Standing up too quickly and feeling lightheaded or unsteady is a common experience—many people have felt it after sitting for a long time or rising from bed in the morning. This sensation, often described as dizziness, lightheadedness, or even a brief \"graying out\" of vision, usually passes within seconds. But how do you know when this reaction is just a minor bodily quirk and when it might signal something more serious?
The medical term for this phenomenon is *orthostatic hypotension*—a drop in blood pressure that occurs when transitioning from lying down or sitting to standing. While occasional episodes are generally harmless, frequent or severe dizziness upon standing can point to underlying health issues such as dehydration, heart conditions, neurological disorders, or medication side effects.
Understanding the causes, risk factors, and warning signs helps determine when self-care is sufficient and when it’s time to consult a healthcare provider.
What Happens When You Stand Up Suddenly?
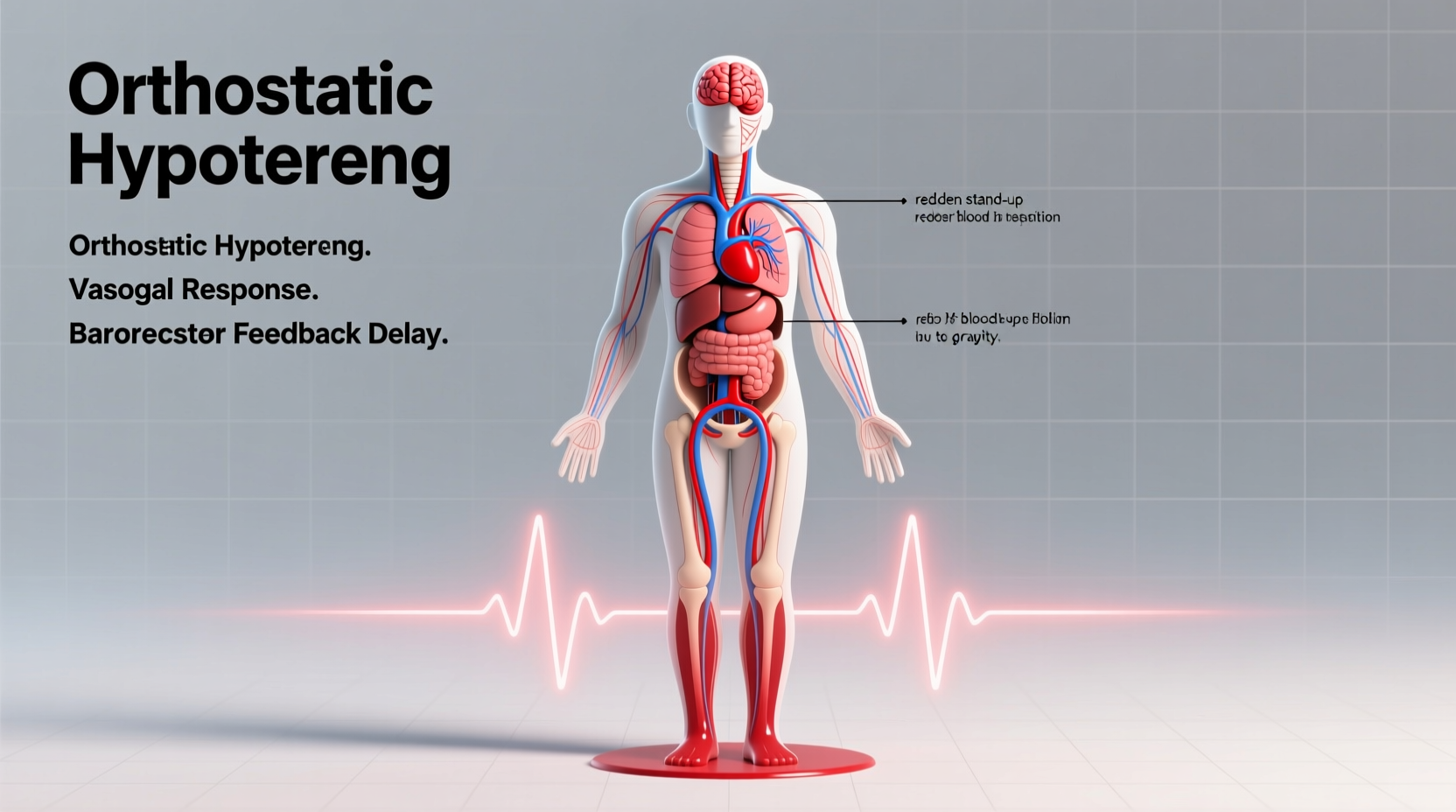
When you stand up, gravity pulls blood downward into your legs and abdomen. This reduces the amount of blood returning to your heart, which temporarily lowers cardiac output and blood pressure. In response, your autonomic nervous system should quickly compensate by constricting blood vessels and increasing heart rate to maintain adequate blood flow to the brain.
If this regulatory system is slow or impaired, blood pressure drops significantly before it’s corrected. This delay results in reduced cerebral perfusion—the brain isn’t getting enough oxygen-rich blood—which causes dizziness, blurred vision, weakness, or even fainting.
This process typically resolves within 10–30 seconds as your circulation adjusts. However, if the adjustment is sluggish or incomplete, symptoms may persist longer or occur more frequently.
Common Causes of Dizziness Upon Standing
Several physiological and environmental factors contribute to transient orthostatic hypotension. Most are benign but worth addressing to prevent falls or worsening symptoms.
- Dehydration: Low fluid volume reduces overall blood volume, making it harder for the body to maintain blood pressure during position changes.
- Medications: Diuretics, blood pressure drugs (like beta-blockers or ACE inhibitors), antidepressants, and Parkinson’s medications can impair vascular tone or heart rate regulation.
- Prolonged bed rest: Inactivity weakens circulatory reflexes, especially in older adults recovering from illness.
- Alcohol consumption: Alcohol dilates blood vessels and contributes to dehydration, both of which exacerbate postural drops in blood pressure.
- Meals (especially large ones): Blood flow shifts to the digestive tract after eating, which can lower systemic pressure—a condition known as postprandial hypotension.
- Heat exposure: Hot environments cause vasodilation and sweating, reducing circulating blood volume.
- Pregnancy: Circulating blood volume increases, but vascular resistance drops, sometimes leading to temporary dizziness when standing.
In younger individuals, especially those with naturally low blood pressure or heightened sensitivity to posture changes, these episodes are often sporadic and not concerning unless they interfere with daily life.
When to Be Concerned: Red Flags and Risk Factors
While momentary dizziness upon standing is common, certain patterns suggest the need for medical evaluation. Persistent or worsening symptoms could indicate an underlying disorder affecting the cardiovascular, neurological, or endocrine systems.
“Recurrent dizziness when standing—especially if accompanied by falls or near-fainting—should never be dismissed as ‘just getting old.’ It’s a sign the body isn’t adapting properly.” — Dr. Lena Torres, Neurologist and Autonomic Specialist
Seek prompt medical attention if you experience any of the following:
- Frequent episodes occurring multiple times per week
- Symptoms lasting longer than one minute
- Near-fainting (presyncope) or actual loss of consciousness (syncope)
- Chest pain, palpitations, or shortness of breath during episodes
- Confusion, slurred speech, or limb weakness—signs of stroke
- Dizziness associated with urinary retention, constipation, or sexual dysfunction (possible autonomic neuropathy)
- History of diabetes, Parkinson’s disease, or heart failure
Older adults are particularly vulnerable due to age-related declines in baroreflex sensitivity, reduced muscle pump efficiency in the legs, and polypharmacy. Chronic conditions like diabetes can damage nerves involved in blood pressure control, leading to neurogenic orthostatic hypotension.
Diagnosis and Medical Evaluation
If dizziness upon standing becomes recurrent or disruptive, a doctor will likely perform a structured assessment to identify the root cause.
Step-by-Step Diagnostic Process
- Medical history review: Includes medication list, duration/frequency of symptoms, presence of chronic illnesses, and lifestyle habits.
- Vital signs measurement: Blood pressure and heart rate are recorded while lying down, then immediately after standing and at one and three minutes post-standing.
- Orthostatic vital criteria: A drop of ≥20 mmHg in systolic BP or ≥10 mmHg in diastolic BP within three minutes of standing confirms orthostatic hypotension.
- Further testing (if indicated): May include electrocardiogram (ECG), tilt table test, blood tests (e.g., hemoglobin, electrolytes, glucose), or referral to cardiology or neurology.
In some cases, ambulatory blood pressure monitoring over 24 hours helps capture intermittent drops not seen during clinic visits.
| Parameter | Normal Response | Abnormal Finding (Orthostatic Hypotension) |
|---|---|---|
| Systolic Blood Pressure | Minor change (<10 mmHg drop) | Drop of ≥20 mmHg within 3 minutes |
| Diastolic Blood Pressure | Stable or slight increase | Drop of ≥10 mmHg |
| Heart Rate | Increases by 10–20 bpm | Little or no increase (suggests autonomic failure) |
| Symptoms Duration | Resolves in <30 seconds | Persists beyond 1 minute or leads to syncope |
Managing and Preventing Episodes
For most people, simple lifestyle adjustments significantly reduce or eliminate dizziness when standing. The goal is to support blood return to the heart and improve vascular responsiveness.
Actionable Prevention Checklist
- ✅ Rise slowly: Sit up first, dangle legs off the bed, wait 10–15 seconds, then stand gradually.
- ✅ Increase fluid intake: Aim for 6–8 glasses of water daily unless restricted by a medical condition.
- ✅ Boost salt intake moderately (only under medical supervision): Salt helps retain fluid and raise blood pressure.
- ✅ Avoid alcohol and large carbohydrate-heavy meals, especially in hot environments.
- ✅ Wear compression stockings: These help prevent blood pooling in the legs.
- ✅ Exercise regularly: Focus on leg strength and aerobic conditioning to enhance circulation.
- ✅ Review medications with your doctor: Some drugs can be adjusted or replaced if contributing to symptoms.
Physical maneuvers can also provide immediate relief during an episode. Crossing your legs and tensing your thigh muscles, squeezing a rubber ball, or performing “leg crossing” while standing activates the muscle pump and raises blood pressure within seconds.
Mini Case Study: Maria, Age 72
Maria began experiencing frequent dizziness when getting out of her recliner or rising from bed. At first, she attributed it to aging. But after two near-falls, she visited her primary care physician. Her blood pressure dropped from 130/80 mmHg lying down to 100/68 mmHg after standing—one minute later, she reported tunnel vision.
Review of her medications revealed she was taking amlodipine (a calcium channel blocker) and hydrochlorothiazide (a diuretic) for hypertension. She also admitted to limiting fluids due to frequent urination. After adjusting her medications, increasing hydration, and starting knee-high compression stockings, her symptoms improved dramatically within three weeks. Follow-up testing showed minimal blood pressure drop upon standing.
This case highlights how multiple factors—medication, hydration, and age-related changes—can combine to cause symptomatic orthostatic hypotension, and how targeted interventions can restore stability.
Frequently Asked Questions
Is it normal to feel dizzy every time I stand up?
No, frequent or consistent dizziness when standing is not considered normal. Occasional lightheadedness may happen due to dehydration or fatigue, but regular episodes warrant evaluation. Recurrent symptoms could indicate orthostatic hypotension, autonomic dysfunction, or medication side effects.
Can low iron cause dizziness when standing?
Yes. Iron deficiency anemia reduces the blood’s oxygen-carrying capacity. When combined with a drop in blood pressure upon standing, this can amplify dizziness and fatigue. Blood tests measuring hemoglobin, ferritin, and iron levels can confirm anemia.
How long should dizziness last after standing?
Normal postural dizziness should resolve within 10–30 seconds as your body adjusts. If symptoms persist beyond one minute, worsen over time, or are accompanied by other neurological or cardiac signs, seek medical advice.
Conclusion: Listen to Your Body
Feeling dizzy when standing up suddenly is often fleeting and harmless, but it shouldn't be ignored if it happens regularly or disrupts your life. Your body uses these moments to communicate—sometimes subtly—that its balance systems need attention. Whether it's adjusting hydration, reevaluating medications, or investigating deeper health concerns, proactive steps make a meaningful difference.
Don’t dismiss recurring dizziness as inevitable, especially if you're older or managing chronic conditions. Early intervention prevents falls, improves quality of life, and may uncover treatable medical issues. Talk to your healthcare provider, track your symptoms, and take control of your circulatory health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?