniques. She combined this with increased fiber, daily walks, and scheduled toilet time after breakfast. Within six weeks, her reliance on laxatives dropped, and she achieved consistent, comfortable bowel movements without straining.
This case highlights how functional issues—often invisible on scans—can profoundly impact bowel health and require specialized treatment beyond diet alone.
Step-by-Step Guide to Restoring Normal Bowel Function
Follow this five-day action plan to reset your digestive rhythm:
- Day 1: Assess current habits. Record food, water intake, and bathroom attempts. Identify low-fiber meals and dehydration patterns.
- Day 2: Add one high-fiber food at each meal (e.g., berries at breakfast, salad at lunch, roasted vegetables at dinner). Drink an extra glass of water with each.
- Day 3: Begin a daily 20-minute walk after dinner. Practice diaphragmatic breathing to reduce stress-related gut tension.
- Day 4: Set a bathroom schedule. Sit on the toilet for 10 minutes after breakfast, even if no urge arises. Use a footstool for optimal posture.
- Day 5: Evaluate progress. If no improvement, consider a gentle osmotic laxative like polyethylene glycol (Miralax) once daily, under pharmacist guidance.
Frequently Asked Questions
Is it dangerous to go several days without pooping?
For most healthy adults, going 3–4 days without a bowel movement isn’t inherently dangerous, though it may cause discomfort. However, prolonged absence of stool, especially with nausea or vomiting, could indicate a blockage and requires urgent evaluation.
Can anxiety really affect my ability to poop?
Yes. The gut and brain are closely linked via the gut-brain axis. Stress and anxiety can slow intestinal transit or cause spasms, contributing to both constipation and diarrhea. Mindfulness, breathing exercises, and therapy can improve gut symptoms.
Are enemas safe for occasional use?
Occasional use of saline or phosphate enemas is generally safe for relieving acute constipation. However, frequent use can disrupt electrolyte balance and desensitize the bowel. Always follow package instructions and avoid use if you have kidney disease or heart conditions.
Conclusion: Take Control of Your Digestive Health
Difficulty pooping is more than just an annoyance—it’s a signal from your body that something needs adjustment. Whether it’s refining your diet, moving more, or addressing deeper functional or medical issues, relief is possible with informed action. Don’t normalize chronic discomfort. Listen to your body, apply these evidence-based strategies, and know when to seek professional help. Small, consistent changes today can lead to lasting digestive wellness tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?