Calluses are thickened areas of skin that develop in response to repeated pressure or friction. While they’re a natural protective mechanism, they can become uncomfortable, unsightly, or even painful if left unchecked. The feet are especially prone to callus formation due to the constant weight-bearing and contact with shoes and surfaces. Understanding why calluses form—and how to prevent them—is essential for maintaining foot health, comfort, and mobility.
What Are Calluses and How Do They Form?
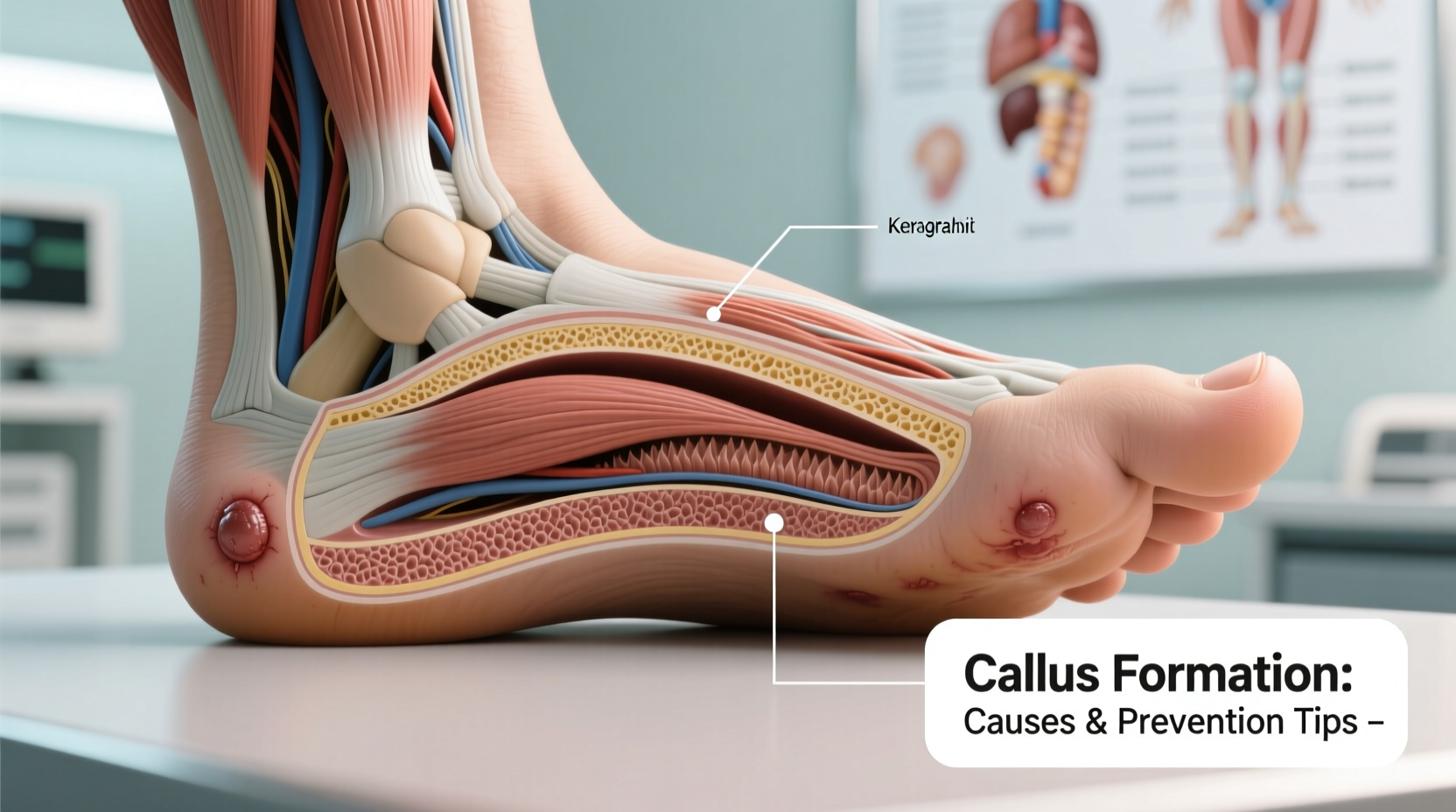
Calluses are patches of hard, dead skin that accumulate when the body tries to protect underlying tissue from damage. Unlike corns, which are smaller and often have a central core, calluses tend to be broader, flatter, and less defined. They typically appear on the soles of the feet, especially under the heels, balls of the feet, or along the sides of toes.
The process begins when repeated mechanical stress—such as walking, standing, or wearing poorly fitting shoes—triggers the skin to produce extra layers of keratin, a tough protein that strengthens the outer layer. Over time, this buildup forms a dense, hardened area. While mild calluses may not cause discomfort, thicker ones can crack, split, or press on nerve endings, leading to pain.
“Calluses are the body’s way of saying it’s under too much pressure. Ignoring them can lead to deeper skin issues or changes in gait.” — Dr. Lena Patel, Podiatrist and Foot Health Specialist
Common Causes of Foot Calluses
Several factors contribute to the development of calluses. Identifying these causes is the first step toward effective prevention.
- Poorly Fitting Footwear: Shoes that are too tight squeeze the toes, while loose shoes cause the foot to slide, increasing friction.
- High-Heeled or Narrow-Toe Shoes: These shift body weight forward, increasing pressure on the ball of the foot.
- Barefoot Walking on Hard Surfaces: Regularly walking without protection exposes the feet to excessive friction.
- Abnormal Gait or Foot Structure: Conditions like flat feet, high arches, or bone misalignments alter pressure distribution.
- Lack of Sock Use: Going barefoot inside shoes reduces cushioning and increases rubbing.
- Occupational Hazards: Jobs requiring long periods of standing or walking (e.g., nursing, retail) increase risk.
Effective Prevention Tips to Avoid Calluses
Preventing calluses doesn’t require drastic changes—it’s about consistent, mindful habits. Here’s how to reduce the risk:
- Wear Properly Fitted Shoes: Ensure there’s enough room in the toe box and that heels don’t slip. Get your feet measured regularly, as size can change with age.
- Choose Supportive Footwear: Look for shoes with cushioned insoles, arch support, and shock-absorbing soles.
- Use Protective Padding: Apply moleskin or gel pads to high-friction zones like heels or toes.
- Wear Moisture-Wicking Socks: Cotton or synthetic blends help reduce sweat and friction.
- Limit Barefoot Activity: Even indoors, walking barefoot on hard floors adds cumulative stress.
- Maintain Foot Hygiene: Wash and dry feet daily, then apply a moisturizer to keep skin supple.
Dos and Don’ts of Callus Prevention
| Do | Don't |
|---|---|
| Trim toenails regularly to prevent toe pressure | Wear flip-flops or sandals for long walks |
| Use pumice stone weekly after bathing | Soak feet excessively, which can weaken skin |
| Replace worn-out shoes every 6–12 months | Cut calluses with sharp objects at home |
| Apply urea-based creams for dry skin | Ignore early signs of redness or thickening |
Step-by-Step Guide to Managing Early Callus Formation
If you notice rough patches beginning to form, taking action early can prevent full-blown calluses. Follow this routine weekly:
- Soak Feet: For 10–15 minutes in warm (not hot) water with Epsom salt to soften skin.
- Gently Exfoliate: Use a pumice stone or foot file in circular motions to remove dead skin. Don’t scrub aggressively.
- Rinse and Dry Thoroughly: Pat feet dry, especially between toes, to prevent fungal growth.
- Moisturize: Apply a foot cream containing urea, lactic acid, or shea butter.
- Protect: Wear soft socks overnight to lock in moisture and consider using silicone toe sleeves during the day.
Real-Life Example: A Retail Worker’s Experience
Sophia, a 34-year-old store associate, spent eight hours a day on her feet. After several months, she noticed thick, yellow patches forming under both heels. At first, she ignored them—until one cracked deeply and became painful. She visited a podiatrist who diagnosed chronic pressure-induced calluses due to rigid work shoes and lack of supportive insoles.
Following a simple care plan—switching to cushioned shoes, using heel pads, and exfoliating twice weekly—her calluses softened within four weeks. “I didn’t realize how much my shoes were hurting me,” she said. “Now I check my feet every Sunday night. It’s part of my self-care routine.”
When to See a Professional
While most calluses can be managed at home, certain situations require medical attention:
- Pain that interferes with walking or daily activities
- Signs of infection (redness, swelling, pus)
- Calluses in people with diabetes or poor circulation
- Recurring calluses despite preventive measures
A podiatrist can safely debride thick calluses, recommend orthotics, or address biomechanical issues contributing to pressure points. Never attempt to cut or shave calluses yourself—this can lead to infections or injury, especially for individuals with compromised immune systems.
Frequently Asked Questions
Can calluses go away on their own?
Yes, if the source of friction or pressure is removed, calluses will gradually thin and disappear over weeks or months. Regular exfoliation and moisturizing speed up the process.
Are calluses contagious?
No, calluses are not caused by viruses and cannot spread from person to person. This distinguishes them from warts, which may look similar but are viral in origin.
Is it safe to use callus removers with salicylic acid?
Over-the-counter pads or liquids containing salicylic acid can be effective, but should be used with caution. Avoid using them if you have diabetes or sensitive skin, and never apply to broken skin.
Final Thoughts and Action Plan
Calluses are more than a cosmetic concern—they’re signals from your body that something needs adjustment. Whether it’s your footwear, walking habits, or foot care routine, small changes can make a big difference in preventing discomfort and long-term damage.
Start today: inspect your feet, evaluate your shoes, and commit to a simple weekly foot maintenance habit. Your feet carry you through life—give them the care they deserve.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?