Struggling to have a bowel movement is more than just uncomfortable—it can disrupt your daily life and affect your overall well-being. If you've ever asked yourself, \"Why can't I poop?\" you're not alone. Constipation affects millions of people worldwide, with causes ranging from lifestyle habits to underlying medical conditions. The good news is that most cases are manageable with the right approach. Understanding why constipation occurs and how to address it effectively is the first step toward regaining digestive comfort and regularity.
Understanding Constipation: What It Really Means
Constipation isn’t just about infrequent bowel movements—it’s defined by difficulty passing stools, straining during defecation, hard or lumpy stools, a sensation of incomplete evacuation, or needing manual assistance to pass stool. While occasional constipation is normal, chronic issues (lasting more than three months) may indicate an underlying problem.
The digestive system relies on coordinated muscle contractions to move waste through the colon. When this process slows down, water is absorbed excessively from the stool, making it dry and difficult to pass. Several factors can interfere with this natural rhythm, including diet, hydration, physical activity, medications, and stress.
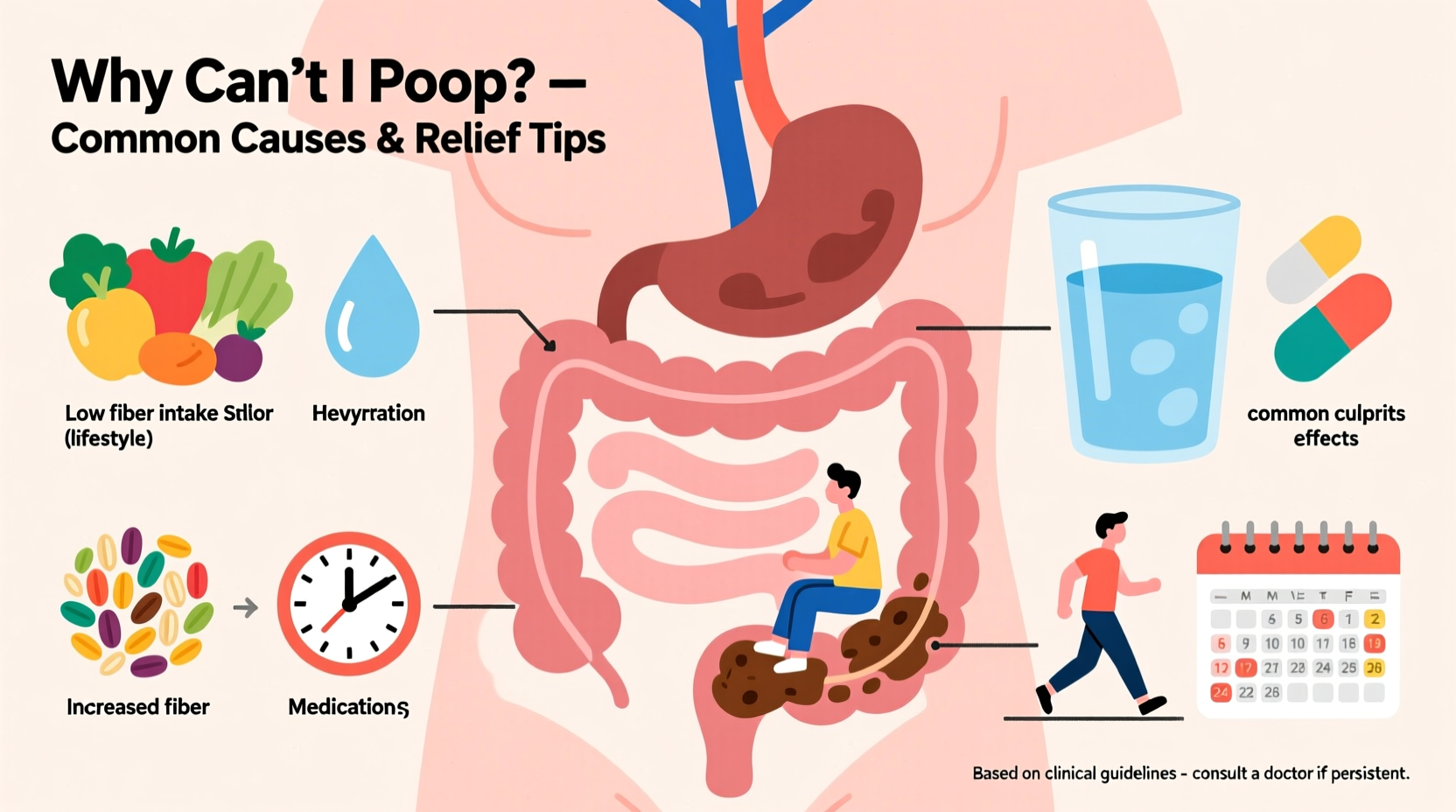
Common Causes of Constipation
Identifying the root cause of your constipation is essential for choosing the right relief strategy. Here are the most frequent contributors:
- Inadequate fiber intake: Diets low in fruits, vegetables, whole grains, and legumes reduce stool bulk and slow transit time.
- Dehydration: Not drinking enough water leads to harder stools that are difficult to pass.
- Sedentary lifestyle: Physical inactivity reduces intestinal motility, slowing digestion.
- Ignoring the urge to go: Delaying bowel movements regularly can weaken signals over time.
- Medications: Opioids, certain antidepressants, antacids containing aluminum or calcium, and iron supplements are common culprits.
- Hormonal imbalances: Conditions like hypothyroidism or diabetes can impair gut function.
- Pelvic floor dysfunction: Inability to coordinate pelvic muscles during defecation can block stool passage.
- Stress and anxiety: Mental health directly influences gut motility via the gut-brain axis.
“Chronic constipation is often multifactorial. A thorough evaluation of diet, medication use, and psychological factors is crucial.” — Dr. Lena Patel, Gastroenterologist
Natural Relief Strategies That Work
Before turning to medication, many people find significant improvement through simple lifestyle adjustments. These evidence-based methods support natural bowel function:
1. Increase Dietary Fiber Gradually
Fiber adds bulk and softness to stool. Aim for 25–30 grams per day from sources like oats, apples, pears, broccoli, lentils, and chia seeds. Introduce fiber slowly to avoid bloating or gas.
2. Hydrate Consistently
Water helps fiber do its job. Without adequate fluids, fiber can actually worsen constipation. Drink at least 6–8 glasses of water daily, more if active or in hot climates.
3. Move Your Body
Exercise stimulates colonic contractions. Even 20–30 minutes of walking daily can improve bowel regularity.
4. Establish a Bathroom Routine
Try to sit on the toilet at the same time each day, ideally 15–45 minutes after breakfast when the gastrocolic reflex is strongest. Don’t rush—give yourself time.
5. Optimize Toilet Position
Sitting upright on a standard toilet can create a kink in the rectum. Using a small footstool to elevate your knees above your hips (like a squatting position) straightens the path and eases elimination.
When to Consider Medical Treatments
If lifestyle changes don’t help within a few weeks, or if symptoms include severe pain, blood in stool, unexplained weight loss, or alternating constipation and diarrhea, consult a healthcare provider. You may need diagnostic tests or prescription treatments.
Over-the-counter options include:
| Type | How It Works | Examples | Use With Caution If... |
|---|---|---|---|
| Bulk-forming laxatives | Add fiber to soften stool | Psyllium (Metamucil), methylcellulose | You’re dehydrated or have swallowing issues |
| Osmotic laxatives | Draw water into the colon | Polyethylene glycol (MiraLAX), lactulose | You have kidney problems |
| Stimulant laxatives | Trigger intestinal contractions | Bisacodyl (Dulcolax), senna | Used long-term—they can cause dependency |
| Stool softeners | Mix water into stool to prevent hardness | Docusate sodium | Post-surgery or during recovery |
Prescription treatments like lubiprostone or linaclotide may be recommended for chronic idiopathic constipation or irritable bowel syndrome with constipation (IBS-C).
Real-Life Example: Overcoming Chronic Constipation
Sarah, a 34-year-old office worker, had struggled with constipation for over two years. Despite trying fiber supplements and occasional laxatives, she rarely had a complete bowel movement. After consulting a gastroenterologist, she discovered she had pelvic floor dysfunction—her muscles were tightening instead of relaxing during attempts to defecate.
She began working with a pelvic floor physical therapist who taught her breathing and relaxation techniques. Combined with increased water intake, daily walks, and scheduled bathroom visits, Sarah saw improvement within six weeks. By addressing the mechanical issue alongside lifestyle habits, she regained reliable bowel function without relying on medication.
Step-by-Step Guide to Immediate Relief
If you're currently unable to poop and seeking fast, safe solutions, follow this practical timeline:
- Day 1 – Morning: Drink a large glass of warm water with lemon upon waking. Follow with a high-fiber breakfast (e.g., oatmeal with prunes and flaxseed).
- Day 1 – Midday: Take a 20-minute walk. Avoid sitting for prolonged periods.
- Day 1 – Evening: Drink another 16 oz of water. Consider taking polyethylene glycol (MiraLAX) as directed if no movement has occurred.
- Day 2 – Morning: Repeat hydration and fiber routine. Spend 10 minutes on the toilet in a supported squat position after breakfast.
- Day 2 – As Needed: If still blocked, consult a doctor before using suppositories or enemas, which can provide quick relief but should not be overused.
Frequently Asked Questions
Can stress really cause constipation?
Yes. Stress activates the sympathetic nervous system, which slows digestion. Chronic anxiety or emotional strain can disrupt gut motility and alter the gut microbiome, contributing to constipation.
Is it dangerous to go several days without pooping?
While uncomfortable, going 3–4 days without a bowel movement isn’t usually dangerous for healthy individuals. However, prolonged retention can lead to fecal impaction, especially in older adults or those on certain medications. Seek medical advice if you experience severe bloating, nausea, or inability to pass gas.
Are bananas good or bad for constipation?
It depends on ripeness. Unripe (green) bananas contain resistant starch, which can be constipating. Ripe bananas, with their softer texture and higher sugar content, are generally safe and mildly helpful due to their fiber and potassium content.
Final Thoughts: Take Control of Your Digestive Health
Not being able to poop is a common yet often overlooked issue that can significantly impact quality of life. The key to relief lies in understanding your body’s signals and responding with consistent, sustainable habits. From increasing fiber and water intake to optimizing posture and managing stress, small daily actions compound into lasting improvements.
If self-care measures fail or red flags appear, don’t hesitate to seek professional guidance. Digestive health is not something to endure in silence. By taking proactive steps today, you can restore comfort, confidence, and regularity tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?