Have you ever stood up quickly and suddenly felt lightheaded, unsteady, or even saw stars? You’re not alone. Millions of people experience this sensation at some point in their lives. While it may seem like a minor inconvenience, recurring dizziness upon standing can be a sign of a condition known as orthostatic hypotension. Understanding the mechanics behind this phenomenon is essential—not only for comfort but also for long-term health.
Orthostatic hypotension, sometimes referred to as postural hypotension, occurs when your blood pressure drops significantly upon changing positions—specifically from sitting or lying down to standing. This sudden drop reduces blood flow to the brain, leading to temporary dizziness, blurred vision, or even fainting. Though occasional episodes are common, especially after dehydration or prolonged bed rest, frequent symptoms warrant attention.
How Blood Pressure Responds to Posture Changes
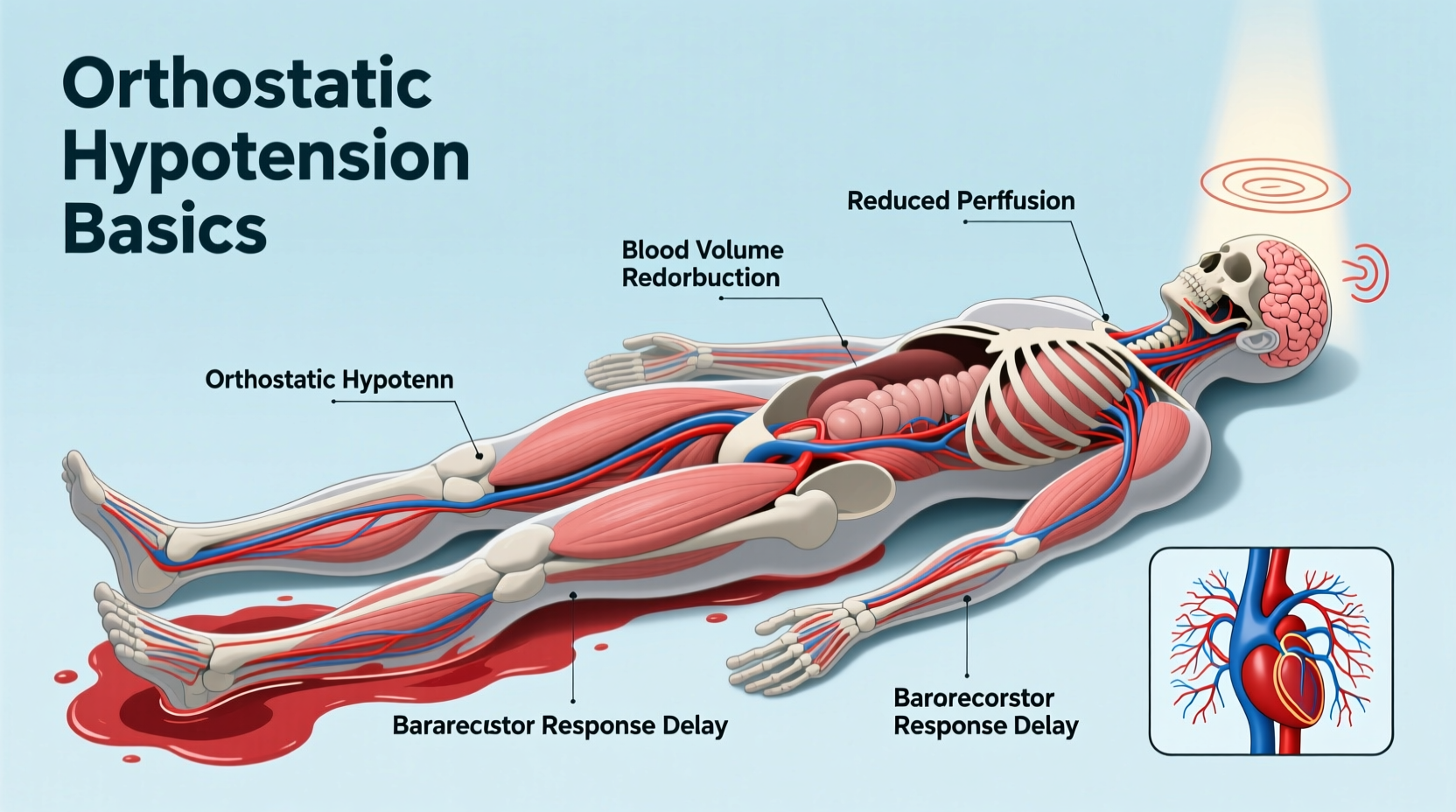
When you stand up, gravity pulls blood downward into your legs and abdomen. In response, your body automatically triggers a series of adjustments to maintain adequate blood flow to the brain. These include tightening blood vessels (vasoconstriction), increasing heart rate slightly, and shifting fluid volume to keep circulation stable. This process is managed by the autonomic nervous system—a network that controls involuntary functions like breathing, digestion, and blood pressure regulation.
In individuals with orthostatic hypotension, this regulatory system falters. The blood vessels don’t constrict efficiently, or the heart doesn’t respond quickly enough, causing a temporary shortfall in cerebral perfusion—the delivery of oxygen-rich blood to the brain. The result? A brief but disorienting episode of dizziness or lightheadedness, typically lasting just seconds to a few minutes.
Common Causes of Orthostatic Hypotension
Several factors can interfere with the body’s ability to regulate blood pressure during position changes. Some are temporary and easily corrected; others may signal underlying medical conditions.
- Dehydration: Insufficient fluid intake reduces blood volume, making it harder for the body to maintain pressure.
- Medications: Diuretics, antihypertensives, antidepressants, and Parkinson’s drugs can all affect blood pressure control.
- Aging: As we age, the autonomic nervous system becomes less responsive, increasing susceptibility.
- Prolonged bed rest: Extended immobility weakens cardiovascular adaptation to upright posture.
- Heart conditions: Bradycardia, heart failure, or valve problems impair effective circulation.
- Nervous system disorders: Parkinson’s disease, multiple system atrophy, and diabetic neuropathy damage autonomic nerves.
- Low blood sugar or anemia: While not direct causes, they can worsen symptoms.
“Orthostatic hypotension isn’t just a nuisance—it can be a window into broader cardiovascular or neurological health.” — Dr. Linda Chen, Neurocardiologist, Mayo Clinic
Recognizing Symptoms and When to Seek Help
Dizziness is the hallmark symptom, but orthostatic hypotension can manifest in several ways:
- Lightheadedness or feeling faint
- Blurred or tunnel vision
- Nausea
- Weakness or fatigue
- Confusion or difficulty concentrating
- Fainting (syncope)
Symptoms usually begin within seconds to a minute after standing and resolve quickly once seated or lying down. However, if episodes occur frequently, lead to falls, or happen without positional change, further evaluation is crucial.
Certain red flags should prompt immediate medical consultation:
- Fainting spells, especially more than once
- Chest pain or palpitations during episodes
- Shortness of breath
- Unexplained weight loss or tremors
- Progressive worsening over time
Diagnosing Orthostatic Hypotension: What to Expect
If your doctor suspects orthostatic hypotension, they will likely perform a simple bedside test called the “orthostatic vital signs” assessment. This involves measuring your blood pressure and heart rate while lying down, then again after one and three minutes of standing.
A diagnosis is typically confirmed if:
- Systolic blood pressure drops by 20 mm Hg or more, OR
- Diastolic blood pressure drops by 10 mm Hg or more
within three minutes of standing, accompanied by relevant symptoms.
Depending on initial findings, additional tests may be recommended:
| Test | Purpose | What It Involves |
|---|---|---|
| Electrocardiogram (ECG) | Check heart rhythm and electrical activity | Non-invasive sensors placed on chest and limbs |
| Echocardiogram | Assess heart structure and pumping function | Ultrasound imaging of the heart |
| Tilt table test | Mimic posture changes under controlled conditions | Lying on a table tilted upright while vitals are monitored |
| Blood tests | Rule out anemia, diabetes, electrolyte imbalances | Standard lab draw |
| Autonomic function testing | Evaluate nervous system control of BP and HR | Specialized labs using breathing, pressure, and sweat tests |
Effective Management Strategies
Treatment depends on the underlying cause, but many cases improve with lifestyle modifications and medication review. The goal is to reduce symptom frequency and prevent injury from falls.
Step-by-Step Guide to Reduce Episodes
- Hydrate consistently: Aim for 6–8 glasses of water daily. Increase intake in hot weather or after exercise.
- Rise slowly: After waking, sit on the edge of the bed for 30 seconds before standing.
- Stay physically active: Regular aerobic exercise improves circulation and vascular tone.
- Wear compression stockings: These help push blood upward from the legs and reduce pooling.
- Review medications: Ask your doctor if any prescriptions could be contributing.
- Avoid large meals: Big portions redirect blood to the digestive tract, worsening dizziness.
- Limit alcohol: It dehydrates and dilates blood vessels, both of which lower blood pressure.
Real-Life Example: Maria’s Experience
Maria, a 68-year-old retired teacher, began noticing she felt “woozy” every morning when getting out of bed. At first, she dismissed it as aging. But after nearly falling twice in the bathroom, she consulted her primary care physician. Her blood pressure was normal while seated but dropped from 130/80 to 105/65 within 60 seconds of standing.
Further investigation revealed she was taking a diuretic for mild hypertension and hadn’t been drinking enough fluids. Her doctor adjusted her medication timing and advised increased salt and water intake. Within two weeks, her symptoms improved dramatically. A follow-up visit confirmed stabilized orthostatic readings.
Maria’s case illustrates how seemingly minor factors—medication timing, hydration—can have significant effects. Early intervention prevented potential falls and improved her confidence in daily movement.
Do’s and Don’ts for Managing Orthostatic Hypotension
| Do | Don't |
|---|---|
| Drink plenty of fluids throughout the day | Go for long periods without drinking |
| Move your legs before standing (e.g., ankle pumps) | Stand up abruptly from lying or sitting |
| Elevate the head of your bed slightly (6–8 inches) | Sleep completely flat if symptoms are worse in the morning |
| Monitor symptoms and track patterns | Ignore repeated dizziness or near-fainting episodes |
| Wear waist-high compression garments | Use knee-high socks—they're less effective |
FAQ
Can orthostatic hypotension go away on its own?
Yes, in cases caused by temporary factors like dehydration, illness, or medication side effects, symptoms often resolve once the trigger is addressed. Chronic forms related to neurological conditions may require ongoing management.
Is orthostatic hypotension dangerous?
While brief dizziness is usually harmless, recurrent episodes increase the risk of falls, fractures, and reduced quality of life. In older adults, it’s linked to higher rates of cardiovascular events and cognitive decline. Proper diagnosis and treatment reduce these risks.
Can young people get orthostatic hypotension?
Absolutely. It’s common in teens and young adults, particularly those with conditions like POTS (postural orthostatic tachycardia syndrome). Athletes, individuals with eating disorders, or those recovering from infections may also experience temporary forms.
Conclusion: Take Control of Your Stability
Feeling dizzy when standing up isn’t something you should simply learn to live with. Orthostatic hypotension is a manageable condition, but only if recognized and addressed. Whether it’s adjusting your morning routine, reevaluating medications, or seeking specialized care, small changes can make a profound difference in your daily well-being.
Start by tracking your symptoms: note when they happen, how long they last, and what you were doing beforehand. Share this information with your healthcare provider. Awareness is the first step toward stability—both physical and emotional.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?