It’s a sensation many people know well: you stand up quickly from sitting or lying down, and suddenly the room tilts slightly. Your vision may blur, your head feels light, and for a few seconds, you wonder if you’re about to lose balance. This momentary dizziness—often called “getting lightheaded”—is surprisingly common. But what causes it, and should you be concerned?
The answer lies in how your body manages blood flow and blood pressure during changes in posture. When you rise from a seated or reclined position, gravity pulls blood downward into your legs and abdomen. Your cardiovascular system must respond rapidly to maintain adequate blood flow to the brain. If this adjustment isn’t swift enough, a temporary drop in cerebral perfusion occurs, leading to dizziness.
This phenomenon is medically known as **orthostatic hypotension** (or postural hypotension), and in most cases, it’s brief and harmless. However, understanding the mechanisms, risk factors, and warning signs can help distinguish between a normal bodily response and a symptom of an underlying condition.
How Blood Pressure Changes with Posture
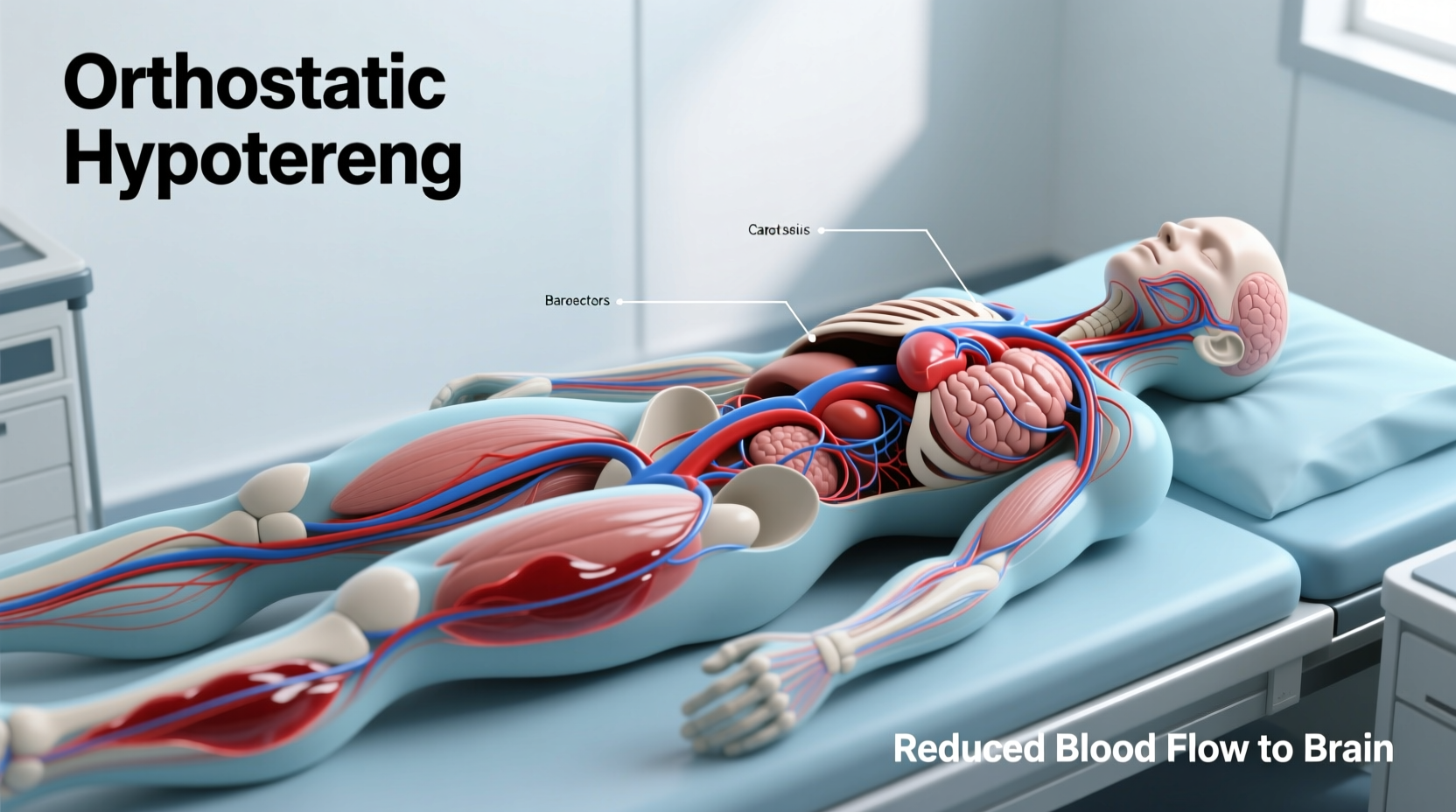
When you lie down, blood distributes evenly throughout your body. Standing up disrupts this equilibrium. Within seconds, approximately 500–800 milliliters of blood shifts to the lower extremities due to gravitational pull. To prevent a critical drop in blood pressure and brain oxygen levels, your autonomic nervous system activates a series of rapid compensatory responses:
- Vasoconstriction: Blood vessels in the legs and abdomen narrow to increase vascular resistance.
- Increased heart rate: The heart beats faster to pump more blood per minute.
- Hormonal adjustments: Norepinephrine and other vasoactive hormones are released to support blood vessel tone.
These reflexes normally occur within one to three heartbeats. When they lag—even by a second or two—blood pressure drops temporarily, reducing blood flow to the brain and causing dizziness, lightheadedness, or even blurred vision.
“Orthostatic symptoms are often benign, but recurrent or severe episodes warrant evaluation. It’s not just about comfort—it’s about identifying potential cardiovascular or neurological issues.” — Dr. Lena Torres, Neurologist and Autonomic Specialist
Is It Normal to Feel Dizzy After Standing Up Quickly?
Yes, occasional mild dizziness upon standing is considered normal, especially in younger adults and adolescents. Studies suggest that up to 30% of healthy individuals experience transient lightheadedness when rising quickly, particularly after prolonged sitting or lying down.
Several factors influence how pronounced this response is:
- Hydration status: Dehydration reduces blood volume, making it harder for the body to compensate.
- Time of day: Blood pressure is naturally lower in the morning, increasing susceptibility.
- Age: Baroreflex sensitivity declines with age, making older adults more prone to orthostatic symptoms.
- Physical fitness: Athletes often have better cardiovascular regulation and fewer symptoms.
When Dizziness Might Signal a Health Problem
While brief dizziness is usually nothing to worry about, certain patterns indicate the need for medical attention. Persistent, severe, or worsening symptoms may point to underlying conditions such as:
- Chronic orthostatic hypotension: A sustained inability to regulate blood pressure upon standing.
- Neurological disorders: Parkinson’s disease, multiple system atrophy, or diabetic neuropathy can impair autonomic function.
- Cardiovascular issues: Arrhythmias, heart failure, or valve problems limit cardiac output.
- Medication side effects: Diuretics, antihypertensives, antidepressants, and Parkinson’s drugs can exacerbate postural drops.
- Anemia or low blood sugar: Both reduce oxygen-carrying capacity or energy supply to the brain.
A key distinction is duration. Normal orthostatic dizziness lasts less than 10 seconds and resolves without intervention. If symptoms persist beyond 30 seconds, involve fainting (syncope), chest pain, palpitations, or confusion, further evaluation is essential.
Red Flags That Warrant Medical Evaluation
| Symptom | Normal Response | Potential Concern |
|---|---|---|
| Dizziness duration | Less than 10 seconds | More than 30 seconds or recurring daily |
| Fainting (syncope) | Never occurred | One or more episodes |
| Associated symptoms | None or mild lightheadedness | Chest pain, shortness of breath, palpitations |
| Frequency | Occasional, situational | Daily or multiple times per day |
| Medication use | None affecting blood pressure | Taking diuretics, alpha-blockers, or opioids |
Mini Case Study: Recognizing a Pattern
Sarah, a 62-year-old office worker, began noticing frequent dizziness when standing from her desk chair. Initially, she dismissed it as fatigue. Over several weeks, however, the episodes became more intense—sometimes lasting nearly a minute and accompanied by nausea. She also felt unusually tired and had started drinking more water without relief.
After fainting once while getting out of the shower, Sarah consulted her doctor. Blood tests revealed mild anemia, and a medication review showed her blood pressure pill—a long-standing regimen—had recently been increased. Further testing confirmed significant orthostatic hypotension: her systolic pressure dropped 32 mmHg upon standing.
Her treatment involved adjusting her medication dosage, increasing salt and fluid intake under supervision, and adopting slow positional changes. Within two weeks, her symptoms improved dramatically. This case illustrates how seemingly minor symptoms can escalate and how simple interventions, guided by proper diagnosis, make a significant difference.
Step-by-Step Guide to Reduce Dizziness When Standing
If you frequently feel dizzy upon standing, these steps can help minimize episodes and improve stability:
- Move slowly: When rising from bed or a chair, sit on the edge for 10–15 seconds before standing.
- Stay hydrated: Aim for 6–8 glasses of water daily, more in hot weather or during exercise.
- Review medications: Ask your doctor if any prescriptions could contribute to low blood pressure.
- Boost electrolytes: In some cases, adding modest amounts of salt (if not contraindicated) supports blood volume.
- Exercise regularly: Aerobic activity improves circulation and autonomic control.
- Wear compression stockings: These help prevent blood pooling in the legs, especially beneficial for those with chronic symptoms.
- Avoid large meals: Big meals divert blood to the digestive tract, increasing postural drop risk.
- Monitor blood pressure: Check readings at home while lying down and immediately after standing to track changes.
Checklist: What You Can Do Today
Use this actionable checklist to assess and manage your dizziness:
- ✅ Stand up slowly—pause after sitting or lying down.
- ✅ Drink water consistently throughout the day.
- ✅ Review all medications with your healthcare provider.
- ✅ Track symptoms in a journal (frequency, timing, severity).
- ✅ Avoid alcohol, which can worsen blood pressure instability.
- ✅ Eat smaller, balanced meals instead of heavy ones.
- ✅ Consider wearing waist-high compression garments if advised.
- ✅ Schedule a check-up if dizziness persists beyond a few weeks.
FAQ: Common Questions About Orthostatic Dizziness
Can dehydration cause dizziness when standing up?
Yes. Dehydration reduces blood volume, making it harder for your body to maintain blood pressure when upright. Even mild dehydration—such as skipping water for several hours—can trigger lightheadedness. Drinking fluids, especially with electrolytes, often resolves the issue quickly.
Is dizziness when standing up a sign of low iron?
It can be. Iron-deficiency anemia reduces hemoglobin levels, impairing oxygen delivery to the brain. People with anemia often report fatigue, paleness, shortness of breath, and orthostatic dizziness. A simple blood test can confirm iron status and guide treatment.
Why do I feel dizzy when standing up after using the bathroom?
This is common, especially at night. Straining during urination or bowel movements can stimulate the vagus nerve, temporarily lowering heart rate and blood pressure (a vasovagal response). Combine this with a sudden stand-up motion, and dizziness becomes more likely. Moving slowly and avoiding forceful straining helps prevent it.
Conclusion: Listen to Your Body, Take Smart Steps
Feeling dizzy when standing up too fast is usually a fleeting, normal reaction caused by a brief delay in your body’s blood pressure regulation. For most people, simple lifestyle adjustments—like rising slowly, staying hydrated, and reviewing medications—are enough to keep symptoms at bay.
But your body uses dizziness as a signal. Recurrent or severe episodes shouldn’t be ignored. They may reflect dehydration, medication side effects, or more complex health conditions that benefit from early detection and management.
Understanding the difference between normal physiology and a warning sign empowers you to act wisely. Whether it’s adjusting your morning routine or scheduling a doctor’s visit, small steps today can prevent falls, injuries, and unnecessary anxiety tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?