Standing up quickly and suddenly feeling lightheaded or unsteady is a surprisingly common experience—so common that many people dismiss it as normal. But while occasional dizziness upon rising may not be cause for alarm, frequent or severe episodes can signal an underlying health issue. Understanding the science behind this sensation, its potential causes, and knowing when it’s time to consult a medical professional can help protect your long-term well-being.
This article explores the physiological mechanisms behind orthostatic dizziness, identifies risk factors and conditions associated with it, and provides clear guidance on when to seek medical attention.
The Science Behind Dizziness When Standing Up Fast
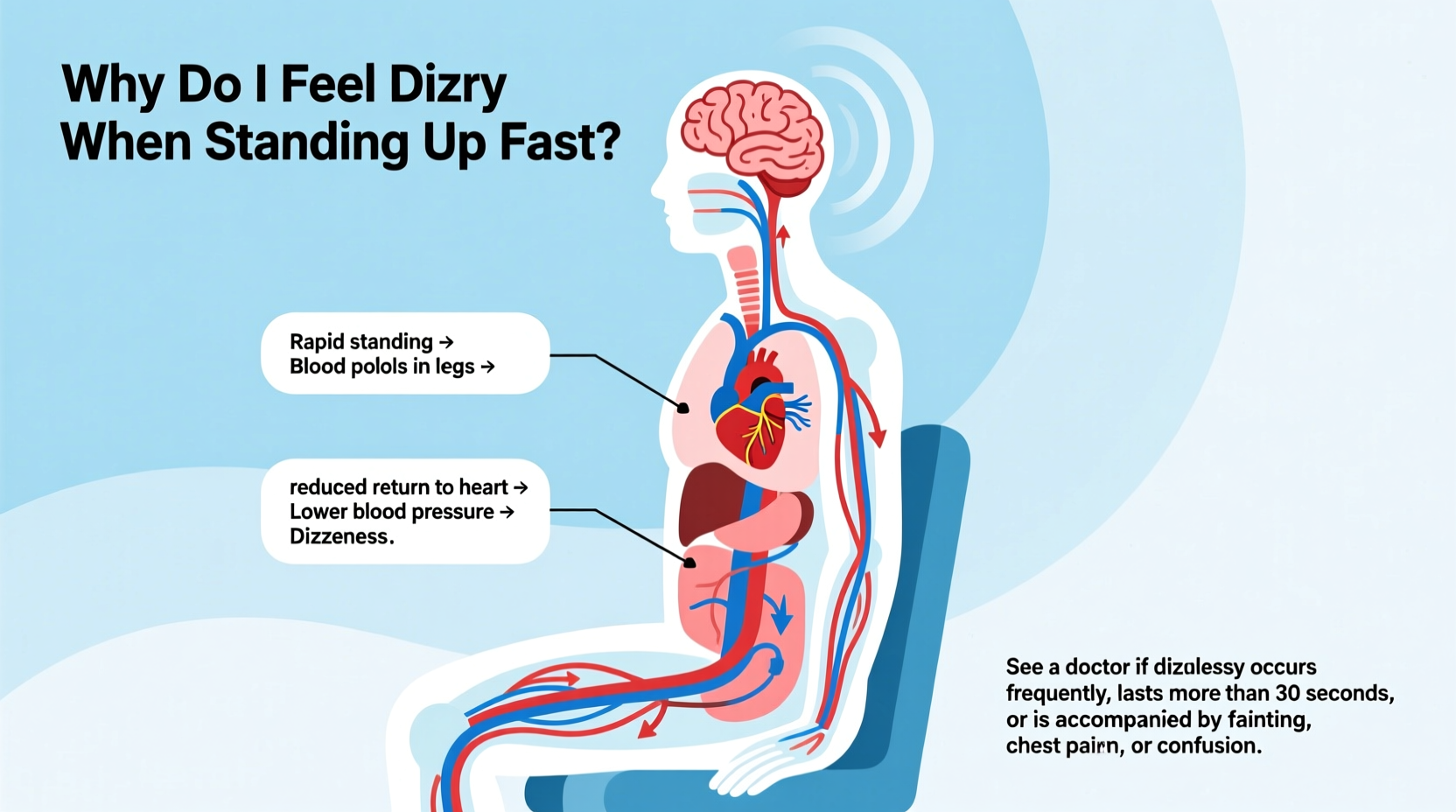
When you stand up from a sitting or lying position, gravity pulls blood downward into your legs and abdomen. This temporary pooling reduces the amount of blood returning to your heart and brain, which can lead to a brief drop in blood pressure. In response, your autonomic nervous system normally compensates by increasing heart rate and constricting blood vessels to maintain adequate cerebral perfusion—the flow of oxygen-rich blood to the brain.
If this regulatory system fails to respond quickly enough, even for a few seconds, you may experience symptoms like:
- Lightheadedness
- Blurred vision
- Tunnel vision
- Nausea
- A feeling of faintness or near-fainting
This condition is known medically as **orthostatic hypotension** (or postural hypotension), defined as a drop of at least 20 mm Hg in systolic blood pressure or 10 mm Hg in diastolic pressure within three minutes of standing.
“Orthostatic dizziness isn’t just ‘getting up too fast’—it reflects how well your cardiovascular and nervous systems are communicating under stress.” — Dr. Lena Patel, Neurologist and Autonomic Specialist
Common Causes of Orthostatic Dizziness
Several factors can impair your body's ability to regulate blood pressure during positional changes. Some are benign and easily corrected; others point to chronic or serious conditions.
Dehydration
Insufficient fluid intake reduces blood volume, making it harder for your body to maintain pressure when upright. Even mild dehydration—common after exercise, alcohol consumption, or illness—can trigger dizziness.
Medications
Certain drugs affect blood pressure regulation. These include:
- Diuretics (“water pills”)
- Alpha-blockers and beta-blockers (used for hypertension)
- Antidepressants (especially tricyclics)
- Parkinson’s disease medications
- Some erectile dysfunction drugs
Aging and Reduced Vascular Elasticity
As we age, blood vessels lose some of their responsiveness, and the baroreceptor reflex—which detects pressure changes—becomes slower. This makes older adults more prone to orthostatic drops, especially if they’re sedentary or have preexisting heart conditions.
Low Blood Sugar (Hypoglycemia)
While less directly linked than blood pressure issues, low glucose levels can contribute to dizziness, weakness, and confusion when standing, particularly in people with diabetes or those skipping meals.
Neurological Conditions
Diseases that damage the autonomic nervous system interfere with the body’s automatic adjustments. Examples include:
- Parkinson’s disease
- Multiple system atrophy (MSA)
- Diabetic neuropathy
- Autoimmune autonomic ganglionopathy
Heart Conditions
Arrhythmias, heart valve problems, or congestive heart failure can reduce cardiac output, limiting the heart’s ability to compensate for posture changes.
When Dizziness Might Signal Something Serious
Occasional lightheadedness after standing quickly is usually harmless. However, recurrent or worsening symptoms—especially when accompanied by other warning signs—may indicate a need for medical evaluation.
Symptoms That Warrant Medical Attention
Seek prompt care if dizziness when standing is paired with any of the following:
- Frequent falls or near-falls
- Chest pain or palpitations
- Shortness of breath
- Confusion or memory lapses
- Fainting (syncope)
- Double vision or slurred speech
- Weakness in limbs
These could suggest cardiovascular disease, neurological disorders, or severe autonomic dysfunction.
Risks of Ignoring Chronic Orthostatic Hypotension
Left untreated, persistent orthostatic hypotension increases the risk of:
- Fractures due to falls
- Cognitive decline (due to repeated cerebral hypoperfusion)
- Increased hospitalization rates in elderly patients
A study published in *Neurology* found that older adults with orthostatic hypotension had a 54% higher risk of developing dementia over 10 years compared to those without the condition.
Diagnostic Process: What to Expect at the Doctor
If your dizziness is frequent or concerning, your doctor will likely begin with a detailed history and physical exam. They’ll ask about:
- Frequency and duration of symptoms
- Timing relative to meals, activity, or medication
- Associated symptoms like fatigue or tremors
- Family history of neurological or heart disease
Common Diagnostic Tests
| Test | Purpose | What It Involves |
|---|---|---|
| Orthostatic Vital Signs | Measure BP and pulse lying, sitting, and standing | Blood pressure checked every minute for 3 minutes after standing |
| Electrocardiogram (ECG) | Check heart rhythm and electrical activity | Non-invasive test using chest electrodes |
| Tilt Table Test | Evaluate autonomic response under controlled conditions | Lie on a table tilted upward while vitals are monitored |
| Blood Tests | Rule out anemia, electrolyte imbalance, diabetes | Standard lab draw for CBC, glucose, kidney function |
| Autonomic Function Testing | Assess nervous system control of BP and HR | Specialized tests including Valsalva maneuver, deep breathing |
In some cases, referral to a cardiologist, neurologist, or autonomic specialist may be necessary for advanced testing.
Step-by-Step Guide to Managing and Preventing Dizziness
You can often reduce or eliminate orthostatic dizziness through lifestyle modifications and careful monitoring. Follow this practical timeline to assess and improve your condition:
- Week 1: Track Symptoms
Keep a daily log noting when dizziness occurs, what you were doing, and any triggers (e.g., heat, dehydration, medication timing). - Week 2: Optimize Hydration and Salt Intake
Drink 1.5–2 liters of water daily. Unless contraindicated (e.g., heart failure), add moderate salt to meals—consult your doctor first. - Week 3: Review Medications
Bring all prescriptions and supplements to your doctor. Ask whether any could be contributing to low blood pressure. - Week 4: Improve Postural Habits
Practice “sit-stand pauses”: After lying down, sit at the edge of the bed for 30 seconds before standing. Avoid sudden movements. - Ongoing: Exercise Regularly
Engage in lower-body resistance training and aerobic activity to improve circulation and vascular tone. Swimming and recumbent biking are excellent choices for those prone to dizziness.
Compression Stockings
Wearing waist-high compression stockings (20–30 mm Hg) can help prevent blood from pooling in the legs. They’re especially effective for people with venous insufficiency or prolonged standing.
Real-Life Example: Maria’s Experience
Maria, a 68-year-old retired teacher, began experiencing frequent dizziness when getting out of bed. At first, she assumed it was just part of aging. But after nearly falling twice in one week, she scheduled a visit with her primary care physician.
Her doctor measured her blood pressure lying down: 128/82 mm Hg. Within two minutes of standing, it dropped to 96/60 mm Hg—with her heart rate barely increasing. Further testing revealed she had autonomic neuropathy secondary to long-standing type 2 diabetes.
With adjustments to her medications, increased fluid intake, and wearing compression garments, Maria reduced her dizziness significantly within six weeks. More importantly, addressing the root cause helped slow progression of her nerve complications.
Her case illustrates how early intervention can prevent dangerous outcomes—and how seemingly minor symptoms deserve investigation.
Do’s and Don’ts: Quick Reference Checklist
| Do’s | Don’ts |
|---|---|
| Stay well-hydrated throughout the day | Stand up abruptly from lying or seated positions |
| Rise slowly—pause before standing | Ignore repeated episodes of lightheadedness |
| Review medications with your doctor annually | Self-adjust blood pressure or heart medications |
| Exercise regularly to support circulation | Skip meals or go long periods without eating |
| Use compression stockings if recommended | Dismiss symptoms just because you’re “getting older” |
Frequently Asked Questions
Is it normal to feel dizzy every time I stand up?
No. While occasional dizziness may happen to anyone, feeling lightheaded every time you stand is not considered normal. It suggests your body isn't adjusting properly to posture changes and should be evaluated—especially if it happens daily or worsens over time.
Can anxiety cause dizziness when standing?
Anxiety itself doesn’t typically cause true orthostatic hypotension, but it can amplify sensations of dizziness. Hyperventilation during anxiety attacks alters blood CO₂ levels, which may cause lightheadedness that mimics orthostatic symptoms. A healthcare provider can differentiate between psychological and physiological causes.
How can I test myself at home for orthostatic hypotension?
You can perform a basic self-check:
1. Lie down for 5 minutes.
2. Measure your blood pressure and pulse.
3. Stand up slowly and remain still.
4. Recheck BP and pulse after 1 and 3 minutes.
If your systolic pressure drops by 20 points or more, or you feel symptomatic, consult your doctor.
Conclusion: Listen to Your Body, Act Early
Dizziness when standing up fast is more than just an inconvenience—it’s a signal from your body that something may be off in its internal balancing act. While many cases stem from simple, correctable causes like dehydration or medication side effects, others point to deeper cardiovascular or neurological concerns.
The key is not to normalize symptoms simply because they’re common. By paying attention to patterns, making smart lifestyle adjustments, and seeking timely medical advice, you can prevent complications and maintain better balance and independence—especially as you age.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?