Standing up from a seated or lying position should be a seamless motion. But if you’ve ever risen too fast and suddenly felt lightheaded, unsteady, or like the room is spinning, you’re not alone. This sensation—commonly known as orthostatic dizziness—is more than just a fleeting annoyance. It’s often a signal from your body about how well your circulatory system is adapting to changes in posture. Two major contributors to this experience are hydration levels and blood pressure regulation. Understanding the connection between these factors can help you manage symptoms and maintain better daily energy and balance.
The Science Behind Dizziness Upon Standing
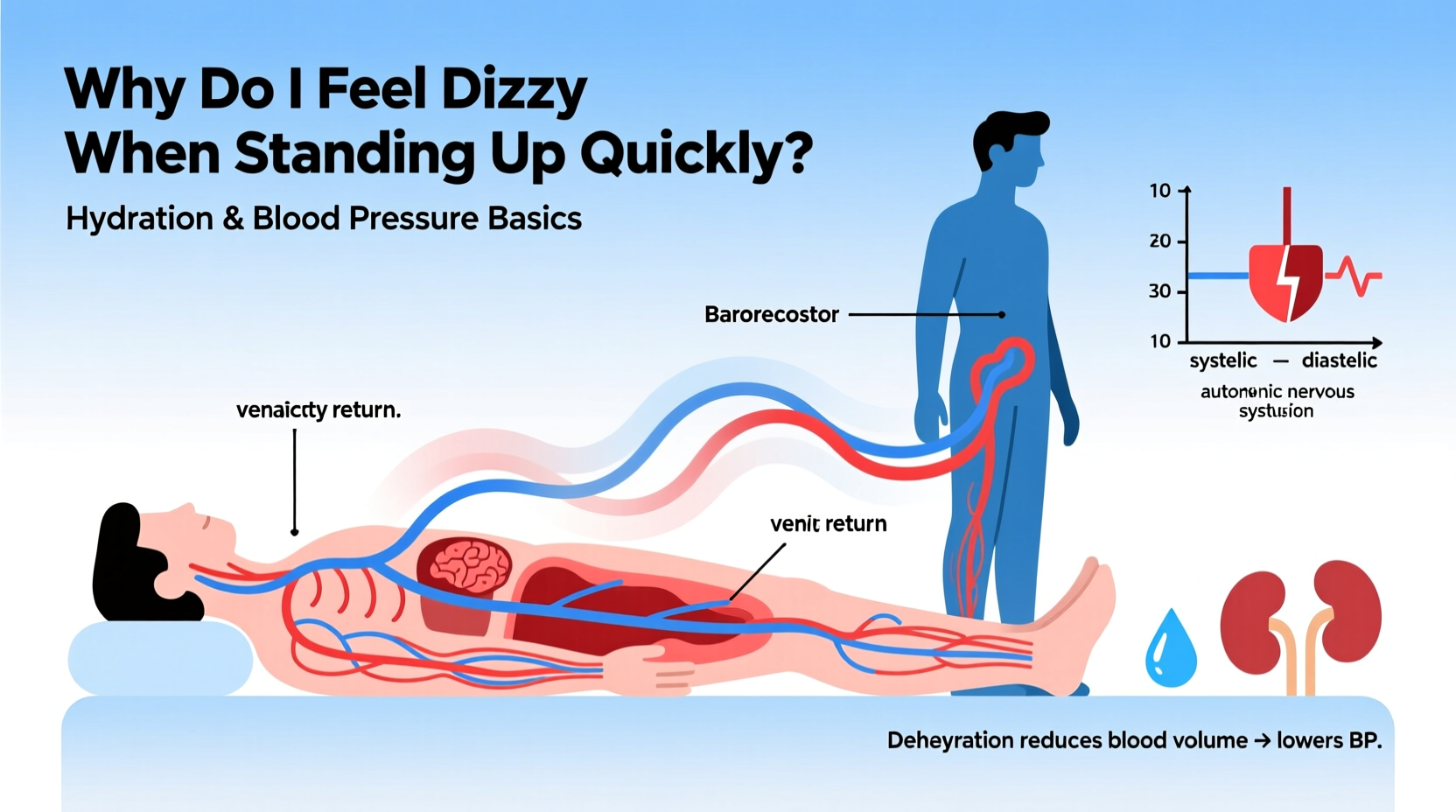
When you stand up, gravity pulls blood downward into your legs and abdomen. In response, your cardiovascular system must act quickly to maintain adequate blood flow to your brain. Normally, your heart rate increases slightly, and your blood vessels constrict to keep blood pressure stable. If this adjustment is delayed or insufficient, cerebral perfusion drops temporarily, leading to dizziness, blurred vision, or even fainting.
This condition is medically referred to as orthostatic hypotension, defined as a drop in systolic blood pressure of at least 20 mm Hg or diastolic pressure by 10 mm Hg within three minutes of standing. While occasional mild dizziness may be harmless, frequent episodes warrant attention, especially when tied to lifestyle factors like hydration and nutrition.
How Hydration Influences Blood Pressure and Balance
Blood volume plays a crucial role in maintaining consistent blood pressure. When you're well-hydrated, your circulatory system has enough fluid to keep blood moving efficiently through your arteries and veins. Dehydration reduces blood volume, which in turn lowers blood pressure and impairs the body’s ability to compensate for gravitational shifts during standing.
Even mild dehydration—losing as little as 1–2% of your body's water—can impair cognitive function and physical stability. For example, someone weighing 70 kg (154 lbs) may begin experiencing symptoms after losing just 700–1400 mL of fluid. Common causes include inadequate water intake, excessive sweating, alcohol consumption, or illness involving vomiting or diarrhea.
Sodium also plays a balancing act here. While excess sodium is often cautioned against, too little can contribute to low blood pressure, especially in active individuals who sweat heavily. Sodium helps retain fluid in the bloodstream, supporting vascular volume. Athletes or those on low-salt diets may unknowingly predispose themselves to postural dizziness.
“Hydration status directly affects autonomic nervous system responses. Chronic underhydration can blunt the body’s ability to regulate blood pressure during positional changes.” — Dr. Lena Torres, Cardiovascular Physiologist
Key Risk Factors for Orthostatic Dizziness
Not everyone experiences dizziness upon standing, but certain conditions increase susceptibility. Recognizing these risk factors allows for proactive management:
- Age: As we age, baroreceptor sensitivity declines, making blood pressure adjustments slower.
- Medications: Diuretics, antihypertensives, antidepressants, and Parkinson’s drugs can interfere with blood pressure control.
- Dietary habits: Low salt intake, skipping meals, or rapid weight loss can reduce circulating volume.
- Medical conditions: Diabetes, anemia, adrenal insufficiency, and autonomic neuropathy disrupt normal regulation.
- Inactivity: Prolonged bed rest or sedentary lifestyle weakens circulatory responsiveness.
Women may be more prone due to generally lower baseline blood pressure and hormonal fluctuations, particularly during menstruation or menopause. However, men are not exempt—especially those with undiagnosed hypertension or cardiovascular issues masked by medication-induced lowering of pressure.
Step-by-Step Guide to Preventing Dizziness When Standing
Managing orthostatic dizziness doesn’t require drastic measures. Small, consistent changes can significantly improve your body’s response to positional shifts. Follow this timeline-based approach:
- Morning (Before Getting Out of Bed): Lie flat for 30 seconds, then sit at the edge of the bed for another 30 seconds before standing. This gives your circulation time to adjust.
- Throughout the Day: Sip water consistently rather than drinking large amounts infrequently. Aim for pale yellow urine as a hydration marker.
- After Sitting for Long Periods: Flex your calf muscles and shift your weight before rising. This “muscle pump” action helps push blood back toward the heart.
- During Episodes: If you feel dizzy, immediately sit or lie down. Cross your legs and tense your leg, abdominal, and gluteal muscles to raise blood pressure temporarily.
- Evening Review: Reflect on patterns—did dizziness follow heat exposure, missed meals, or increased activity? Track symptoms in a journal for two weeks.
Over time, this routine strengthens your body’s adaptive mechanisms and reduces reliance on emergency compensatory actions.
Do’s and Don’ts: Managing Hydration and Blood Pressure
| Do | Don't |
|---|---|
| Drink water steadily throughout the day (about 2–2.5 liters for most adults) | Wait until you're thirsty to drink—thirst is a late sign of dehydration |
| Include moderate salt in your diet if blood pressure is normally low | Overuse diuretic beverages like coffee or tea without balancing fluids |
| Eat small, balanced meals regularly to stabilize blood sugar and volume | Stand up abruptly after prolonged sitting or lying down |
| Monitor symptoms and consult a doctor if dizziness becomes frequent | Ignore recurrent dizziness, especially if accompanied by palpitations or fainting |
| Wear compression stockings if recommended, especially if standing for long periods | Self-diagnose or stop prescribed medications without medical advice |
Real-Life Example: Maria’s Morning Struggles
Maria, a 48-year-old office worker, began noticing she frequently felt “woozy” when getting up from her desk or after waking. She assumed it was stress-related fatigue. After a particularly intense episode where she nearly fainted in the bathroom, she consulted her primary care physician.
Her evaluation revealed mildly low blood pressure (106/64 mm Hg) and signs of chronic mild dehydration. She admitted to drinking only one glass of water daily, relying mostly on diet soda. Her lunch was often skipped, and she exercised intensely three times a week without adjusting fluid intake.
With guidance, Maria started drinking 1.5 liters of water daily, added a pinch of sea salt to her morning lemon water, and began eating a protein-rich snack before bedtime. Within two weeks, her symptoms improved dramatically. Her doctor noted her standing blood pressure stabilized, and she reported feeling more alert and physically steady throughout the day.
Maria’s case illustrates how subtle imbalances—easily overlooked—can manifest as disorienting symptoms. Correcting them didn’t require medication, just awareness and consistent habit change.
Expert Recommendations for Daily Management
Clinicians emphasize that prevention starts with routine self-awareness. Monitoring your body’s signals is key. Here are evidence-based strategies endorsed by healthcare professionals:
- Hydration tracking: Use a marked water bottle or app to ensure consistent intake.
- Postural training: Practice slow transitions and isometric exercises like leg crossing to build tolerance.
- Nutritional balance: Ensure adequate intake of electrolytes—sodium, potassium, and magnesium—through whole foods.
- Regular movement: Avoid sitting for more than 60 minutes at a time; walk briefly every hour.
- Medical review: If taking blood pressure medications, discuss dose timing with your doctor—some are more likely to cause morning dips.
Frequently Asked Questions
Is it normal to feel dizzy every time I stand up?
No, regular dizziness upon standing is not considered normal. Occasional mild lightheadedness may happen, especially after dehydration or prolonged sitting. But if it occurs frequently, it could indicate underlying issues such as hypovolemia (low blood volume), autonomic dysfunction, or medication side effects. Persistent symptoms should be evaluated by a healthcare provider.
Can drinking more water really help with dizziness?
Yes, especially if your dizziness is linked to dehydration. Increasing fluid intake improves blood volume and supports stable blood pressure during posture changes. Studies show that drinking 500 mL of water can raise blood pressure within minutes in people prone to orthostatic hypotension. However, water alone isn’t a cure-all—electrolyte balance and overall health matter too.
Should I be worried if I sometimes see stars when I stand?
Seeing “stars” or darkening vision when standing is typically due to transient reduced blood flow to the visual cortex. While brief episodes are common and usually benign, they shouldn’t be ignored if they worsen or come with other symptoms like chest pain, irregular heartbeat, or confusion. These could point to cardiovascular or neurological concerns needing further investigation.
Conclusion: Take Control of Your Stability
Dizziness when standing up quickly is more than just a minor inconvenience—it’s a physiological clue. Your body relies on a finely tuned interplay between hydration, blood pressure, and nervous system coordination to keep you upright and alert. Ignoring repeated episodes risks falls, reduced quality of life, and missed opportunities to catch early signs of imbalance.
You don’t need complex interventions to make meaningful improvements. Start today: refill your water bottle, pause before standing, assess your diet, and track your symptoms. Small adjustments compound into lasting resilience. If symptoms persist, seek professional evaluation—your health deserves attention, not assumption.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?