It’s no longer rare to hear someone say, “I’ve had COVID three times.” What was once a novel virus has become a recurring presence in many lives. While initial infection brought widespread fear and uncertainty, the growing number of people reporting multiple bouts of illness raises a critical question: Why do I keep getting COVID? The answer lies in a combination of viral evolution, immune dynamics, behavior, and environment. Understanding the mechanics behind repeat infections is key to making informed decisions about personal health and long-term protection.
The Science Behind Repeat Infections
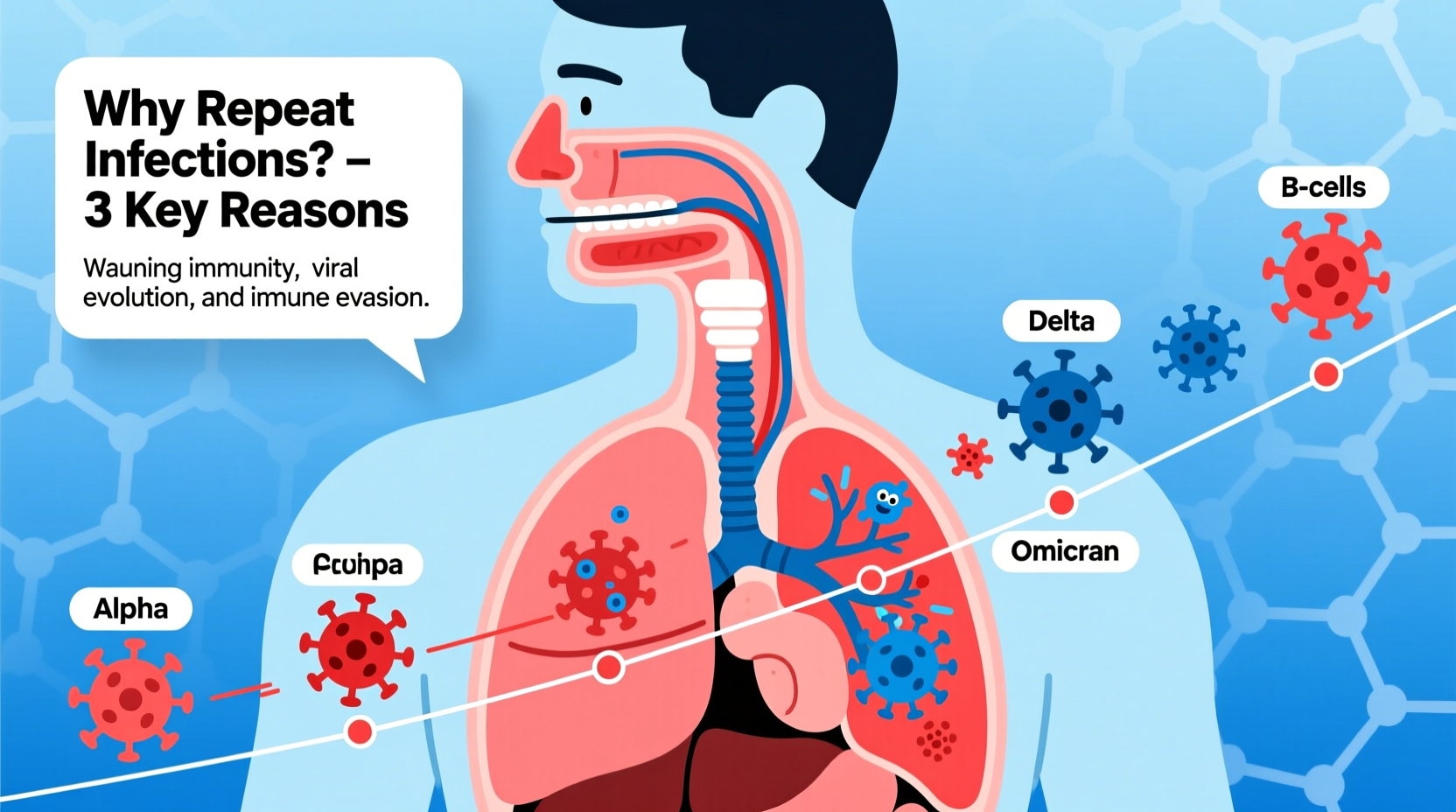
When SARS-CoV-2 first emerged, scientists believed that natural infection would confer lasting immunity—similar to other coronaviruses like those causing the common cold. However, it quickly became evident that immunity from both infection and vaccination wanes over time. Moreover, the virus has evolved rapidly, producing variants that can partially evade immune defenses.
Repeat infections occur when a person contracts the virus again after recovering from a prior bout. This doesn’t necessarily mean their immune system failed—it may simply have been overwhelmed by a new variant or weakened due to time, stress, or age. The Centers for Disease Control and Prevention (CDC) officially recognizes reinfection as possible and increasingly common, especially since the emergence of Omicron subvariants such as BA.5, XBB, and JN.1.
Immunity post-infection typically offers strong protection for 3–6 months, but this varies widely between individuals. Factors like age, underlying health conditions, and the specific variant involved influence how long protection lasts.
Variants and Immune Evasion
One of the primary reasons for repeat infections is the virus's ability to mutate. Each major variant introduces changes to the spike protein—the part of the virus targeted by vaccines and prior immunity. These changes allow newer strains to bypass antibodies generated from previous infections or vaccinations.
For example, Omicron differed significantly from the original Wuhan strain and earlier variants like Delta. Its numerous mutations enabled it to spread more efficiently and infect people who were previously immune. Subsequent subvariants have continued this trend, evolving to be more transmissible and better at escaping neutralizing antibodies.
This constant evolution means that immunity becomes less effective over time—not because the body \"forgets\" the virus, but because the virus looks different enough to slip past existing defenses.
“Viruses evolve to survive. SARS-CoV-2 is no exception. Its rapid mutation rate allows it to stay one step ahead of our immune responses.” — Dr. Angela Rasmussen, Virologist, University of Saskatchewan
Risk Factors That Increase Likelihood of Reinfection
Not everyone experiences repeated infections equally. Certain behaviors and biological factors increase susceptibility:
- Frequent exposure: Working in healthcare, public transit, schools, or crowded indoor spaces increases contact with infected individuals.
- Weakened immune function: Chronic illnesses (e.g., diabetes, HIV), immunosuppressive treatments, or aging reduce the body’s ability to fight off reinfection.
- Lack of updated vaccination: Those who haven’t received bivalent or monovalent boosters tailored to newer variants are at higher risk.
- Indoor ventilation: Poorly ventilated environments allow viral particles to accumulate, increasing transmission risk.
- Behavioral habits: Skipping masks, avoiding testing, or returning to work too soon after recovery contribute to cycles of infection.
Real-Life Scenario: A Teacher’s Experience
Sarah, a middle school teacher in Chicago, contracted her first case of COVID in early 2022 during the Omicron wave. She recovered within ten days and assumed she’d be protected for several months. By late summer, she tested positive again—this time with few symptoms. In spring 2023, despite being vaccinated and boosted, she caught another variant after a family gathering. Then, in winter 2024, she fell ill a fourth time.
Sarah’s situation reflects a growing pattern among frontline workers and caregivers. Her repeated exposures in classrooms and social settings, combined with evolving variants, made reinfection almost inevitable—even with precautions. However, each subsequent illness was milder than the last, suggesting her immune system was learning and adapting, even if it couldn’t always prevent infection.
How Immunity Works—and Why It Falters
The human immune system responds to viruses through two main arms: innate and adaptive immunity. After infection, B cells produce antibodies, while T cells help destroy infected cells and regulate the response. Over time, memory B and T cells remain, ready to react faster upon re-exposure.
However, antibody levels naturally decline within months. While memory cells persist, they may not act quickly enough to stop infection entirely—especially against a fast-replicating, mutated variant. This results in a breakthrough infection, though often with reduced severity.
Vaccination enhances this process by priming the immune system without causing disease. Updated boosters train the body to recognize current circulating strains, improving protection against both infection and severe outcomes.
| Factor | Impact on Reinfection Risk |
|---|---|
| Time since last infection | Risk increases after 3–6 months |
| Vaccination status | Boosters reduce risk by up to 70% |
| Viral variant | Newer variants (e.g., JN.1) more likely to cause reinfection |
| Indoor crowding | Doubles exposure likelihood in poorly ventilated areas |
| Pre-existing immunity | Hybrid immunity (infection + vaccine) offers strongest protection |
Practical Steps to Reduce Your Risk
You can’t eliminate the risk of catching COVID again, but you can significantly lower it. Here’s a checklist of evidence-based actions:
- Stay up to date with recommended boosters (including XBB.1.5 and JN.1-targeted vaccines)
- Wear a high-quality mask (N95/KF94) in crowded indoor settings
- Improve home and workspace ventilation (open windows, use HEPA filters)
- Test early when symptoms appear or after known exposure
- Avoid close contact with infected individuals for at least five days
- Maintain good sleep, nutrition, and stress management to support immune function
When and How to Test
Early detection is crucial. If you develop symptoms like sore throat, cough, fatigue, or fever—or have been exposed—take an at-home antigen test. False negatives are common in the first 1–2 days, so repeat testing 24–48 hours later increases accuracy. Positive results should be followed by isolation to protect others.
Consider serial testing even if asymptomatic after exposure, especially before visiting vulnerable loved ones. The CDC recommends isolating for at least five days and wearing a mask around others for ten days post-infection.
Frequently Asked Questions
Can I get COVID more than three times?
Yes. There is no biological limit to how many times you can be infected. With ongoing circulation of the virus and continuous evolution, multiple infections over years are expected. However, hybrid immunity (from vaccines and prior infections) tends to make later infections less severe.
Does each infection weaken my immune system?
There is no conclusive evidence that mild reinfections permanently impair immunity. However, some individuals report lingering symptoms or increased fatigue after multiple bouts, a phenomenon seen in long COVID cases. Maintaining overall health supports resilience.
Am I contagious if I’ve had it before?
Absolutely. Prior infection does not prevent you from spreading the virus. You are most contagious in the first few days after symptoms begin—or from day zero if asymptomatic. Always take precautions when infected, regardless of history.
Conclusion: Staying Ahead of the Virus
Repeat COVID infections are not a sign of personal failure or weak immunity—they reflect the reality of living with a highly transmissible, constantly changing virus. The goal is no longer to avoid infection at all costs, but to minimize harm through smart prevention and timely care.
By staying informed, keeping vaccinations current, and adopting sustainable protective habits, you can reduce how often you get sick and ensure that when you do, the impact is minimal. Long-term coexistence with SARS-CoV-2 requires vigilance, not fear. Use the knowledge in this guide to protect yourself and your community—one practical step at a time.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?