Feeling full after just a few bites of food can be confusing and frustrating. You sit down for a meal with a healthy appetite, only to feel uncomfortably full minutes later—sometimes even before finishing half your plate. This sensation, known as early satiety, is more than just an inconvenience. While it’s occasionally normal, persistent or sudden onset could signal underlying digestive or metabolic issues.
Understanding why this happens—and knowing when it's time to seek medical advice—is essential for maintaining long-term digestive health. This article breaks down the physiological and pathological causes of early satiety, highlights warning signs, and offers practical strategies to manage the condition effectively.
What Is Early Satiety?
Early satiety refers to the feeling of fullness that occurs shortly after starting a meal, often leading to reduced food intake. It differs from general bloating or indigestion because the sensation arises quickly and consistently during meals rather than afterward.
The stomach typically expands to accommodate food, signaling fullness gradually through nerve feedback to the brain. In cases of early satiety, this process is disrupted—either due to mechanical limitations in the stomach or altered signaling pathways.
Common Causes of Feeling Full Quickly
Many factors contribute to early satiety, ranging from lifestyle habits to chronic conditions. Below are the most frequent causes:
- Overeating fiber or fat: High-fiber or high-fat meals slow gastric emptying, increasing the sensation of fullness.
- Dehydration: Drinking too little water can impair digestion and amplify fullness signals.
- Eating too quickly: Rapid eating doesn’t allow time for satiety hormones like leptin to signal the brain.
- Stress and anxiety: The gut-brain axis can trigger premature fullness during emotional distress.
- Pregnancy: Hormonal changes and physical space constraints lead to quicker fullness, especially in the first trimester.
- Medications: Certain drugs—including antidepressants, opioids, and diabetes medications like GLP-1 agonists (e.g., semaglutide)—are designed to promote fullness.
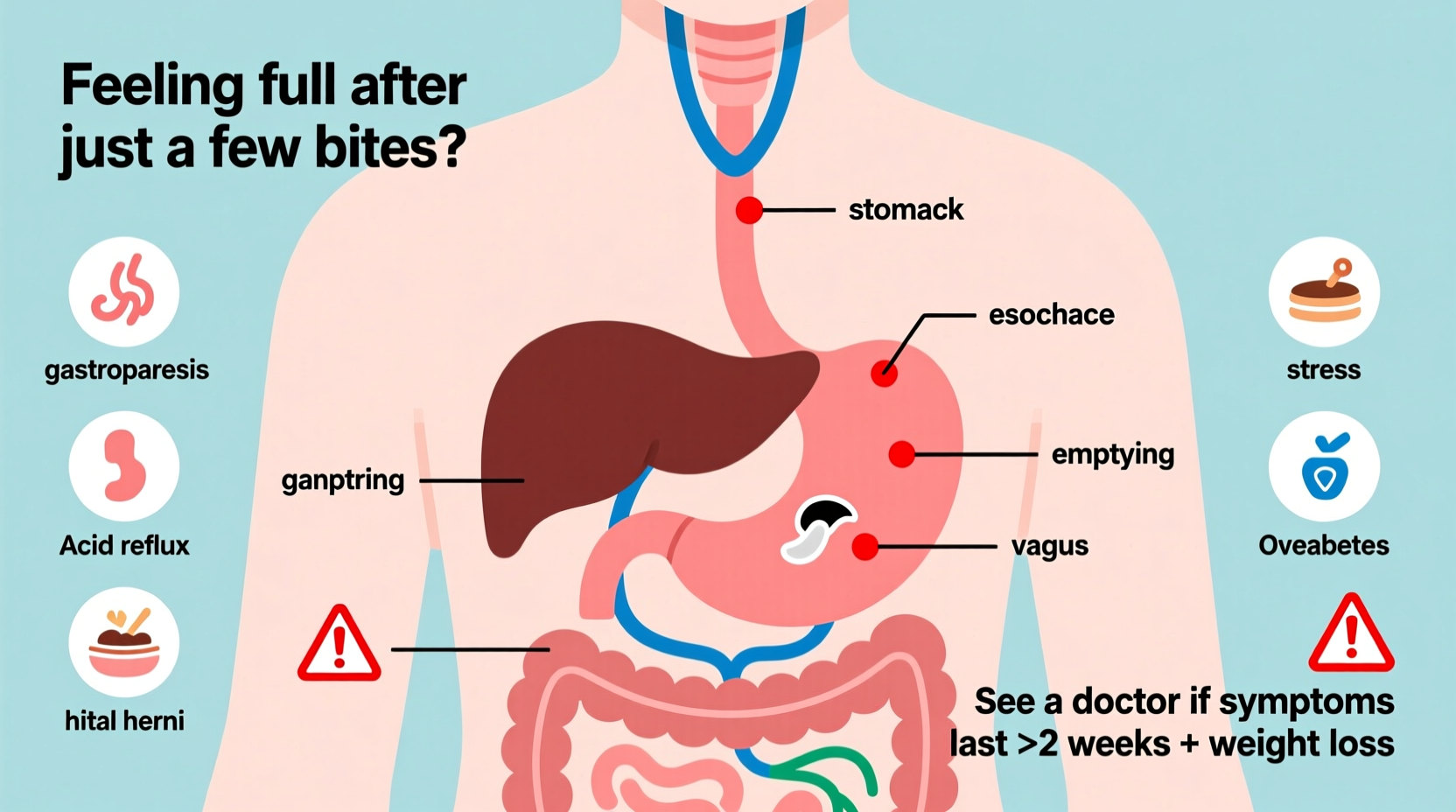
Gastrointestinal Disorders Linked to Early Satiety
When early satiety becomes chronic, it may point to a gastrointestinal disorder. Common conditions include:
- Gastroparesis: A condition where the stomach empties slowly due to nerve damage, often associated with diabetes or post-viral syndromes.
- Peptic ulcers: Sores in the stomach lining or duodenum can cause pain and fullness after minimal food intake.
- Functional dyspepsia: Chronic indigestion without a clear structural cause, marked by upper abdominal discomfort and early fullness.
- Gastritis: Inflammation of the stomach lining, often caused by H. pylori infection or prolonged NSAID use.
- GERD (Gastroesophageal Reflux Disease): Acid reflux can mimic or worsen feelings of fullness, especially if the lower esophageal sphincter is compromised.
When to Worry: Red Flags That Require Medical Attention
Occasional early fullness isn't alarming. However, certain symptoms suggest a need for prompt evaluation by a healthcare provider.
| Symptom | May Indicate | Action |
|---|---|---|
| Unintentional weight loss (5+ lbs in a month) | Malignancy, malabsorption, or chronic inflammation | See a gastroenterologist immediately |
| Nausea or vomiting after most meals | Gastroparesis or bowel obstruction | Seek diagnostic testing (e.g., gastric emptying study) |
| Persistent abdominal pain | Ulcer, pancreatitis, or inflammatory disease | Get endoscopy or imaging |
| Fatigue and pale skin | Anemia from chronic blood loss (e.g., ulcer) | Blood tests and GI workup |
| Difficulty swallowing (dysphagia) | Esophageal stricture or tumor | Urgent endoscopic evaluation needed |
“Persistent early satiety should never be dismissed as ‘just stress’ or ‘getting older.’ It’s a symptom that deserves investigation, especially when paired with weight loss.” — Dr. Lena Torres, Gastroenterology Specialist, Cleveland Clinic
Real-Life Example: Maria’s Experience with Gastroparesis
Maria, a 47-year-old teacher with type 2 diabetes, began noticing she couldn’t finish her breakfast within weeks of adjusting her medication. She attributed it to being “more mindful” of portion sizes—until she started losing weight unintentionally and felt bloated after sipping soup.
After several months of worsening symptoms, she consulted a gastroenterologist. A gastric emptying scan confirmed gastroparesis. With dietary modifications, prokinetic medication, and tighter glucose control, Maria regained her ability to eat regular meals and stabilized her weight.
Her case underscores how easily early satiety can be overlooked—especially when masked by preexisting conditions like diabetes.
Practical Steps to Manage Early Satiety
If you experience frequent early fullness but don’t have red-flag symptoms, consider these evidence-based adjustments:
Step-by-Step Guide to Improving Meal Tolerance
- Slow down while eating: Aim for at least 20 minutes per meal. Chew thoroughly to aid digestion and give satiety signals time to register.
- Reduce fat and fiber temporarily: While both are healthy, they delay gastric emptying. Opt for low-residue options like white rice, boiled potatoes, and lean poultry.
- Avoid carbonated drinks: Gas from sodas or sparkling water increases intra-abdominal pressure and fullness.
- Stay upright after meals: Sit or walk gently for 30–60 minutes to support gastric motility.
- Monitor medication side effects: Review prescriptions with your doctor. Drugs like metformin, exenatide, or tricyclic antidepressants commonly cause fullness.
Checklist: When to See a Doctor
Use this checklist to determine whether your symptoms warrant medical evaluation:
- ✅ Lost weight without trying in the past 1–2 months
- ✅ Feel nauseous or vomit after most meals
- ✅ Experience pain or burning in the upper abdomen regularly
- ✅ Have a history of diabetes, ulcers, or abdominal surgery
- ✅ Notice changes in bowel habits (diarrhea, constipation, black stools)
- ✅ Symptoms persist beyond two weeks despite dietary changes
If you check two or more items, schedule an appointment with your primary care physician or a gastroenterologist.
Frequently Asked Questions
Can anxiety really make me feel full faster?
Yes. Anxiety activates the sympathetic nervous system, which slows digestion and alters gut motility. Many people report stomach discomfort, bloating, and early fullness during periods of high stress. Cognitive behavioral therapy (CBT) and mindfulness practices have been shown to improve functional GI symptoms linked to anxiety.
Is early satiety a sign of cancer?
It can be—but not usually. While stomach or pancreatic cancers may present with early fullness, they’re typically accompanied by other serious symptoms like significant weight loss, jaundice, or persistent vomiting. These cancers are relatively rare. However, any unexplained, progressive fullness lasting more than a few weeks should be evaluated to rule out serious causes.
Do GLP-1 drugs like Ozempic cause permanent changes to hunger?
GLP-1 receptor agonists are designed to enhance satiety and slow gastric emptying. Most effects reverse after discontinuation, though some users report lingering changes in appetite for weeks. There’s no evidence of permanent alteration in hunger signals, but long-term data is still emerging.
Conclusion: Listen to Your Body, But Don’t Ignore Warning Signs
Feeling full quickly isn’t always a cause for concern—especially if it happens occasionally and resolves with simple dietary tweaks. However, when early satiety becomes a pattern, interferes with nutrition, or appears alongside other symptoms, it’s time to take action.
Your digestive system communicates through subtle cues. Pay attention to those signals. Small changes in eating habits can make a big difference, but professional guidance is crucial when symptoms persist. Addressing the root cause early can prevent complications like malnutrition or delayed diagnosis of treatable conditions.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?