Bacterial vaginosis (BV) is the most common vaginal condition among women aged 15 to 44. Unlike yeast infections, which are caused by an overgrowth of fungus, BV results from an imbalance in the natural bacteria that live in the vagina. Many women experience recurrent BV—defined as four or more episodes in a year—leading to frustration, discomfort, and concern about long-term health. Understanding why BV keeps coming back is the first step toward lasting relief.
The good news: while BV is frustratingly persistent for some, it’s highly manageable with the right knowledge and habits. This guide breaks down the science behind recurring BV, identifies key triggers, and offers practical, evidence-based strategies to restore balance and prevent future flare-ups.
Understanding Bacterial Vaginosis: The Science Behind the Imbalance
The vagina hosts a complex ecosystem of bacteria, dominated by beneficial Lactobacillus species. These bacteria produce lactic acid, maintaining a slightly acidic pH (typically between 3.8 and 4.5), which protects against harmful microbes. BV occurs when this balance shifts—Lactobacillus levels drop, and anaerobic bacteria like Gardnerella vaginalis, Prevotella, and Atopobium multiply.
Symptoms often include a thin, grayish-white discharge, a strong “fishy” odor (especially after sex), and sometimes itching or burning. However, up to 50% of women with BV have no noticeable symptoms, making it easy to overlook until complications arise.
Recurrent BV isn’t just bad luck—it’s usually tied to ongoing disruptions in the vaginal environment. Identifying and addressing these factors is crucial for long-term control.
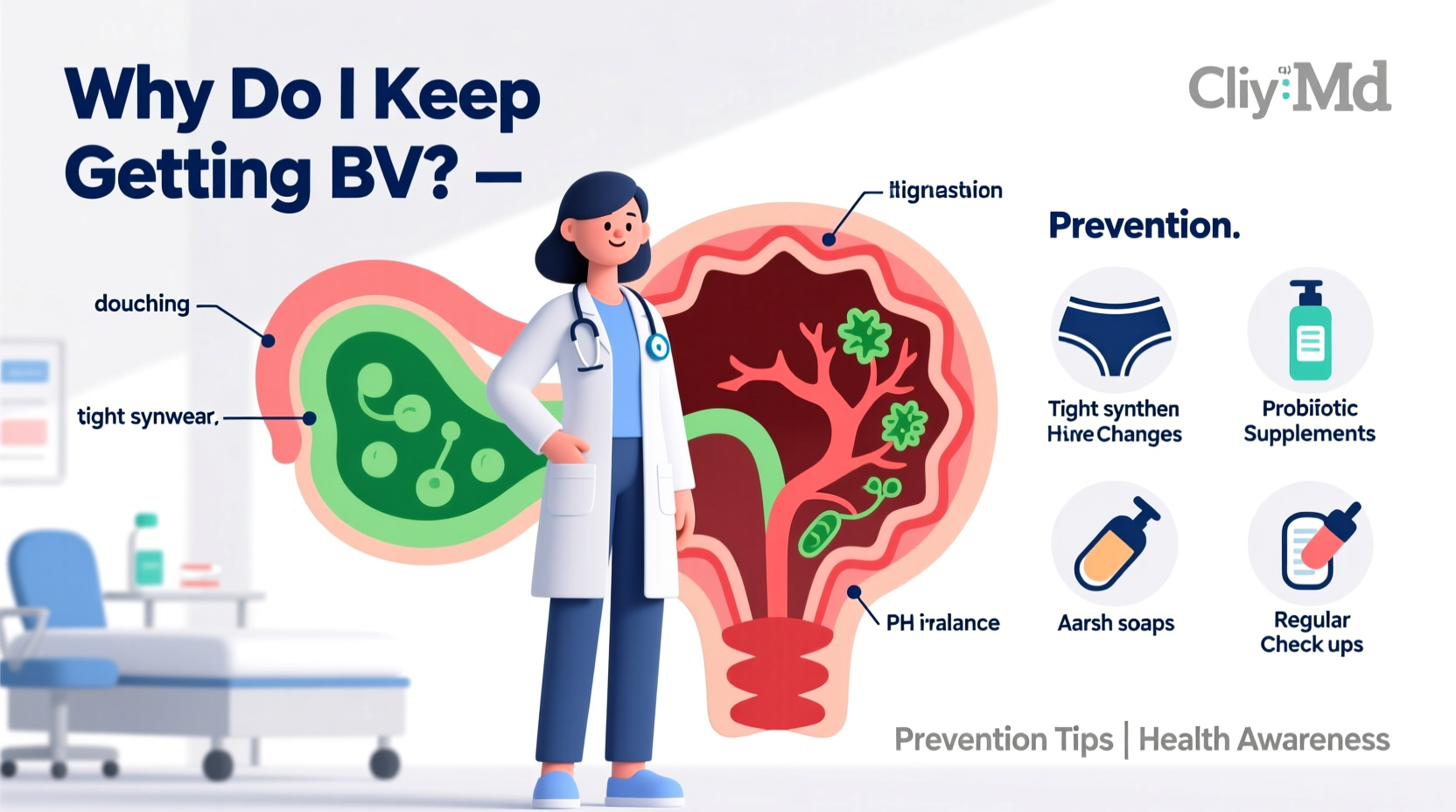
Common Causes of Recurrent BV
Several lifestyle, biological, and behavioral factors can contribute to repeated BV episodes. While not all causes apply to every individual, recognizing patterns can help pinpoint personal triggers.
- Sexual activity: Having a new or multiple sexual partners increases risk, though BV is not classified as a sexually transmitted infection (STI). Semen has a high pH, which can temporarily disrupt vaginal acidity.
- Douching: This practice washes away protective lactobacilli and introduces foreign substances into the vaginal canal, significantly increasing BV risk.
- Hormonal fluctuations: Menstruation, pregnancy, and menopause affect vaginal pH and moisture levels, creating windows of vulnerability.
- Smoking: Nicotine may impair immune function in the genital tract and alter local bacterial communities.
- Intrauterine devices (IUDs): Some studies suggest a slight increase in BV risk among IUD users, possibly due to changes in cervical mucus or minor tissue irritation.
- Antibiotic use: Broad-spectrum antibiotics can kill off good bacteria along with harmful ones, paving the way for BV.
- Poor intimate hygiene: Using scented soaps, wipes, or laundry detergents near the vulva can irritate sensitive skin and disrupt microbial balance.
Prevention Strategies That Actually Work
Preventing recurrent BV requires consistency and attention to daily habits. Medical treatment clears active infections, but long-term wellness depends on sustaining a healthy vaginal environment.
1. Maintain a Healthy Vaginal pH
The ideal vaginal pH is mildly acidic. You can support this balance by:
- Using only warm water or mild, unscented soap on the external vulva (never inside the vagina).
- Choosing period products carefully—opt for cotton tampons and pads without fragrances.
- Urinating and wiping front to back after sex to reduce bacterial transfer.
2. Support Lactobacillus Colonization
Some research suggests that certain probiotics—especially those containing Lactobacillus rhamnosus GR-1 and L. reuteri RC-14—may help restore healthy flora when taken orally or applied vaginally.
“Probiotic supplementation shows promise in reducing recurrence rates, particularly when used alongside conventional therapy.” — Dr. Sarah Thompson, Gynecological Infectious Disease Specialist
3. Practice Safer Sex Habits
While abstinence isn’t necessary, consider these adjustments:
- Use condoms consistently—they help maintain pH stability and reduce exposure to semen and other microbes.
- Limit the number of sexual partners.
- Clean sex toys thoroughly before and after use, and use non-porous materials like silicone with a condom.
4. Wear Breathable Underwear
Tight synthetic fabrics trap moisture, creating a breeding ground for bacteria. Cotton underwear allows airflow and reduces humidity in the genital area.
Step-by-Step Guide to Reducing BV Recurrence
Follow this six-week plan to reset your routine and build sustainable defenses against BV:
- Week 1: Eliminate douching, scented soaps, and feminine sprays. Switch to fragrance-free laundry detergent.
- Week 2: Begin taking a clinically studied vaginal probiotic daily.
- Week 3: Evaluate your underwear choices—replace synthetic fabrics with breathable cotton options.
- Week 4: Start using condoms during sex if not already doing so.
- Week 5: Track your cycle and note any BV symptoms around menstruation or ovulation.
- Week 6: Schedule a gynecologist visit to discuss persistent issues and rule out other conditions.
This gradual approach minimizes overwhelm and helps identify what works best for your body.
Do’s and Don’ts: Quick Reference Table
| Do’s | Don’ts |
|---|---|
| Wash the vulva with water or mild, unscented soap | Use scented wipes, bubble baths, or perfumed lotions |
| Wear cotton underwear and loose-fitting clothes | Wear tight nylon or polyester undergarments |
| Use condoms during sexual activity | Douche or rinse inside the vagina |
| Take a probiotic with proven strains | Smoke cigarettes |
| Change tampons/pads frequently during your period | Use expired or heavily fragranced menstrual products |
Real-Life Example: Maria’s Journey with Recurrent BV
Maria, a 32-year-old teacher, had been battling BV for over two years. She visited her doctor every few months, received antibiotics, and felt temporary relief—but symptoms always returned within weeks. Frustrated, she sought a second opinion.
After reviewing her habits, her provider noticed Maria regularly used scented panty liners and douching products marketed as “freshening” solutions. She also wore tight leggings daily and hadn’t considered switching to cotton underwear.
With guidance, Maria stopped douching, switched to unscented products, started a daily probiotic, and began wearing cotton briefs. Within three months, her BV episodes dropped from quarterly to none. She now manages her vaginal health proactively and shares her story with friends who face similar struggles.
Frequently Asked Questions
Can BV go away on its own?
Occasionally, mild BV may resolve without treatment. However, leaving it untreated increases the risk of complications such as pelvic inflammatory disease (PID), higher susceptibility to STIs (including HIV), and adverse pregnancy outcomes like preterm birth. It’s best to seek diagnosis and treatment.
Is there a link between BV and yeast infections?
Yes—both result from imbalances in vaginal flora, but they involve different organisms. Treating one doesn’t prevent the other. In fact, antibiotic treatment for BV can sometimes trigger a yeast infection by disrupting bacterial balance further. Probiotics may help reduce this risk.
Why do I get BV after my period?
Menstrual blood has a neutral pH (around 7.0), which temporarily raises vaginal pH and creates a favorable environment for anaerobic bacteria. Combined with prolonged exposure to damp tampons or pads, this can trigger BV. Changing products frequently and washing the vulva gently post-period can help.
Final Thoughts: Take Control of Your Vaginal Health
Recurrent BV is more than a nuisance—it’s a signal that something in your routine or biology needs adjustment. While antibiotics are essential for treating active infections, true prevention lies in consistent, informed self-care. By understanding your body’s unique needs and avoiding common pitfalls, you can break the cycle of recurrence.
Every small change—from swapping out scented products to wearing breathable fabrics—adds up. Don’t hesitate to work closely with your healthcare provider, especially if BV continues despite preventive efforts. New treatments, including extended antibiotic regimens and vaginal pH stabilizers, are available for chronic cases.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?