Standing up quickly and suddenly feeling lightheaded or unsteady isn’t just an odd sensation—it’s your body reacting to a rapid shift in blood flow. This common experience, often dismissed as trivial, may actually be a sign of orthostatic hypotension. While occasional dizziness upon rising is normal for many, frequent or severe episodes can indicate underlying health concerns. Understanding why this happens, what factors contribute to it, and how to manage it empowers you to take control of your well-being.
What Is Orthostatic Hypotension?
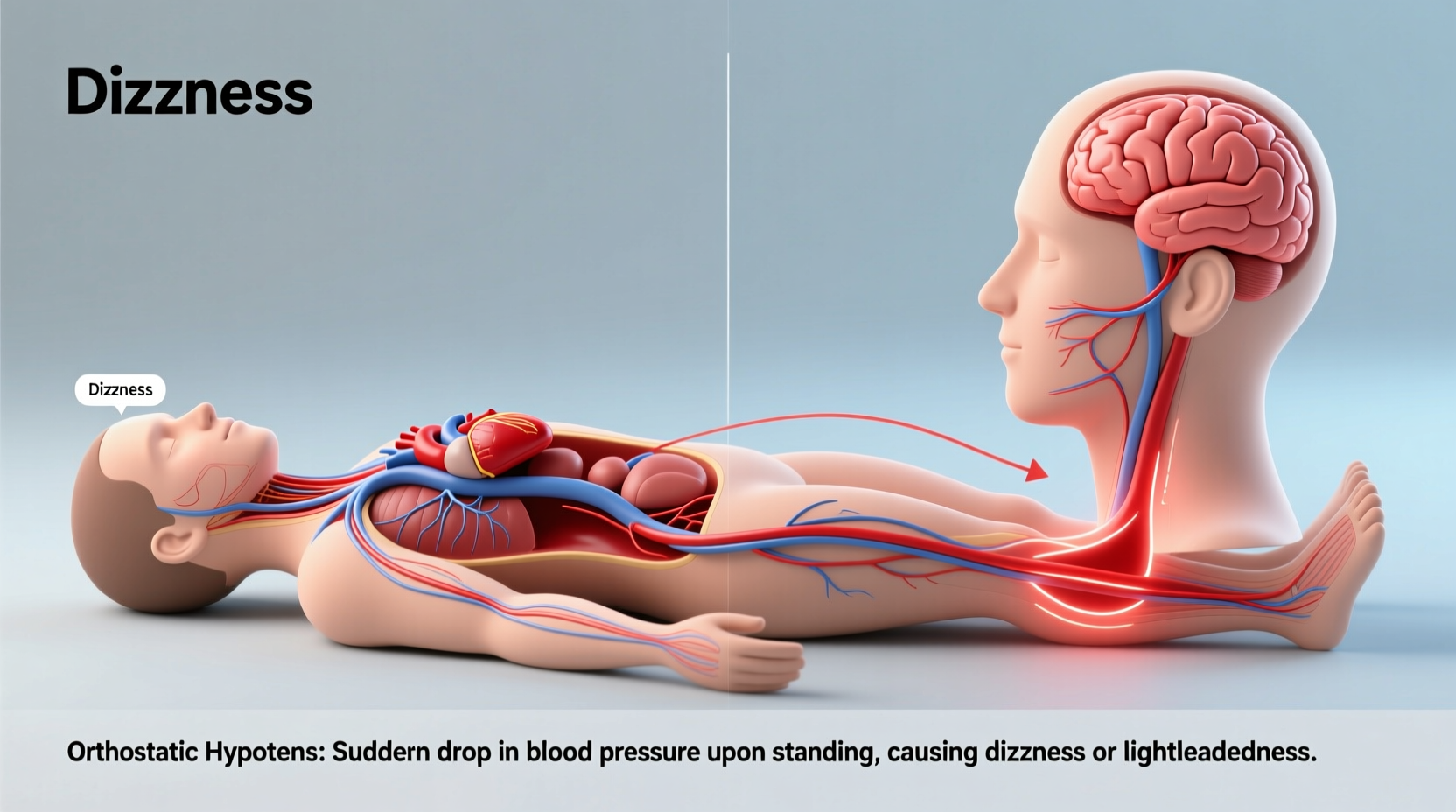
Orthostatic hypotension—also known as postural hypotension—is a condition where your blood pressure drops significantly when you stand up from a sitting or lying position. The term \"orthostatic\" comes from the Greek word for “standing upright,” and \"hypotension\" means low blood pressure. When this drop occurs, your brain temporarily receives less oxygen-rich blood, leading to dizziness, lightheadedness, blurred vision, or even fainting.
The American Heart Association defines orthostatic hypotension as a decrease in systolic blood pressure of at least 20 mm Hg or a reduction in diastolic pressure of 10 mm Hg within three minutes of standing. This physiological response is more than just a brief head rush; it reflects how efficiently your circulatory and nervous systems regulate blood flow during positional changes.
How Your Body Normally Responds to Standing Up
When you stand, gravity pulls blood into your legs and abdomen. To compensate, your autonomic nervous system triggers several adjustments: your heart rate increases slightly, blood vessels constrict, and hormones like norepinephrine help maintain adequate blood pressure. These reflexes ensure that enough blood reaches your brain without interruption.
In individuals with orthostatic hypotension, these mechanisms don’t respond quickly or effectively enough. The delay or failure in vasoconstriction and cardiac adjustment leads to reduced cerebral perfusion—the medical term for blood delivery to the brain—resulting in transient neurological symptoms.
Common Causes and Risk Factors
Orthostatic hypotension doesn’t occur in isolation. It’s typically the result of one or more contributing factors affecting cardiovascular regulation, hydration status, or neurological function. Some causes are temporary and reversible, while others point to chronic conditions requiring medical evaluation.
Dehydration
Insufficient fluid intake reduces blood volume, making it harder for your body to maintain pressure when upright. Even mild dehydration from inadequate water consumption, excessive sweating, vomiting, or diarrhea can trigger symptoms.
Medications
Certain drugs are notorious for lowering blood pressure as a side effect. Common culprits include:
- Diuretics (water pills)
- Alpha-blockers used for high blood pressure or prostate issues
- Antidepressants, especially tricyclics
- Parkinson’s disease medications
- Heart medications such as beta-blockers and vasodilators
Aging and Autonomic Dysfunction
As people age, the body's ability to regulate blood pressure diminishes. The baroreceptor reflex—the system responsible for detecting and correcting blood pressure changes—becomes less responsive. Older adults are therefore more prone to orthostatic drops, particularly if they have pre-existing vascular stiffness or neuropathy.
Underlying Medical Conditions
Several diseases interfere with autonomic control or blood volume regulation:
- Diabetes: Can damage nerves involved in blood pressure control (autonomic neuropathy).
- Parkinson’s disease: Affects both motor function and autonomic regulation.
- Heart problems: Arrhythmias, heart failure, or valve disorders impair cardiac output.
- Anemia: Reduces oxygen-carrying capacity, worsening symptoms of poor perfusion.
- Adrenal insufficiency: Low cortisol levels affect sodium retention and vascular tone.
“Orthostatic hypotension is not just a nuisance—it can be a warning sign of autonomic dysfunction or cardiovascular compromise.” — Dr. Laura Nguyen, Neurologist and Autonomic Specialist
Symptoms and When to Seek Help
Dizziness upon standing is the hallmark symptom, but orthostatic hypotension can manifest in various ways:
- Lightheadedness or feeling faint
- Blurred or tunnel vision
- Nausea
- Weakness or fatigue
- Confusion or difficulty concentrating
- Fainting (syncope)
Symptoms usually begin within seconds to a few minutes after standing and resolve quickly once seated or lying down. However, recurrent episodes increase the risk of falls, especially in older adults. According to the National Institute on Aging, falls related to orthostatic hypotension contribute significantly to injury and hospitalization in seniors.
Red Flags That Warrant Medical Evaluation
While isolated incidents may not be concerning, persistent or worsening symptoms should prompt a visit to your healthcare provider. Seek immediate attention if you experience:
- Frequent fainting spells
- Chest pain or palpitations during episodes
- Shortness of breath
- Neurological symptoms like slurred speech or limb weakness
- Symptoms that interfere with daily activities
Diagnosis and Testing Methods
Diagnosing orthostatic hypotension involves a combination of clinical history, physical examination, and objective measurements. Your doctor will likely perform a simple bedside test called the orthostatic vital signs assessment.
Step-by-Step Diagnostic Process
- You lie down for 5 minutes while your blood pressure and heart rate are recorded.
- You stand up, and readings are taken again at 1 minute and 3 minutes.
- A drop meeting the criteria (≥20 mm Hg systolic or ≥10 mm Hg diastolic) confirms the diagnosis.
In some cases, further testing may be needed:
- Tilt table test: Monitors BP and heart rate while you’re strapped to a table that tilts from horizontal to vertical.
- Autonomic function tests: Assess how your nervous system controls heart rate and blood pressure.
- Blood tests: Check for anemia, electrolyte imbalances, diabetes, or hormonal disorders.
- Electrocardiogram (ECG) or echocardiogram: Evaluate heart structure and rhythm.
| Test Type | Purpose | What to Expect |
|---|---|---|
| Orthostatic Vital Signs | Measure BP change with posture | Quick, non-invasive; done in clinic |
| Tilt Table Test | Evaluate syncope causes | 30–60 min; may provoke symptoms |
| Blood Work | Identify underlying conditions | Fasting may be required |
| ECG/Echocardiogram | Assess heart function | Painless; uses electrodes or ultrasound |
Prevention and Management Strategies
Managing orthostatic hypotension often begins with lifestyle modifications. Many people find relief through simple, consistent habits that support circulatory stability.
Hydration and Salt Intake
Maintaining adequate fluid volume helps sustain blood pressure. Aim for 6–8 glasses of water daily, more if you're active or live in a hot climate. In some cases, doctors recommend slightly increasing salt intake under supervision—especially for those with low-normal sodium levels—but this should never be done without medical advice, particularly if you have hypertension or kidney disease.
Physical Counterpressure Maneuvers
These techniques help prevent blood pooling in the lower body:
- Flexing leg muscles before and after standing
- Toe raises or marching in place before rising
- Leaning forward slightly when standing
- Wearing compression stockings (typically 20–30 mm Hg)
Medication Review
If you're on medications that lower blood pressure, discuss timing and dosage with your doctor. Sometimes adjusting when you take a pill (e.g., avoiding doses before bedtime or early morning) can reduce symptoms. Never stop or alter medication without professional guidance.
Dietary Considerations
Large meals, especially those high in carbohydrates, can worsen postprandial hypotension—a type of low blood pressure after eating. Opt for smaller, more frequent meals rich in protein and fiber. Limit alcohol, which dilates blood vessels and exacerbates dizziness.
Exercise and Physical Conditioning
Regular aerobic activity improves vascular tone and autonomic responsiveness. Walking, swimming, or cycling for 30 minutes most days enhances circulation and reduces symptom frequency over time. Strength training also supports muscle pump function in the legs.
📋 **Checklist: Daily Habits to Reduce Dizziness When Standing**- ✅ Drink water throughout the day
- ✅ Rise slowly from lying to sitting to standing
- ✅ Perform leg muscle contractions before standing
- ✅ Avoid prolonged standing or hot environments
- ✅ Eat balanced, moderate-sized meals
- ✅ Wear compression stockings if recommended
- ✅ Monitor blood pressure at home if advised
Real-Life Example: Managing Symptoms After Surgery
John, a 68-year-old retiree, began experiencing frequent dizziness after knee replacement surgery. Initially attributing it to pain medication, he continued to feel lightheaded weeks after stopping opioids. His primary care physician performed an orthostatic blood pressure test and found a 28 mm Hg drop in systolic pressure upon standing. Further evaluation revealed mild autonomic dysfunction likely exacerbated by immobility and dehydration during recovery.
With guidance, John increased his fluid intake, started wearing compression socks, and incorporated gentle daily walks. He also adjusted the timing of his blood pressure medication to avoid taking it first thing in the morning. Within six weeks, his symptoms improved dramatically. This case illustrates how multiple factors can converge—and how targeted interventions make a meaningful difference.
Frequently Asked Questions
Is it normal to feel dizzy every time I stand up?
Occasional mild dizziness may be normal, especially if you stand quickly. However, regular or severe dizziness when standing is not something to ignore. It could signal orthostatic hypotension or another health issue and warrants evaluation by a healthcare provider.
Can young people get orthostatic hypotension?
Yes. While more common in older adults, younger individuals—especially those with conditions like POTS (postural orthostatic tachycardia syndrome), eating disorders, or prolonged bed rest—can experience similar symptoms. Dehydration and intense exercise are also common triggers in younger populations.
Does caffeine help with orthostatic hypotension?
Caffeine can cause short-term increases in blood pressure due to its stimulant effects, which might provide temporary relief. However, its diuretic properties may lead to dehydration over time, potentially worsening symptoms. Moderation is key, and reliance on caffeine is not a sustainable solution.
Conclusion: Take Control of Your Stability
Feeling dizzy when standing up too fast is more than just an inconvenience—it’s a signal from your body that something in your circulatory regulation needs attention. Whether due to dehydration, medication side effects, aging, or an underlying condition, orthostatic hypotension is manageable with the right approach. By staying hydrated, moving mindfully, reviewing medications, and seeking medical insight when needed, you can reduce episodes and improve your quality of life.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?