It’s a familiar sensation: you rise from sitting or lying down, and the room seems to tilt. Your vision may blur, your head spins, and for a few seconds, you feel unsteady. While occasional dizziness upon standing is common and usually harmless, frequent or severe episodes can signal an underlying health issue. Understanding why this happens—and knowing when it's time to be concerned—can help protect your long-term well-being.
This sudden dizziness, medically known as orthostatic hypotension or postural hypotension, occurs when blood pressure drops rapidly upon changing positions. The brain receives less oxygen-rich blood, triggering symptoms like lightheadedness, fainting, or blurred vision. Though often brief, these episodes shouldn’t be ignored if they occur regularly or are accompanied by other warning signs.
What Causes Dizziness When Standing Up Suddenly?
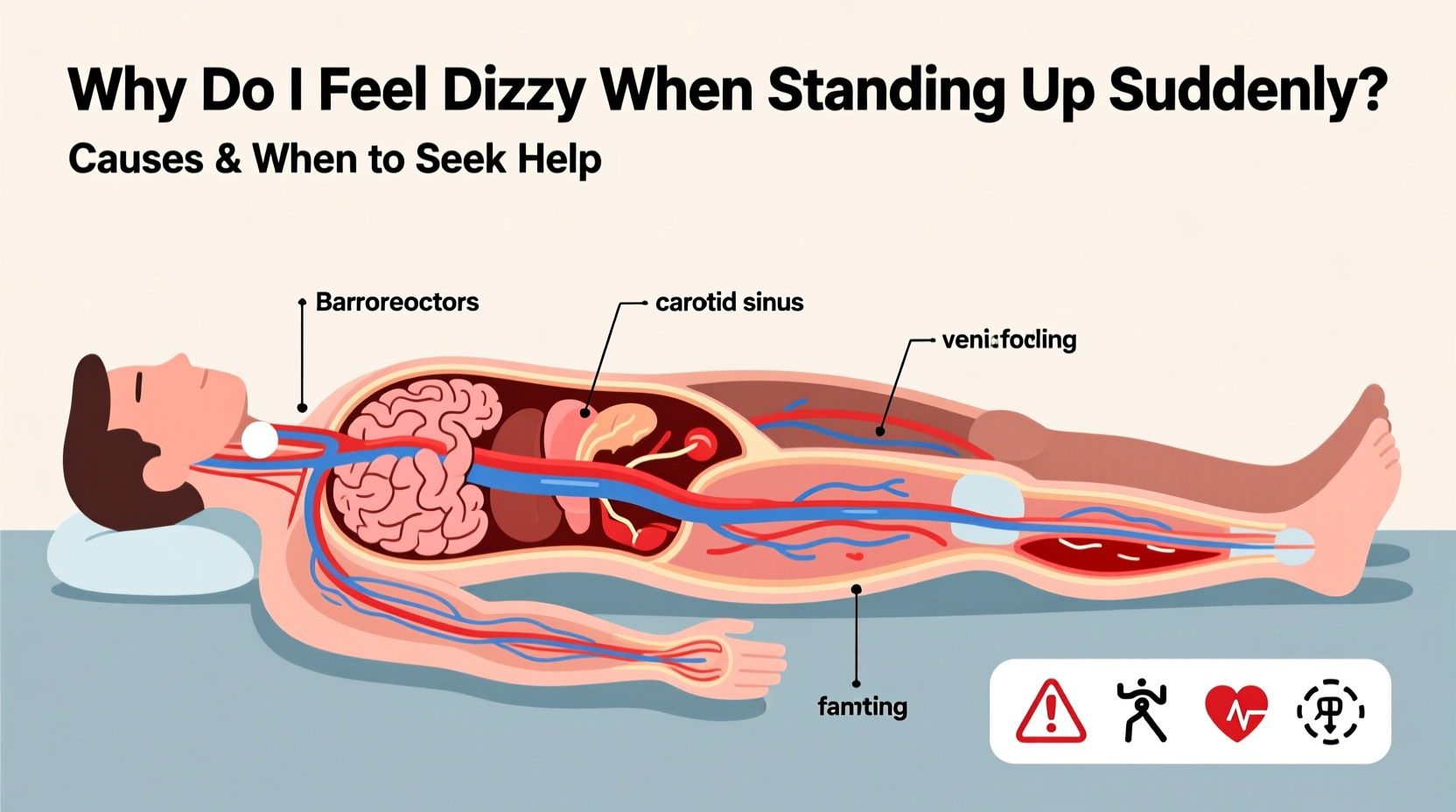
The human body maintains stable blood pressure through a complex system involving the heart, blood vessels, and nervous system. When you stand, gravity pulls blood downward into your legs and abdomen. To compensate, your autonomic nervous system signals your heart to beat faster and your blood vessels to constrict, ensuring adequate blood flow to the brain.
When this system falters—even slightly—blood pressure dips, leading to dizziness. Several factors can disrupt this balance:
- Dehydration: Low fluid volume reduces blood volume, making it harder to maintain pressure.
- Medications: Diuretics, blood pressure drugs, antidepressants, and Parkinson’s medications can affect circulation.
- Aging: Blood vessel elasticity declines with age, and the autonomic response slows.
- Prolonged bed rest: Inactivity weakens cardiovascular responsiveness.
- Heart conditions: Arrhythmias, heart valve problems, or heart failure impair blood output.
- Nervous system disorders: Diabetes-related nerve damage (autonomic neuropathy), Parkinson’s disease, or multiple system atrophy interfere with blood pressure regulation.
Common Triggers and Risk Factors
Dizziness upon standing isn’t always a sign of illness. Certain everyday behaviors and conditions increase the likelihood:
1. Dehydration and Electrolyte Imbalance
Sweating, diarrhea, vomiting, or insufficient water intake reduce blood volume. Even mild dehydration can trigger dizziness, especially in hot environments or after exercise.
2. Medication Side Effects
Over 500 medications list orthostatic hypotension as a potential side effect. These include:
- Beta-blockers and calcium channel blockers (for high blood pressure)
- Alpha-blockers (used for enlarged prostate)
- Tricyclic antidepressants and antipsychotics
- Opioids and sedatives
3. Postprandial Hypotension
Some people experience dizziness 30–75 minutes after eating, especially large meals. Blood diverts to the digestive tract, lowering supply to the brain. This is more common in older adults and those with autonomic dysfunction.
4. Pregnancy
In early pregnancy, hormonal changes relax blood vessels, which can lower blood pressure. Combined with increased blood volume demands, this may cause temporary dizziness when standing quickly.
5. Anemia
Low red blood cell count reduces oxygen delivery. When combined with positional changes, even minor drops in cerebral perfusion can cause lightheadedness.
“Orthostatic hypotension is not a diagnosis but a symptom—a clue that something in the cardiovascular or neurological system needs evaluation.” — Dr. Lena Torres, Neurologist & Autonomic Specialist
When to Worry: Red Flags That Require Medical Attention
Occasional, fleeting dizziness when rising too fast is normal. But certain patterns suggest a need for professional assessment:
| Symptom | Normal Occurrence | When to Seek Help |
|---|---|---|
| Dizziness duration | 1–5 seconds | Lasts more than 10–15 seconds or leads to near-fainting |
| Frequency | Once in a while | Multiple times per week or daily |
| Associated symptoms | None or mild lightheadedness | Chest pain, palpitations, confusion, slurred speech, or weakness |
| History of falls | No | Yes—especially if resulting in injury |
| Underlying condition | None | Diabetes, Parkinson’s, heart disease, or stroke history |
If you experience any of the following, consult a healthcare provider promptly:
- Fainting (syncope) or near-fainting spells
- Dizziness that worsens over time
- Unexplained fatigue or cognitive fog
- Trouble regulating body temperature or sweating
- Double vision, difficulty speaking, or limb weakness (possible stroke signs)
Step-by-Step Guide to Managing and Preventing Episodes
You can reduce the frequency and severity of dizziness when standing with simple lifestyle adjustments. Follow this practical sequence:
- Hydrate consistently: Aim for 6–8 glasses of water daily. Increase intake in heat or during illness.
- Rise gradually: After waking, sit on the edge of the bed for 30 seconds before standing.
- Stay active: Regular aerobic exercise improves circulation and vascular tone.
- Review medications: Ask your doctor if any prescriptions could contribute to low blood pressure.
- Monitor symptoms: Keep a log of when dizziness occurs, its duration, and triggers.
- Elevate your head at night: Use an extra pillow to reduce nighttime fluid shifts.
- Avoid large carbohydrate-heavy meals: Opt for smaller, balanced meals to prevent postprandial drops.
- Wear compression stockings: These help push blood back toward the heart and reduce pooling in the legs.
Real-Life Example: Recognizing a Silent Warning
Maria, a 68-year-old retired teacher, began noticing she felt “wobbly” every morning when getting out of bed. At first, she dismissed it as aging. But within two months, the dizziness lasted longer, and she nearly fell twice while walking to the kitchen.
Concerned, she visited her primary care physician. Blood tests revealed mild anemia, and a tilt-table test confirmed significant orthostatic hypotension. Further investigation uncovered early-stage autonomic neuropathy linked to undiagnosed type 2 diabetes.
With better glucose control, hydration strategies, and compression socks, Maria’s symptoms improved dramatically. Her case highlights how seemingly minor dizziness can be an early indicator of systemic disease.
Do’s and Don’ts: Quick Reference Checklist
To stay safe and minimize risk, follow this actionable checklist:
| Do’s | Don’ts |
|---|---|
| Drink water throughout the day | Stand up immediately after lying down |
| Move slowly when changing positions | Ignore repeated dizziness or near-fainting |
| Use support (like a wall or furniture) when rising | Consume excessive alcohol, which dilates blood vessels |
| Track symptoms in a journal | Stop prescribed medications without consulting your doctor |
| Wear compression garments if advised | Exercise in extreme heat or humidity |
FAQ: Common Questions About Sudden Dizziness
Can anxiety cause dizziness when standing up?
Anxiety doesn’t directly cause orthostatic hypotension, but it can amplify symptoms. Rapid breathing (hyperventilation) during anxious episodes alters blood CO₂ levels, potentially worsening lightheadedness. However, true positional dizziness stems from blood pressure dysregulation, not psychological causes alone.
Is it dangerous to feel dizzy every time I stand?
Not always, but frequent episodes increase fall risk, especially in older adults. Over time, recurrent drops in cerebral perfusion may contribute to cognitive decline. Persistent dizziness warrants medical evaluation to rule out heart, neurological, or metabolic issues.
How is orthostatic hypotension diagnosed?
Doctors diagnose it using a simple test: measuring blood pressure and heart rate while lying down, then again after standing for 1 and 3 minutes. A drop of 20 mmHg in systolic pressure or 10 mmHg in diastolic pressure confirms the condition. Additional tests may include ECG, echocardiogram, or autonomic function studies.
Conclusion: Listen to Your Body and Act Early
Dizziness when standing up suddenly is more than just an inconvenience—it’s your body signaling a possible imbalance. While many cases stem from reversible causes like dehydration or medication side effects, others point to deeper cardiovascular or neurological concerns. Ignoring recurring symptoms can lead to falls, injuries, or missed diagnoses of serious conditions.
The key is awareness and action. Pay attention to how often dizziness occurs, what triggers it, and whether it’s getting worse. Simple habits—staying hydrated, moving mindfully, and reviewing medications—can make a significant difference. But if symptoms persist or escalate, don’t hesitate to seek medical advice.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?