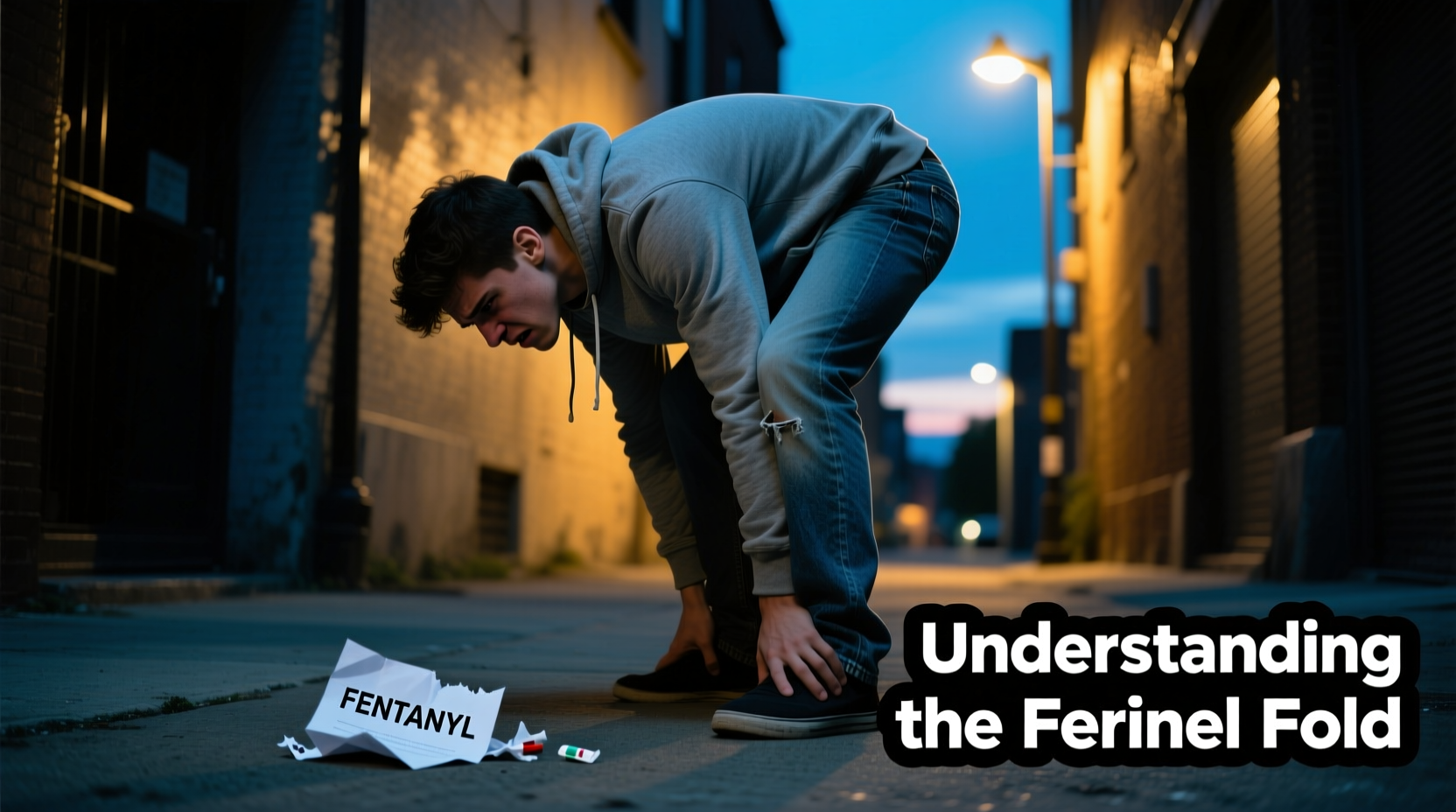
The term \"fentanyl fold\" has emerged in public health discussions, emergency medicine, and harm reduction circles to describe a distinct posture observed in individuals under the influence of fentanyl: a forward-bent stance, often with the head dropped toward the chest, arms slack, and minimal responsiveness. This physical presentation is more than a casual observation—it reflects the intense physiological effects of one of the most potent synthetic opioids available. Understanding why fentanyl users frequently adopt this posture requires examining the drug’s impact on the central nervous system, respiratory function, and muscular control.
Fentanyl, estimated to be 50 to 100 times more potent than morphine, binds rapidly to mu-opioid receptors in the brain, producing powerful analgesia and euphoria. However, it also depresses vital autonomic functions, including breathing and motor coordination. The \"fentanyl fold\" is not merely behavioral; it is a visible manifestation of profound neurological suppression. Recognizing this posture can be critical for bystanders, first responders, and healthcare providers in identifying overdose situations and initiating life-saving interventions.
The Neurological Basis of the Fentanyl Fold
When fentanyl enters the bloodstream, it quickly crosses the blood-brain barrier and activates opioid receptors responsible for pain modulation, reward, and autonomic regulation. One of the most immediate effects is the suppression of the brainstem’s respiratory centers, leading to slowed or shallow breathing—a condition known as respiratory depression. Concurrently, the drug disrupts normal muscle tone and postural control.
The forward-bending posture seen in many users results from a combination of factors:
- Muscle relaxation: Fentanyl induces generalized skeletal muscle relaxation, particularly in the neck, back, and core stabilizers. Without adequate support from these muscles, the body collapses into a slumped position.
- Sedation: Users experience rapid onset of drowsiness, often progressing to nodding off. In this semi-conscious state, maintaining upright posture becomes physically impossible.
- Reduced proprioception: The brain's ability to sense body position in space is impaired, making coordinated movement difficult and balance unstable.
This triad of effects creates a predictable physical presentation: the individual may sit or stand but slowly slump forward, chin dropping toward the chest, arms hanging limply. In severe cases, they may collapse entirely, appearing unresponsive.
“Opioids like fentanyl don’t just dull pain—they silence entire networks in the brain responsible for staying awake, breathing, and holding yourself upright.” — Dr. Lena Patel, Emergency Medicine Physician and Addiction Specialist
Respiratory Depression and Postural Collapse
The link between respiration and posture is often overlooked, but the two are deeply interconnected. Breathing relies on the diaphragm and intercostal muscles, which require stable trunk support. When fentanyl suppresses both respiratory drive and postural musculature, the body defaults to the path of least resistance: folding forward.
In this bent-over position, the chest cavity is compressed, further restricting lung expansion. This creates a dangerous feedback loop: reduced oxygen intake worsens sedation, which deepens respiratory depression. The posture itself can exacerbate hypoxia, increasing the risk of brain injury or cardiac arrest.
Case Study: Overdose Recognition in Public Spaces
In downtown Seattle, a security guard at a transit station noticed a man slumped on a bench, head nearly touching his knees, breathing irregularly. At first glance, he appeared to be sleeping. But when the guard called his name and received no response, he recognized the signs of opioid intoxication. Using training from a local harm reduction program, he administered naloxone (Narcan) via nasal spray.
Within three minutes, the man gasped, sat up, and became alert. Paramedics arrived shortly after and confirmed the incident as a non-fatal fentanyl overdose. The guard later said he wouldn’t have intervened if not for learning about the “fentanyl fold” during a community workshop. This case illustrates how recognizing this specific posture can mean the difference between life and death.
Common Misinterpretations and Risks
One of the most dangerous aspects of the fentanyl fold is that it is often misinterpreted. Bystanders may assume the person is simply tired, intoxicated by alcohol, or experiencing homelessness-related fatigue. Law enforcement officers might view the individual as non-compliant or resisting arrest when, in reality, they are neurologically incapacitated.
A study published in the Journal of Urban Health found that nearly 40% of witnessed overdoses in public spaces were not reported immediately due to misidentification of symptoms. The bent-forward posture was frequently mistaken for loitering or mental illness rather than medical distress.
To address this, public awareness campaigns now emphasize the visual cues of opioid overdose, with the fentanyl fold being a key identifier. Training materials for police, EMTs, and shelter staff include images and descriptions of this posture to improve early recognition.
Do’s and Don’ts When Encountering Someone in the Fentanyl Fold
| Action | Recommendation |
|---|---|
| Check responsiveness | DO tap the shoulder and shout their name. |
| Assess breathing | DO look for slow, shallow, or absent breaths. |
| Administer naloxone | DO use Narcan if available and suspect opioid involvement. |
| Leave them alone | DON’T assume they’re just sleeping it off. |
| Wait for symptoms to worsen | DON’T delay action—respiratory failure can occur within minutes. |
| Restrain or shake violently | DON’T use force; it won’t reverse overdose and may cause injury. |
Prevention and Harm Reduction Strategies
While the fentanyl fold is a symptom of acute intoxication, addressing the root causes requires systemic harm reduction efforts. These include expanding access to naloxone, promoting supervised consumption sites, and improving addiction treatment availability.
For individuals who use drugs, education about safer practices can reduce the likelihood of reaching this level of impairment. Some effective strategies include:
- Never using alone—have someone present who can call for help or administer naloxone.
- Starting with a small test dose, especially when drug potency is unknown. Carrying naloxone at all times.
- Using fentanyl test strips to detect the presence of the drug in other substances.
- Engaging with outreach programs that offer counseling and medical referrals.
Frequently Asked Questions
Is the fentanyl fold always a sign of overdose?
Not necessarily. Some users may exhibit this posture during heavy intoxication without meeting full criteria for overdose. However, it is a strong warning sign of impending respiratory depression and should be treated as a medical emergency until evaluated by professionals.
Can someone recover from the fentanyl fold without intervention?
Possibly, but it’s extremely risky. Even if the person regains consciousness, they remain vulnerable to sudden respiratory arrest. Unsupervised recovery increases the chance of fatal outcomes. Medical evaluation is strongly recommended.
Does the fentanyl fold only happen with pure fentanyl?
No. Most cases involve fentanyl mixed with other drugs like heroin, cocaine, or counterfeit pills. Because fentanyl is often undetected by users, even those not intending to consume it may experience the fold due to contamination.
Conclusion: A Call for Compassion and Action
The fentanyl fold is more than a physical stance—it’s a silent cry for help, a visible signal of a national crisis unfolding in plain sight. Recognizing this posture empowers communities to respond swiftly and humanely. It challenges us to see beyond stigma and treat substance use disorder as the public health issue it is.
Every person exhibiting the fentanyl fold deserves dignity, immediate care, and access to long-term support. Whether you're a passerby, a service provider, or a policymaker, your awareness can save lives. Learn the signs, carry naloxone, and advocate for compassionate solutions. The next person you see bent over might not just be struggling with a drug—they might be fighting for their life.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?