It’s a sensation many people know all too well: you rise from a seated or lying position, and suddenly the room tilts. Your vision may blur, your ears might ring, and for a few disorienting seconds, you feel like you’re about to collapse. This momentary dizziness—often called “getting lightheaded”—is usually brief and harmless. But when it happens frequently or is accompanied by other symptoms, it could signal an underlying issue worth investigating.
The medical term for this phenomenon is *orthostatic hypotension*, also known as postural hypotension. It occurs when your blood pressure drops significantly upon standing, reducing blood flow to the brain. While occasional episodes are common and typically resolve within seconds, persistent or severe dizziness warrants attention. Understanding why this happens—and knowing when to seek help—is essential for maintaining long-term health and preventing falls or more serious complications.
What Causes Dizziness When Standing Up?
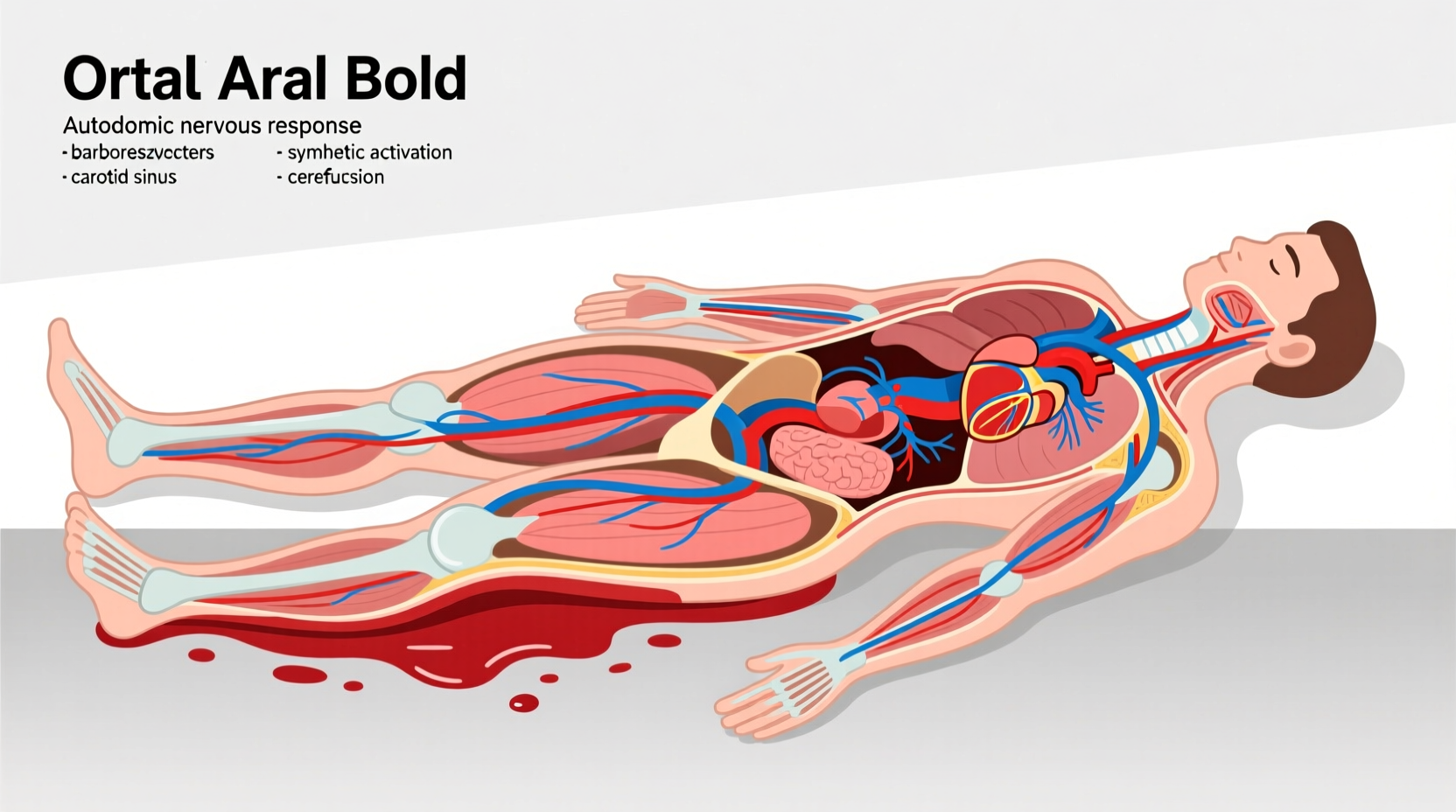
When you stand up, gravity pulls blood downward into your legs and abdomen. In response, your body automatically adjusts: your heart rate increases slightly, blood vessels constrict, and hormones like norepinephrine are released to maintain steady blood pressure and ensure adequate oxygen reaches the brain. This process, managed by the autonomic nervous system, normally works seamlessly.
However, if this regulatory system falters—even briefly—the result is a temporary drop in blood pressure. That dip reduces cerebral perfusion (blood supply to the brain), leading to dizziness, lightheadedness, blurred vision, or even fainting.
Common causes include:
- Dehydration: Low fluid volume reduces overall blood pressure.
- Medications: Blood pressure drugs, diuretics, antidepressants, and Parkinson’s medications can impair vascular regulation.
- Prolonged bed rest: Muscles weaken and circulation adapts poorly to upright posture.
- Age-related changes: The autonomic nervous system becomes less responsive over time.
- Meals (especially large ones): Blood diverts to the digestive tract, lowering pressure elsewhere.
How the Body Regulates Blood Pressure During Position Changes
The transition from lying down to standing involves rapid physiological coordination. Within one to two seconds of standing, approximately 500–800 mL of blood shifts to the lower body. To compensate, baroreceptors in the carotid arteries and aortic arch detect the pressure change and send signals to the brainstem. The sympathetic nervous system then triggers vasoconstriction and a modest increase in heart rate—usually 10–20 beats per minute—to stabilize blood pressure.
In healthy individuals, systolic blood pressure should not drop more than 20 mm Hg, and diastolic no more than 10 mm Hg, within three minutes of standing. A larger drop defines orthostatic hypotension.
This reflex can be impaired by neurological conditions (like diabetes-induced neuropathy), cardiovascular disease, or aging. Even temporary factors such as alcohol consumption or heat exposure can delay or weaken the response.
“Orthostatic hypotension isn’t just a nuisance—it’s a window into autonomic function. Recurrent episodes deserve evaluation.” — Dr. Lena Patel, Neurologist and Autonomic Specialist, Mayo Clinic
When Should You Be Concerned?
Occasional, mild dizziness lasting only a few seconds after standing is generally not a cause for alarm. However, certain red flags suggest the need for medical assessment:
| Symptom Pattern | Normal Reaction | Sign of Concern |
|---|---|---|
| Dizziness duration | Less than 5 seconds | Lasts longer than 30 seconds or leads to near-fainting |
| Frequency | Rare, situational (e.g., after dehydration) | Multiple times daily or weekly without clear trigger |
| Associated symptoms | Mild lightheadedness only | Chest pain, palpitations, confusion, slurred speech, or loss of consciousness |
| Impact on daily life | No functional limitation | Avoids standing, uses furniture for support, or has fallen |
If dizziness is recurrent or worsens over time, especially in older adults, it may indicate:
- Autonomic dysfunction: Seen in Parkinson’s disease, multiple system atrophy, or diabetic neuropathy.
- Heart rhythm disorders: Bradycardia or arrhythmias that impair cardiac output.
- Anemia or low blood volume: Reduces oxygen-carrying capacity and circulating blood.
- Adrenal insufficiency: Impacts hormone regulation of blood pressure.
Mini Case Study: Recognizing a Hidden Condition
John, a 67-year-old man with type 2 diabetes, began experiencing frequent dizziness when getting out of bed. He dismissed it as “just getting older” until he fainted while walking to the bathroom one morning. After being hospitalized, tests revealed significant orthostatic hypotension and reduced heart rate variability—signs of autonomic neuropathy caused by long-term poor glucose control. With medication adjustments, increased salt and fluid intake, and compression stockings, his symptoms improved dramatically. His case underscores how seemingly minor symptoms can mask progressive neurological damage.
Prevention and Management Strategies
For most people, simple lifestyle changes can reduce or eliminate episodes of dizziness upon standing. These strategies work by improving blood volume, enhancing vascular tone, or minimizing sudden pressure drops.
Step-by-Step Guide to Safer Position Changes
- Pause before rising: When waking, sit on the edge of the bed for 10–15 seconds with feet on the floor.
- Contract leg muscles: Before standing, tense your calves and thighs to push blood upward.
- Rise slowly: Use arms to assist from a chair, avoiding quick jerks.
- Stand still initially: Remain motionless for 10 seconds after standing to allow circulation to adjust.
- Stay hydrated: Drink water throughout the day, especially in hot weather or after exercise.
Checklist: Daily Habits to Reduce Dizziness
- ✅ Drink at least 1.5–2 liters of water daily unless contraindicated.
- ✅ Limit alcohol and caffeine, both of which can dehydrate and affect vascular tone.
- ✅ Avoid large carbohydrate-heavy meals; opt for smaller, frequent meals instead.
- ✅ Review medications with your doctor—some may contribute to low blood pressure.
- ✅ Wear compression stockings (20–30 mmHg) if recommended by a physician.
- ✅ Exercise regularly to improve circulation and vascular responsiveness.
- ✅ Sleep with the head of the bed elevated 6–8 inches to reduce nighttime pooling.
For those with diagnosed orthostatic hypotension, doctors may recommend increasing dietary salt under supervision, prescribing fludrocortisone (to retain fluid), or midodrine (a vasoconstrictor). However, these treatments require careful monitoring due to potential side effects.
Frequently Asked Questions
Is it normal to feel dizzy every time I stand up?
No. While occasional dizziness can happen due to dehydration or fatigue, feeling dizzy every time you stand is not normal and suggests a consistent failure in blood pressure regulation. It should be evaluated by a healthcare provider, especially if it interferes with daily activities.
Can anxiety cause dizziness when standing?
Anxiety itself doesn’t directly cause orthostatic hypotension, but it can amplify symptoms. Hyperventilation during anxious episodes alters blood chemistry and may lead to lightheadedness. Additionally, people with anxiety may become hyper-aware of bodily sensations, making normal fluctuations feel more alarming. However, true orthostatic dizziness is tied to measurable blood pressure changes, not psychological state alone.
Can young people experience this, or is it only an older adult issue?
While more common in adults over 65 due to age-related declines in autonomic function, younger individuals can also experience orthostatic hypotension. Causes in younger people include dehydration, eating disorders, prolonged inactivity, pregnancy, or conditions like POTS (Postural Orthostatic Tachycardia Syndrome), where heart rate spikes abnormally upon standing.
Conclusion: Listen to Your Body, Act When Needed
Feeling dizzy when standing up too fast is often a fleeting inconvenience, easily corrected by slowing down and staying hydrated. But the body rarely sends warning signs without reason. Recurrent or worsening dizziness is a cue to pause and assess—not just your posture, but your overall health.
Whether it’s adjusting medications, managing chronic conditions, or simply drinking more water, small changes can yield significant improvements in stability and quality of life. Don’t dismiss persistent symptoms as “just part of aging.” Early intervention can prevent falls, improve independence, and uncover hidden health issues before they escalate.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?