For generations, women in labor have been told not to eat once contractions begin. The rule seems strict—especially during a process that can last many hours and demands significant physical energy. Yet modern obstetrics continues to advise limited or no food intake during active labor. Understanding the reasoning behind this guidance, the evolving research, and what exceptions may exist today is essential for expectant mothers preparing for childbirth.
The restriction isn’t about discipline or outdated tradition—it’s rooted in patient safety, particularly around anesthesia risks. While practices are slowly adapting, especially for low-risk births, the core concern remains valid and widely upheld by major health organizations.
The Risk of Pulmonary Aspiration
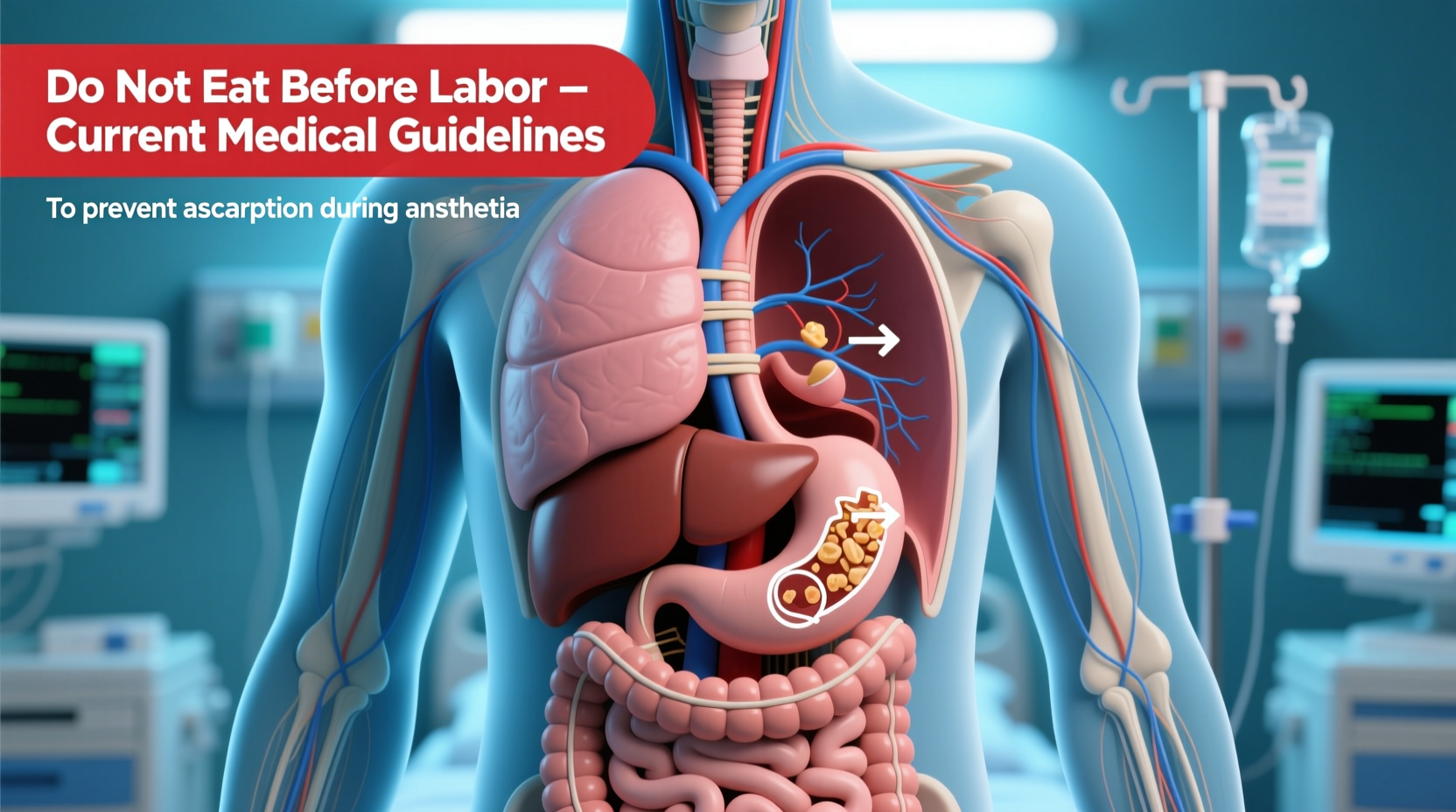
The primary reason fasting is recommended during labor is the risk of pulmonary aspiration—a rare but life-threatening condition where stomach contents enter the lungs. This becomes especially dangerous if general anesthesia is required during an emergency cesarean section.
During general anesthesia, protective reflexes like swallowing and coughing are suppressed. If the stomach is full, there's a higher chance of regurgitation while unconscious. Once vomit reaches the lungs, it can cause severe inflammation, infection, or even respiratory failure—a condition known as Mendelson’s syndrome, first described in 1946 among pregnant women undergoing anesthesia.
“Although rare, aspiration under anesthesia carries high maternal mortality. Fasting reduces gastric volume and acidity, significantly lowering this risk.” — Dr. Laura Henderson, Anesthesiologist and Maternal Safety Advocate
Pregnancy itself increases the risk. Hormonal changes slow digestion, and the growing uterus puts pressure on the stomach, making reflux more likely. Even a routine meal several hours before labor could leave substantial contents in the stomach when anesthesia is unexpectedly needed.
Current Medical Guidelines: What Major Organizations Say
Despite anecdotal stories of hospitals allowing ice chips or clear liquids, official recommendations remain cautious. Here's what leading health authorities advise:
| Organization | Guideline on Eating During Labor |
|---|---|
| American Society of Anesthesiologists (ASA) | Low-risk women may consume clear liquids (water, fruit juice without pulp, black tea, coffee, sports drinks). Solid foods discouraged. |
| Royal College of Obstetricians and Gynaecologists (RCOG) | Healthy women with uncomplicated pregnancies may have light meals early in labor. Reassessment needed as labor progresses. |
| ACOG (American College of Obstetricians and Gynecologists) | Clear liquids permitted in low-risk labor; solids not recommended due to aspiration risk. |
| World Health Organization (WHO) | Encourages freedom of movement and oral intake during labor for low-risk women. |
Note the distinction: most guidelines differentiate between *clear liquids* and *solid food*. While sipping water or broth may be acceptable, eating toast, fruit, or sandwiches is generally prohibited once active labor begins.
Who Should Avoid All Food and Drink?
Certain conditions elevate the risk of complications requiring anesthesia, making fasting non-negotiable:
- Women expecting a cesarean delivery (planned or likely)
- Those with preeclampsia or gestational diabetes
- Individuals with obesity (BMI ≥30), which increases anesthesia difficulty
- Anyone with gastrointestinal disorders affecting motility
- Patients receiving opioid pain medications, which delay gastric emptying
In these cases, even clear fluids may be restricted after a certain point. Your care team will assess your individual risk profile and guide you accordingly.
What Can You Safely Consume During Labor?
If you're low-risk and your provider permits it, not all intake is off-limits. The key is choosing items that leave the stomach quickly and don’t increase acidity.
- Water – Essential for hydration and poses no risk.
- Clear broths – Provide electrolytes and minimal residue.
- Frozen fruit bars without chunks – Can soothe nausea and offer small energy boosts.
- Sports drinks – Useful if labor is prolonged; balance sugar and electrolytes.
- Black coffee or tea (without milk) – Permitted in small amounts if tolerated.
Foods to avoid entirely include dairy products, meats, grains, nuts, and anything with fat or fiber, as these take much longer to digest—sometimes over 6–8 hours.
Real-World Scenario: A Low-Risk Birth with Flexible Intake
Maya, 29, was in her first pregnancy with no complications. Her birth plan included mobility, hydrotherapy, and the ability to eat lightly during early labor at a freestanding birthing center. Under midwife supervision, she consumed oatmeal with banana early on and later sipped coconut water and lemon tea.
When she transitioned to active labor, her midwife advised switching to ice chips and water only. Though hungry after 18 hours, Maya understood the precaution. When unexpected fetal distress arose, she required an emergency transfer and general anesthesia for a rapid C-section. Because she had followed fluid-only protocols for over six hours, her stomach was sufficiently empty, reducing anesthesia risk.
Her son was born healthy, and Maya later reflected: “I was glad I didn’t push to eat more. That final call wasn’t worth risking his safety.”
Step-by-Step: Managing Nutrition Before and During Labor
To navigate this safely and effectively, follow this timeline:
- 48 Hours Before Due Date Window: Focus on nutrient-dense meals—lean proteins, whole grains, fruits, and vegetables—to build energy reserves.
- At First Signs of Labor: Eat a light meal (e.g., toast with peanut butter, yogurt, or rice with steamed veggies) if nausea-free.
- Active Contractions Begin: Switch to clear liquids only. Pack a bottle with water, diluted juice, or electrolyte solution.
- En Route to Hospital/Birth Center: Inform staff what you’ve consumed and when. Honesty ensures proper risk assessment.
- Once Admitted: Follow facility policy. Most will allow ice chips, Popsicles, or sips of approved drinks.
Emerging Research and Changing Practices
Recent studies suggest that for low-risk women, light meals during labor do not increase complications. A 2023 Cochrane review analyzed nine trials involving over 3,000 participants and found no difference in cesarean rates, aspiration events, or neonatal outcomes between women who ate lightly and those who did not.
Despite this, widespread change has been slow. Hospitals must balance individual choice with institutional liability. Emergency readiness means preparing for worst-case scenarios—even rare ones. Until protocols evolve uniformly, most providers err on the side of caution.
FAQ
Can I eat anything if I’m having a planned C-section?
No. For scheduled cesareans under general anesthesia, fasting for at least 8 hours (including solids and most liquids) is standard. Some facilities allow clear liquids up to 2 hours before surgery—always confirm with your anesthesiologist.
Why are ice chips allowed if food isn’t?
Ice chips melt into water, leaving no particulate matter. They provide moisture and oral comfort without increasing stomach volume or acidity significantly.
Is there a safe alternative to eating for energy during long labor?
Yes. Intravenous (IV) dextrose solutions can maintain blood sugar levels. While not routine, they may be used if dehydration or hypoglycemia is a concern. Discuss options with your provider ahead of time.
Checklist: Preparing for Labor Without Compromising Safety
- ✔ Discuss your nutrition plan with your OB or midwife during prenatal visits
- ✔ Pack approved clear liquids (e.g., electrolyte powders, herbal teas)
- ✔ Eat a balanced, easily digestible meal at the first signs of labor
- ✔ Keep a log of food and drink intake (time and amount)
- ✔ Stay hydrated with small, frequent sips
- ✔ Follow hospital or birth center policies upon arrival
Conclusion
The rule against eating during labor persists not out of rigidity, but out of deep commitment to maternal safety. While new evidence supports greater flexibility for low-risk individuals, the stakes of anesthesia complications remain too high to abandon caution entirely. By understanding the reasons behind the guideline, preparing nutritionally in advance, and respecting real-time medical advice, women can approach childbirth with both empowerment and prudence.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?