That sudden wave of lightheadedness or unsteadiness after rising from a seated or lying position is more than just an inconvenience—it’s your body signaling a temporary drop in blood flow to the brain. This phenomenon, commonly known as orthostatic hypotension or postural dizziness, affects millions of people across all age groups. While occasional episodes are usually harmless, frequent or severe dizziness upon standing may point to underlying health issues. Understanding the root causes and adopting targeted prevention strategies can help you regain stability and confidence in daily movement.
What Happens When You Stand Up Suddenly?
When you transition from sitting or lying down to standing, gravity pulls blood downward into your legs and abdomen. In response, your autonomic nervous system normally triggers rapid adjustments: blood vessels constrict, heart rate increases slightly, and cardiac output rises to maintain consistent blood pressure and ensure adequate oxygen delivery to the brain. When this system falters—even briefly—blood pressure drops, leading to reduced cerebral perfusion and symptoms like dizziness, blurred vision, or even fainting.
This transient condition is formally called orthostatic hypotension, defined by a drop of at least 20 mm Hg in systolic blood pressure or 10 mm Hg in diastolic pressure within three minutes of standing. For most people, it lasts only seconds. But for others, especially older adults or those with chronic conditions, it can be recurrent and disruptive.
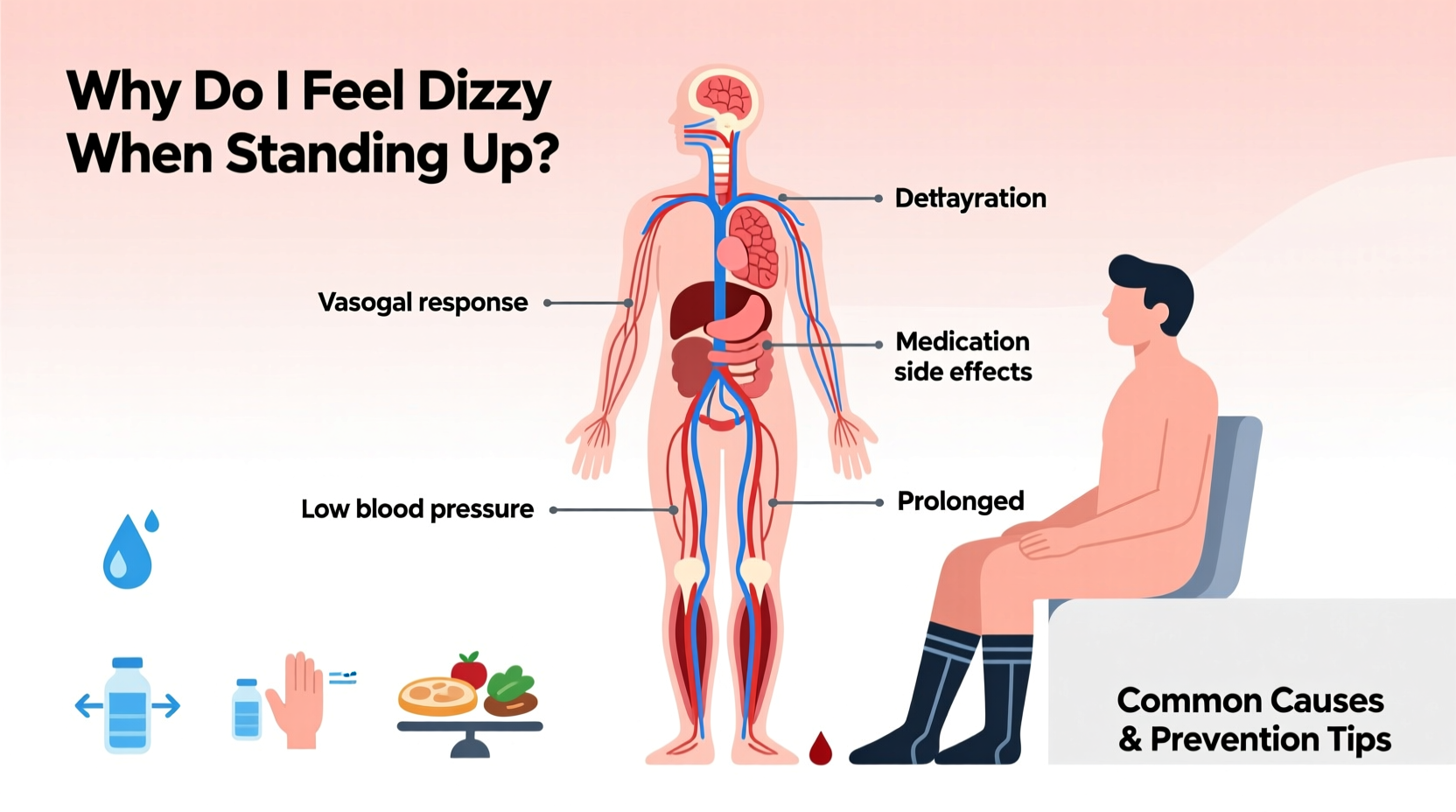
Common Causes of Sudden Dizziness Upon Standing
Dizziness when standing isn’t always due to one single factor. It often results from a combination of physiological changes, lifestyle habits, and medical influences. Below are some of the most prevalent contributors:
1. Dehydration
Inadequate fluid intake reduces blood volume, making it harder for your body to maintain stable blood pressure during posture changes. Even mild dehydration—such as skipping water after exercise or not drinking enough on hot days—can trigger dizziness.
2. Medications
Several prescription drugs affect blood pressure regulation. These include:
- Diuretics (water pills)
- Alpha-blockers used for prostate issues or high blood pressure
- Antidepressants, particularly tricyclics
- Anti-anxiety medications
- Parkinson’s disease treatments
If you’ve recently started or changed medication and noticed increased dizziness, consult your doctor before making any adjustments.
3. Age-Related Changes
As we age, the autonomic nervous system becomes less responsive. Blood vessels lose elasticity, and baroreceptor sensitivity declines—both impairing the body's ability to quickly regulate blood pressure. This makes orthostatic hypotension significantly more common in individuals over 65.
4. Prolonged Bed Rest or Inactivity
Extended periods of immobility—such as recovery from surgery or illness—can weaken cardiovascular responsiveness. After days of lying down, the body struggles to adapt to upright posture, increasing dizziness risk.
5. Underlying Medical Conditions
Certain chronic diseases interfere with normal blood pressure control:
- Diabetes: Can damage nerves involved in blood pressure regulation (autonomic neuropathy).
- Parkinson’s disease: Impairs autonomic function and dopamine-related vascular tone.
- Heart conditions: Arrhythmias, heart failure, or valve disorders limit effective circulation.
- Anemia: Low red blood cell count reduces oxygen-carrying capacity, amplifying dizziness symptoms.
“Orthostatic hypotension should never be dismissed as ‘just getting old.’ It’s a measurable sign that warrants evaluation, especially if it leads to falls.” — Dr. Lena Patel, Neurologist and Autonomic Specialist
Prevention Tips to Reduce Dizziness When Standing
You don’t have to live with recurring dizziness. Simple, evidence-based strategies can significantly reduce or eliminate symptoms by supporting better blood pressure control and circulation.
1. Move Gradually Between Positions
Instead of jumping out of bed or rising abruptly from a chair, follow a stepwise approach:
- When lying down, sit up first and stay seated on the edge of the bed for 10–30 seconds.
- Stand slowly, holding onto a stable surface.
- Pause for another 10–15 seconds before walking.
This allows your cardiovascular system time to compensate for gravitational shifts.
2. Stay Hydrated Throughout the Day
Maintaining optimal fluid balance supports blood volume and pressure stability. Aim for 6–8 glasses of water daily, adjusting for climate, activity level, and individual needs. If you're prone to low sodium levels, your doctor might recommend slightly increasing salt intake—but only under supervision.
3. Avoid Triggers Like Heat and Alcohol
Hot environments (saunas, baths, summer weather) cause blood vessels to dilate, worsening blood pressure drops. Similarly, alcohol impairs autonomic reflexes and acts as a diuretic. Limit exposure to these triggers, especially around times when you’re likely to stand up frequently.
4. Wear Compression Stockings
These specially designed garments apply gentle pressure to the legs, reducing blood pooling and improving venous return to the heart. They’re particularly helpful for people with chronic orthostatic hypotension or varicose veins.
5. Perform Counterpressure Maneuvers
For those who experience warning signs like lightheadedness or tunnel vision, certain physical techniques can prevent full-blown dizziness:
- Cross your legs and tense leg muscles while standing.
- Squeeze a rubber ball or clench fists firmly.
- Lean forward slightly or bend at the waist.
These actions increase vascular resistance and boost blood pressure temporarily.
Do’s and Don’ts: Managing Postural Dizziness
| Do’s | Don’ts |
|---|---|
| Stay well-hydrated throughout the day | Ignore repeated episodes of dizziness |
| Rise slowly from sitting or lying positions | Stand up too quickly after long rest |
| Eat smaller, more frequent meals (large meals can worsen symptoms) | Consume excessive alcohol or caffeine |
| Review medications with your doctor regularly | Stop prescribed meds without medical advice |
| Use compression stockings if recommended | Exercise in extreme heat or humidity |
Real-Life Example: Maria’s Experience with Morning Dizziness
Maria, a 72-year-old retired teacher, began experiencing frequent dizziness when getting out of bed. At first, she brushed it off as aging. But after nearly falling twice in one week, she consulted her physician. Testing revealed mild orthostatic hypotension linked to a combination of her blood pressure medication and lower-than-normal fluid intake.
Her doctor adjusted her medication timing and advised her to drink a glass of water before rising each morning. She also started wearing mid-thigh compression stockings and adopted a “sit-wait-stand” routine. Within two weeks, her symptoms improved dramatically. More importantly, her confidence in moving safely returned.
Maria’s case highlights how identifying contributing factors—and applying simple interventions—can lead to meaningful improvements without drastic lifestyle overhauls.
When to See a Doctor
Occasional, brief dizziness when standing is common and often benign. However, seek medical evaluation if you experience:
- Frequent or worsening episodes
- Symptoms lasting longer than a minute or two
- Near-fainting or actual fainting (syncope)
- Chest pain, palpitations, or shortness of breath
- Confusion, slurred speech, or weakness (could indicate neurological issues)
Your healthcare provider may perform a tilt-table test, check for anemia or electrolyte imbalances, or assess autonomic function to determine the underlying cause.
Step-by-Step Guide to Safer Rising
Follow this five-step process every time you get up from bed or a seated position:
- Pause and Breathe: Before moving, take three deep breaths to prepare your nervous system.
- Sit Up Slowly: Roll to your side, then use your arms to push yourself into a seated position on the edge of the bed or chair.
- Wait 30 Seconds: Let your body adjust. Focus on steady breathing.
- Stand Gradually: Use support (like a wall or furniture) to rise slowly to your feet.
- Hold Still Briefly: Remain still for 10–15 seconds before walking to ensure no dizziness occurs.
Practicing this sequence consistently trains your body to respond more efficiently to positional changes.
Frequently Asked Questions
Can low iron cause dizziness when standing up?
Yes. Iron deficiency anemia reduces the blood’s oxygen-carrying capacity, which can amplify symptoms of dizziness, fatigue, and breathlessness when changing positions. Treating the underlying anemia often improves orthostatic tolerance.
Is it normal to feel dizzy after eating and then standing?
In some cases, yes. A condition called postprandial hypotension causes blood pressure to drop after meals, especially large or carbohydrate-heavy ones. Blood diverts to the digestive tract, leaving less available for the brain. Eating smaller meals and remaining seated for 10–15 minutes after eating can help prevent this.
Can anxiety cause dizziness when standing?
While anxiety doesn’t directly cause orthostatic hypotension, it can heighten awareness of bodily sensations and lead to hyperventilation, which may mimic or worsen dizziness. However, true postural dizziness stems from measurable blood pressure changes, so proper diagnosis is key.
Conclusion: Take Control of Your Stability
Feeling dizzy when standing up suddenly is more than just a fleeting discomfort—it’s a signal from your body that deserves attention. Whether caused by dehydration, medication side effects, or age-related changes, most cases can be managed effectively with informed habits and preventive care. By staying hydrated, moving mindfully, reviewing medications, and recognizing warning signs, you can minimize dizziness and reduce fall risks.
If symptoms persist or interfere with daily life, don’t hesitate to consult a healthcare professional. Early intervention can uncover treatable conditions and restore your sense of balance—literally and figuratively.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?