Difficulty straightening the knee is more than just a minor inconvenience—it can disrupt daily movement, limit mobility, and signal underlying joint issues. Whether the stiffness appeared suddenly after an injury or developed gradually over time, understanding the root cause is essential for recovery. This article explores the most common reasons behind knee extension limitations, backed by clinical insights, and provides actionable strategies to restore function and prevent long-term damage.
Anatomy of the Knee and Normal Extension
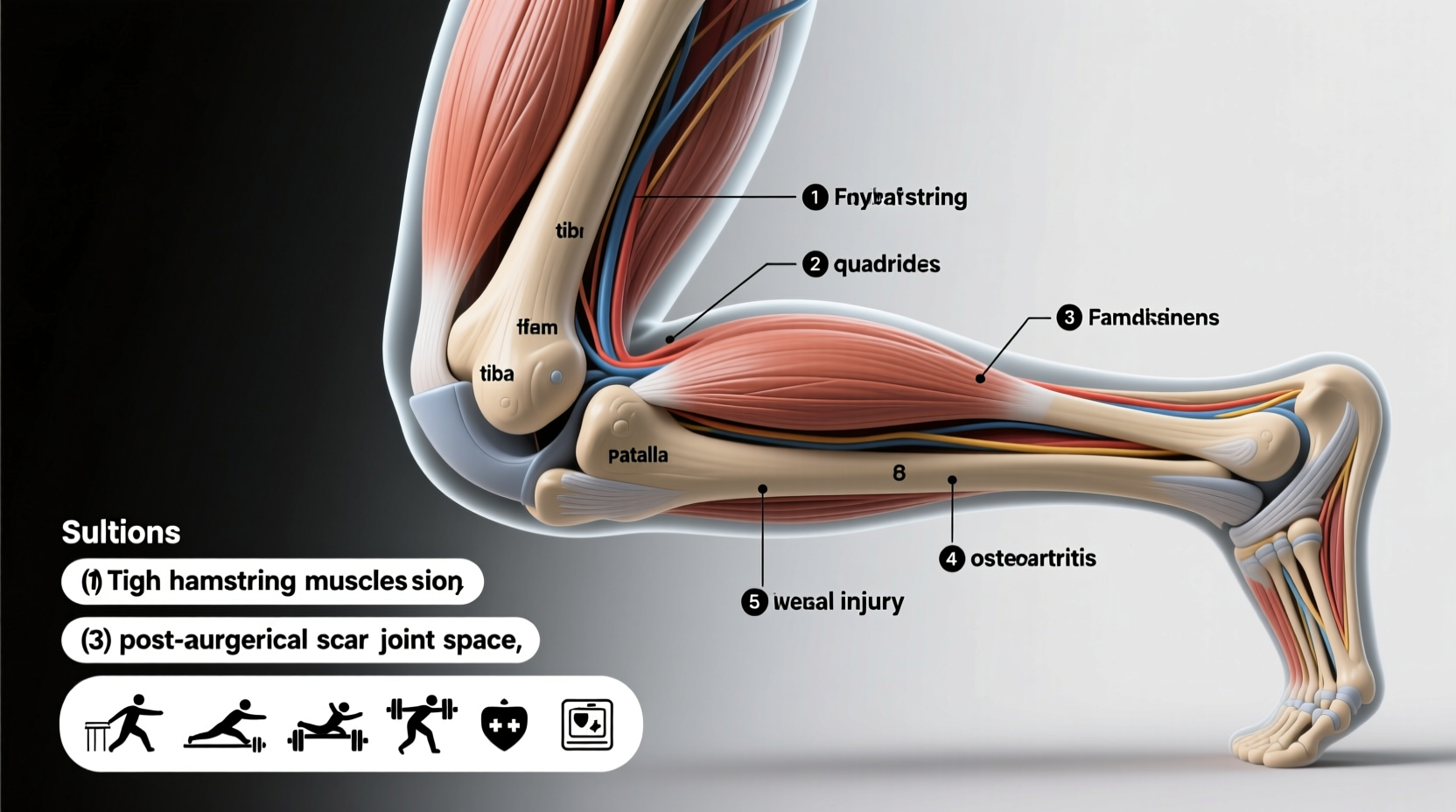
The knee joint functions as a hinge, allowing flexion (bending) and extension (straightening). Full extension—when the leg locks into a straight position—is critical for walking, standing, and balance. The quadriceps muscle, patella (kneecap), ligaments (ACL, PCL, MCL, LCL), menisci, and synovial fluid all contribute to smooth motion. When any of these components are compromised, the ability to fully extend the knee may be impaired.
Normal knee extension ranges from 0° (fully straight) to about 140° of flexion. A loss of even 5–10° of extension can alter gait patterns, increase stress on other joints, and accelerate wear in the knee cartilage. Persistent inability to straighten the knee should never be ignored.
Common Causes of Inability to Straighten the Knee
Several conditions can restrict knee extension. Identifying the cause is the first step toward effective treatment.
1. Meniscus Tears
A torn meniscus—a C-shaped cartilage cushion between the femur and tibia—is one of the most frequent culprits. A bucket-handle tear, where a portion of the meniscus flips into the joint space, can physically block full extension. This often occurs during twisting motions, especially in sports or lifting activities.
2. Anterior Cruciate Ligament (ACL) Injury
ACL tears frequently result in swelling and joint effusion (fluid buildup), which mechanically limits extension. Additionally, post-injury muscle inhibition—where the quadriceps shuts down due to pain or inflammation—can prevent full straightening even after swelling subsides.
3. Arthritis (Osteoarthritis or Rheumatoid)
Chronic joint degeneration leads to cartilage loss, bone spurs, and synovial thickening. These changes can reduce the joint’s range of motion over time. In advanced osteoarthritis, bony growths may physically obstruct extension.
4. Joint Effusion (Knee Swelling)
Excess fluid inside the joint capsule, caused by trauma, overuse, or inflammatory conditions, creates pressure that inhibits full extension. Even small amounts of fluid can disrupt normal mechanics.
5. Quadriceps Tendon or Patellar Tendon Dysfunction
Injuries or tendinopathy affecting the tendons that connect the kneecap to the shinbone or thigh muscles can impair the force needed to straighten the knee. Weakness or scarring in these structures often results in a persistent flexion contracture.
6. Post-Surgical Stiffness
After knee surgery—especially ACL reconstruction or meniscectomy—scar tissue formation (arthrofibrosis) can restrict motion. Without early and consistent rehabilitation, patients may struggle to regain full extension.
“Even a 5-degree loss of knee extension can increase patellofemoral joint stress by up to 50% during walking.” — Dr. Robert F. LaPrade, Orthopedic Knee Specialist
Diagnosis: How Doctors Identify the Cause
Accurate diagnosis begins with a thorough physical exam and imaging. Physicians assess:
- Range of motion (active and passive)
- Pain location and swelling
- Ligament stability (Lachman test, anterior drawer)
- Meniscal signs (McMurray’s test)
- Muscle strength and inhibition
Imaging tools such as MRI can detect soft tissue injuries, while X-rays reveal arthritis or loose bodies. Ultrasound may be used to evaluate tendon integrity and fluid presence.
Solutions and Treatment Approaches
Treatment depends on the underlying cause but generally follows a tiered approach—from conservative care to surgical intervention when necessary.
1. Reduce Swelling and Inflammation
For acute injuries, the R.I.C.E. protocol (Rest, Ice, Compression, Elevation) helps minimize swelling, which often restores some extension. Nonsteroidal anti-inflammatory drugs (NSAIDs) may be recommended short-term.
2. Physical Therapy and Range-of-Motion Exercises
A structured rehab program is essential. Therapists use techniques such as:
- Heel props: Lying on your back with heels elevated on a rolled towel to encourage passive extension.
- Quadriceps sets: Tightening the thigh muscle while pressing the knee down into a surface.
- Standing knee extensions: Using body weight to gently stretch the posterior capsule.
“Early mobilization after injury or surgery is key. Delaying therapy increases the risk of permanent stiffness.” — Dr. Karen Weiss, Physical Therapist and Sports Rehab Specialist
3. Manual Therapy and Joint Mobilization
Skilled therapists perform anterior glide mobilizations of the tibia to improve extension. Soft tissue work on tight hamstrings or posterior capsule structures can also enhance mobility.
4. Surgical Intervention
If mechanical blocks like meniscal tears or loose bodies are present, arthroscopic surgery may be required. In cases of severe arthrofibrosis, manipulation under anesthesia (MUA) or lysis of adhesions might be performed.
Step-by-Step Guide to Regaining Knee Extension at Home
While professional guidance is ideal, these steps can support recovery under medical supervision:
- Assess Your Baseline: Lie flat and attempt to fully straighten both legs. Note any gap under the back of the knee.
- Apply Ice (if swollen): 15–20 minutes every 2–3 hours to reduce effusion.
- Perform Heel Prop Exercises: Lie on your back with the affected leg extended. Place a rolled towel under the heel so the knee hangs slightly off the edge. Relax for 5–10 minutes, 3–5 times daily.
- Do Quad Sets: Tighten the thigh muscle and press the knee down into the floor. Hold for 5 seconds, repeat 20 times, 3 times a day.
- Use a Towel Stretch: Sit with the leg straight and loop a towel around the foot. Gently pull toes toward you to stretch the back of the knee.
- Track Progress Weekly: Measure improvement using a goniometer or smartphone app designed for joint angles.
Do’s and Don’ts Table
| Do’s | Don’ts |
|---|---|
| Keep the knee moving within pain-free range | Allow prolonged sitting with bent knees |
| Elevate the leg to reduce swelling | Ignore persistent locking or catching |
| Follow prescribed physical therapy exercises | Force the knee into extension aggressively |
| Use ice after activity if inflamed | Delay medical evaluation if symptoms persist beyond 1–2 weeks |
Real Example: Recovery After Meniscus Repair
Mark, a 38-year-old recreational soccer player, twisted his knee during a weekend game. Initially, he assumed it was a sprain, but after three days, he couldn’t stand fully upright without a noticeable bend in his right knee. An MRI revealed a bucket-handle tear of the medial meniscus. After arthroscopic repair, he began physical therapy immediately. Using heel props and quad sets, he regained full extension within four weeks. By week eight, he returned to light jogging. His therapist emphasized consistency: “Even on days when progress felt minimal, doing the exercises made the difference.”
Frequently Asked Questions
Can a stiff knee heal on its own?
Mild stiffness from minor strain or temporary swelling may improve with rest and gentle movement. However, structural issues like meniscal tears or significant scar tissue won’t resolve without targeted treatment. Ignoring persistent extension deficits can lead to chronic dysfunction.
How long does it take to regain full knee extension?
Recovery varies. Acute swelling-related stiffness may resolve in 1–2 weeks with proper care. Post-surgical or chronic contractures can take 6–12 weeks of consistent therapy. Early intervention significantly improves outcomes.
Is it bad to walk with a bent knee?
Walking with incomplete extension alters biomechanics, increasing stress on the hip, lower back, and opposite knee. Over time, this can lead to secondary pain and joint degeneration. Restoring full extension should be a priority.
Conclusion: Take Action Before It Gets Worse
The inability to straighten your knee is not something to dismiss as normal aging or minor soreness. It’s a sign that your joint mechanics are compromised. Whether due to injury, inflammation, or degeneration, timely assessment and action can prevent long-term disability. Start with simple home techniques, but don’t hesitate to consult a healthcare provider if improvement stalls. With the right approach, most people can restore full function and return to their active lives.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?