The liver is one of the most vital organs in the human body, quietly performing hundreds of essential functions every day. Unlike some organs, the liver cannot be replaced by machines or dialysis when it fails. Without a functioning liver, survival is impossible beyond a few days. This isn’t just due to its size or location—it’s because of the sheer volume and complexity of processes it manages. From detoxifying harmful substances to producing life-sustaining proteins, the liver operates as the body’s biochemical command center. When liver function fails, multiple systems collapse rapidly, leading to life-threatening complications.
The Liver’s Critical Functions
The liver performs over 500 known physiological tasks, many of which are irreplaceable. These include:
- Detoxification: Filters toxins, drugs, alcohol, and metabolic waste from the bloodstream.
- Protein synthesis: Produces albumin (which maintains blood volume) and clotting factors necessary for wound healing.
- Metabolism regulation: Processes carbohydrates, fats, and proteins into usable energy sources.
- Bile production: Creates bile to aid in fat digestion and absorption of fat-soluble vitamins (A, D, E, K).
- Storage: Stores glycogen (for energy), iron, and key vitamins.
- Immune support: Houses immune cells that help clear bacteria from the blood, especially from the digestive tract.
When these functions falter, the consequences are systemic. There is no artificial device capable of replicating this breadth of activity—making the liver non-negotiable for survival.
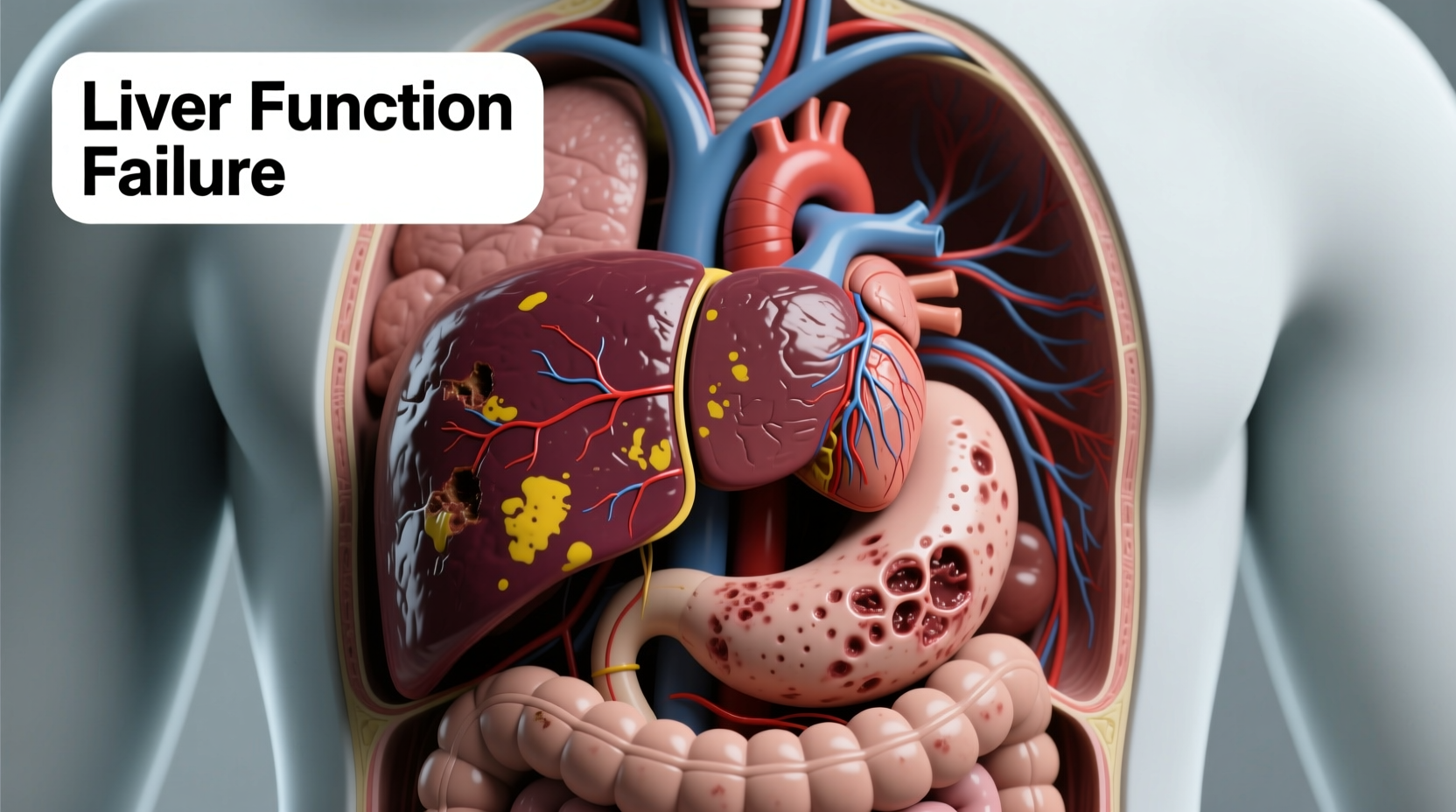
What Happens During Liver Function Failure?
Liver failure occurs when large portions of the liver become damaged and can no longer function properly. It can develop acutely (over days or weeks) or chronically (over years). Acute liver failure is particularly dangerous because it strikes without warning and progresses rapidly.
As liver cells die, critical processes begin to shut down:
- Toxins like ammonia accumulate in the blood, affecting brain function and causing hepatic encephalopathy—confusion, drowsiness, and eventually coma.
- Clotting factors diminish, increasing the risk of uncontrollable bleeding.
- Fluid leaks into the abdomen (ascites) and legs (edema) due to low albumin levels.
- Bilirubin builds up, leading to jaundice—yellowing of the skin and eyes.
- Infections become more frequent due to weakened immunity.
Without intervention, multi-organ failure follows. The kidneys often fail next (hepatorenal syndrome), and respiratory distress may occur due to fluid accumulation and metabolic imbalance.
Stages of Liver Failure Progression
| Stage | Symptoms | Reversibility |
|---|---|---|
| Compensated Cirrhosis | Fatigue, mild swelling, occasional nausea | Potentially reversible with treatment |
| Decompensated Cirrhosis | Jaundice, ascites, variceal bleeding, confusion | Limited recovery; transplant often needed |
| Acute Liver Failure | Rapid mental decline, coagulopathy, hypoglycemia | Life-threatening; requires ICU care and possible transplant |
Common Causes of Liver Failure
Liver failure doesn’t happen in isolation. It’s usually the end result of prolonged damage from various sources:
- Alcohol-related liver disease: Chronic heavy drinking leads to fatty liver, hepatitis, and cirrhosis.
- Viral hepatitis: Hepatitis B and C are leading global causes of chronic liver damage.
- Non-alcoholic fatty liver disease (NAFLD): Linked to obesity, insulin resistance, and metabolic syndrome.
- Drug-induced injury: Overdose of acetaminophen (Tylenol), certain antibiotics, or herbal supplements.
- Autoimmune conditions: Autoimmune hepatitis where the immune system attacks liver cells.
- Genetic disorders: Hemochromatosis (iron overload), Wilson’s disease (copper accumulation).
Early detection is crucial. Many people remain asymptomatic until significant damage has occurred.
“Once liver function drops below 15–20%, the body can no longer compensate. That’s when we see rapid clinical deterioration.” — Dr. Rajiv Mehta, Hepatologist at Boston General Hospital
Real-Life Example: A Case of Acetaminophen Overdose
Consider the case of Maria, a 34-year-old woman who took high doses of acetaminophen for several days to manage chronic back pain. She wasn’t aware that exceeding the recommended daily limit (4,000 mg) could be fatal. Within 72 hours, she developed nausea, abdominal pain, and confusion. By the time she reached the emergency room, her liver enzymes were 50 times above normal. Despite aggressive treatment with N-acetylcysteine (an antidote), her liver continued to fail. She was listed for an urgent transplant and received a donor liver after five days on life support. Her recovery was slow but complete—thanks to timely intervention.
Maria’s story illustrates how quickly liver failure can escalate, even from seemingly harmless medications. It also highlights the narrow window for effective treatment.
Step-by-Step: What to Do If Liver Failure Is Suspected
If liver dysfunction is suspected, immediate action can save lives. Follow this timeline:
- Recognize early signs: Persistent fatigue, loss of appetite, dark urine, or unexplained bruising.
- Seek medical evaluation: Blood tests (liver function panel, INR, bilirubin) and imaging (ultrasound, elastography).
- Stop harmful substances: Discontinue alcohol, unnecessary medications, or supplements under medical guidance.
- Treat underlying cause: Antivirals for hepatitis, corticosteroids for autoimmune disease, or antidotes for poisoning.
- Assess transplant eligibility: In advanced cases, referral to a transplant center is urgent.
In acute settings, patients may require intensive care monitoring, mechanical ventilation, or dialysis if kidney function declines.
Prevention Checklist
You can significantly reduce your risk of liver failure by taking proactive steps:
- ✔ Get vaccinated against hepatitis A and B.
- ✔ Limit alcohol consumption or abstain completely if at risk.
- ✔ Maintain a healthy weight to prevent NAFLD.
- ✔ Read medication labels and avoid combining drugs that stress the liver.
- ✔ Avoid sharing needles or personal items like razors.
- ✔ Schedule regular checkups if you have diabetes, high cholesterol, or a family history of liver disease.
Frequently Asked Questions
Can you live with only part of your liver?
Yes—and this is one of the liver’s remarkable features. The liver can regenerate. Even if 70% is removed surgically, it can regrow to full size within weeks, provided the remaining tissue is healthy. However, regeneration does not occur in advanced cirrhosis or acute failure.
Is liver failure always permanent?
Not always. Acute liver failure caused by drug overdose or viral infection may be reversible if treated early. Chronic liver failure due to cirrhosis is generally irreversible, though progression can be slowed with proper management.
How long can someone survive without a functioning liver?
Without any liver function, survival is limited to a few days. Even with intensive care, death typically occurs within 1–2 weeks unless a transplant is performed. The body simply cannot sustain basic metabolic balance without hepatic support.
Conclusion: Protect Your Liver Like Your Life Depends on It—Because It Does
The liver is silent but indispensable. Its ability to work behind the scenes means problems often go unnoticed until it's too late. Yet, with informed choices and preventive care, most liver diseases are avoidable or manageable. Understanding the risks, recognizing symptoms early, and seeking prompt medical help can make the difference between life and death.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?