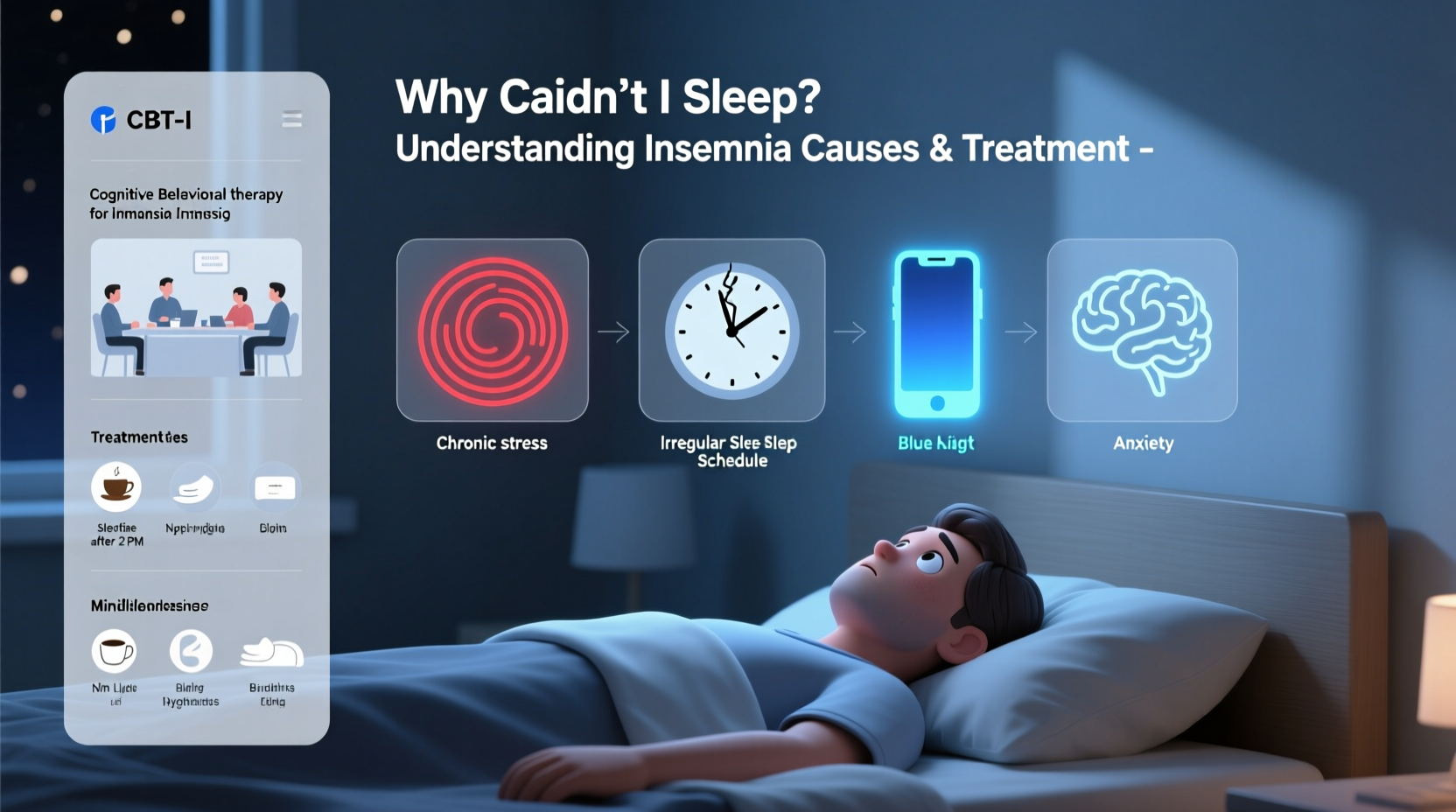
For millions of people, falling or staying asleep is not a simple act of turning off the lights. Instead, it becomes a nightly battle marked by racing thoughts, physical restlessness, and mounting frustration. Insomnia isn’t just about being tired—it affects mood, concentration, immune function, and long-term health. Understanding why you can't sleep begins with recognizing that insomnia is rarely caused by a single factor. It’s often a complex interplay of lifestyle, mental health, medical conditions, and environmental influences.
What Is Insomnia?
Insomnia is a sleep disorder characterized by difficulty falling asleep, staying asleep, or waking up too early without being able to return to sleep—despite having adequate opportunity for rest. It can be short-term (acute), lasting days or weeks, or chronic, persisting for more than three months and occurring at least three nights per week.
The consequences extend beyond fatigue. Chronic sleep deprivation increases the risk of cardiovascular disease, depression, anxiety, weight gain, and impaired cognitive performance. According to the American Academy of Sleep Medicine, nearly 30% of adults report symptoms of insomnia, while 10% suffer from chronic insomnia severe enough to impact daily functioning.
Common Causes of Insomnia
Insomnia doesn’t occur in a vacuum. Identifying root causes is essential for effective treatment. These factors typically fall into several overlapping categories:
Psychological Triggers
- Stress: Work pressure, financial worries, relationship conflicts, or major life changes can keep the mind active at night.
- Anxiety and Depression: Both are strongly linked to sleep disruption. Anxiety may cause racing thoughts, while depression often leads to early morning awakening.
- Hyperarousal: A state of heightened physiological and cognitive alertness, even during rest hours, commonly seen in people with chronic insomnia.
Lifestyle & Environmental Factors
- Poor Sleep Hygiene: Irregular sleep schedules, late-night screen use, caffeine consumption after noon, or exercising close to bedtime.
- Noise and Light Pollution: Even low levels of ambient light or sound can interfere with melatonin production and sleep onset.
- Uncomfortable Sleep Environment: Overheating, an unsupportive mattress, or room temperature above 68°F (20°C) can disrupt comfort.
Medical Conditions
- Chronic Pain: Arthritis, back pain, fibromyalgia, or migraines make it difficult to find a comfortable position.
- Respiratory Issues: Asthma, COPD, or sleep apnea can interrupt breathing and fragment sleep.
- Hormonal Imbalances: Menopause, thyroid disorders, or diabetes can alter body rhythms and trigger nighttime awakenings.
Medications and Substances
- Certain antidepressants, corticosteroids, beta-blockers, and decongestants may interfere with sleep cycles.
- Alcohol, though initially sedating, disrupts REM sleep and causes mid-sleep awakenings.
“Many patients don’t realize how much their afternoon coffee or evening phone scrolling contributes to their insomnia. Small adjustments often yield dramatic improvements.” — Dr. Lena Torres, Board-Certified Sleep Specialist
Evidence-Based Treatments for Insomnia
Treatment depends on whether insomnia is acute or chronic, and whether it's primary (not linked to another condition) or secondary (caused by an underlying issue). The most effective approaches combine behavioral strategies, medical evaluation, and lifestyle modifications.
Cognitive Behavioral Therapy for Insomnia (CBT-I)
Considered the gold standard for treating chronic insomnia, CBT-I addresses the thoughts and behaviors that perpetuate sleep difficulties. Unlike medication, its benefits are long-lasting.
| Component | Description | Expected Benefit |
|---|---|---|
| Sleep Restriction | Limits time in bed to actual sleep duration to increase sleep efficiency | Reduces fragmented sleep and strengthens bed-sleep association |
| Stimulus Control | Reinforces bed as a place only for sleep and sex | Breaks mental associations between bed and wakefulness |
| Cognitive Restructuring | Challenges unhelpful beliefs like “I’ll never sleep again” | Reduces performance anxiety around sleep |
| Relaxation Training | Includes techniques like diaphragmatic breathing and progressive muscle relaxation | Lowers physical tension and mental arousal |
Medication Options
While not recommended as a first-line or long-term solution, prescription medications such as zolpidem (Ambien), eszopiclone (Lunesta), or over-the-counter antihistamines may offer temporary relief. However, they carry risks of dependency, tolerance, and next-day drowsiness.
A Real-Life Example: Sarah’s Journey Back to Sleep
Sarah, a 42-year-old project manager, began experiencing insomnia after a high-pressure work deadline. Initially, she’d lie awake for an hour or two, worrying about unfinished tasks. Over time, this pattern worsened. She started checking the clock repeatedly, dreading bedtime, and relying on wine to wind down. After six months, her energy dropped, and she became irritable at work.
She consulted a sleep clinic and was diagnosed with chronic insomnia triggered by stress and reinforced by poor sleep habits. Her treatment plan included CBT-I sessions, eliminating alcohol before bed, setting a consistent wake-up time, and limiting screen exposure after 8 PM. Within eight weeks, Sarah reduced her sleep onset time from 90 to 25 minutes and reported feeling more focused and emotionally balanced.
Step-by-Step Guide to Improving Your Sleep
If you’re struggling to sleep, follow this structured approach to identify and address contributing factors:
- Track Your Sleep Patterns: Keep a sleep diary for two weeks noting bedtime, wake time, awakenings, caffeine intake, and mood.
- Establish a Consistent Schedule: Go to bed and wake up at the same time every day—even on weekends.
- Optimize Your Sleep Environment: Make your bedroom cool, dark, and quiet. Consider blackout curtains, white noise machines, or earplugs.
- Limit Stimulants: Avoid caffeine after 2 PM and nicotine altogether. Reduce alcohol intake, especially in the evening.
- Practice Wind-Down Rituals: Spend 30–60 minutes doing calming activities like reading, light stretching, or journaling.
- Restrict Bed Use: Only use your bed for sleep and intimacy. No phones, TV, or work.
- Seek Professional Help: If insomnia persists beyond a month despite self-help efforts, consult a doctor or sleep specialist.
Frequently Asked Questions
Can insomnia go away on its own?
Acute insomnia related to temporary stress may resolve once the situation improves. However, chronic insomnia usually requires intervention. Without treatment, it can become a self-sustaining cycle due to conditioned arousal and negative sleep beliefs.
Is it harmful to force myself to stay in bed when I can’t sleep?
Yes. Staying in bed while awake reinforces the brain’s association between the bed and wakefulness. This can deepen insomnia. It’s better to get up, move to another room, and engage in a quiet activity until you feel sleepy.
How long does CBT-I take to work?
Most people notice improvement within 4 to 6 weeks of consistent therapy. Full benefits often emerge after 8 weeks. The effects tend to last longer than those of medication because they address root causes.
Take Control of Your Sleep Tonight
Sleep is not a luxury—it’s a biological necessity. If you’ve been asking, “Why can’t I sleep?” know that answers exist, and solutions are within reach. Whether your insomnia stems from stress, poor habits, or an underlying condition, targeted changes can restore your ability to rest deeply and wake refreshed. Start by evaluating your current routines, eliminate common disruptors, and consider professional support if needed. Your mind and body depend on quality sleep to function at their best.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?