Suddenly catching a whiff of smoke or burning plastic—only to realize no one else smells it and there’s no source—can be unsettling. These experiences, known as phantom smells or olfactory hallucinations, affect more people than you might think. While occasional episodes may not be alarming, persistent or recurring phantom burning odors can signal underlying health conditions. Understanding why this happens is the first step toward addressing the cause and finding relief.
What Are Phantom Smells?
Phantom smells, medically termed *phantosmia*, occur when a person perceives an odor that isn’t actually present. The sensation is real to the individual, even though no external stimulus exists. These smells vary widely but often include unpleasant scents like burning rubber, rotting food, chemicals, or cigarette smoke. Burning smells are among the most commonly reported.
Phantosmia can affect one or both nostrils and may last seconds, minutes, or persist for hours. It can appear suddenly or develop gradually. In some cases, it occurs alongside distortions in normal smell perception (*parosmia*), where familiar scents become distorted or foul.
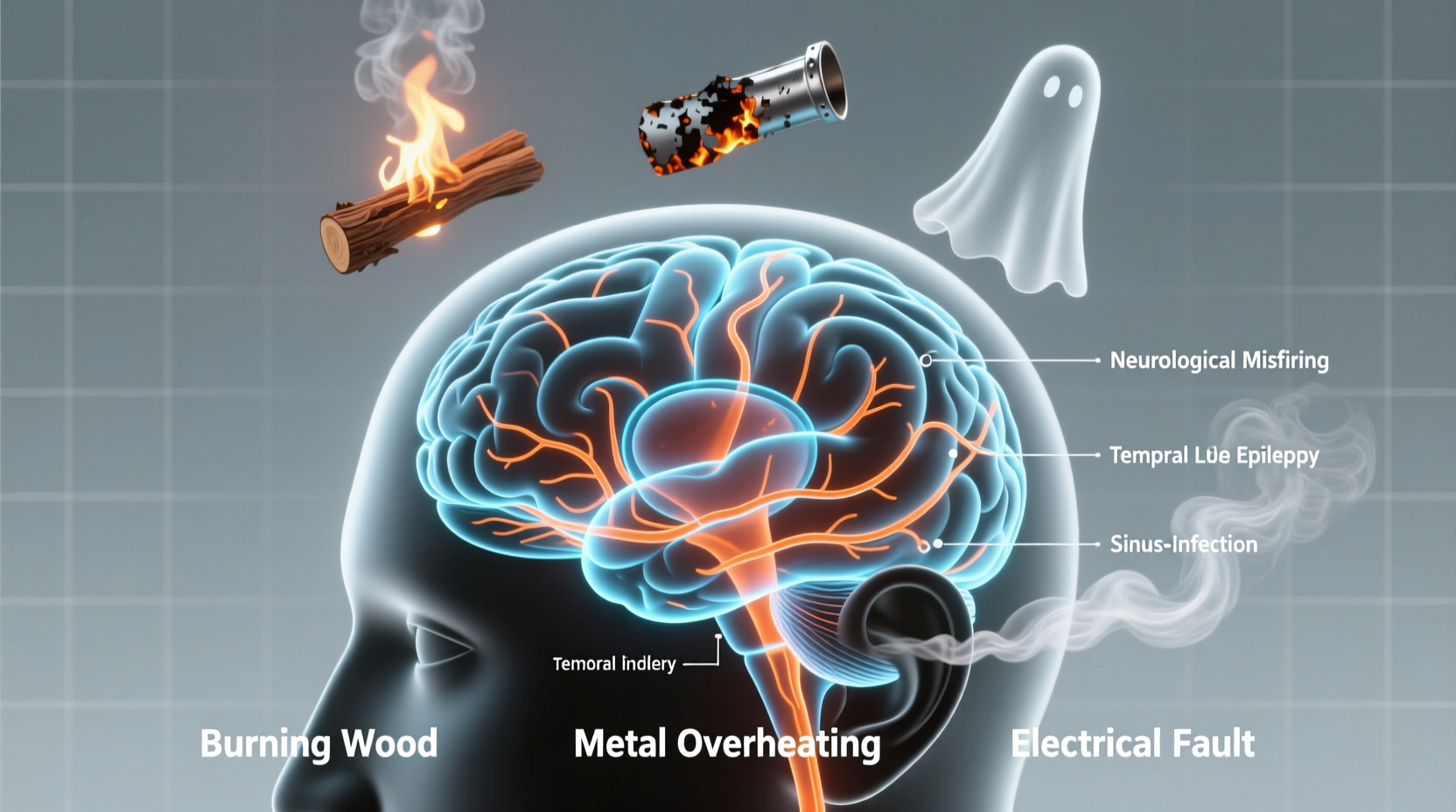
Common Causes of Burning Smells That Aren’t Real
The nose and brain work together to interpret odors, so disruptions at any point in this system can lead to false signals. Here are the most frequent explanations for smelling burning when there’s no fire:
Nasal and Sinus Conditions
Infections, chronic sinusitis, or nasal polyps can irritate the olfactory nerves, leading to abnormal smell signals. Post-nasal drip, allergies, or exposure to strong irritants (like cleaning products) may also trigger temporary phantosmia.
Neurological Disorders
Because smell is processed in the brain, neurological issues are a major contributor. Conditions such as:
- Epilepsy (especially temporal lobe seizures)
- Parkinson’s disease
- Migraines
- Alzheimer’s disease
“Olfactory hallucinations can be the only noticeable symptom of a seizure disorder, especially if it originates in the temporal lobe.” — Dr. Lena Patel, Neurologist, Johns Hopkins Medicine
Head Injuries
Trauma to the head can damage the olfactory bulb or nerve pathways responsible for smell. Even mild concussions may disrupt sensory processing, leading to phantom odors months after the initial injury.
Viral Infections (Including Post-COVID)
One of the most recognized triggers in recent years is viral infection, particularly SARS-CoV-2. Many people recovering from COVID-19 report lingering smell distortions, including phantom burning or chemical scents. This is believed to stem from inflammation or damage to olfactory support cells.
Medications and Toxins
Certain drugs—including antibiotics, antidepressants, antihypertensives, and chemotherapy agents—can alter smell perception. Long-term exposure to chemicals like pesticides or solvents may also contribute.
When to Be Concerned: Red Flags
While isolated episodes of phantom smells may resolve on their own, certain patterns warrant medical evaluation. Seek prompt care if you experience:
- Frequent or worsening phantom odors
- Loss of ability to smell real odors (anosmia)
- Headaches, dizziness, or vision changes
- Seizures or muscle twitching
- Memory problems or confusion
- Recent head trauma
| Symptom Pattern | Possible Cause | Action Recommended |
|---|---|---|
| Smell occurs before dizziness or confusion | Temporal lobe seizure | See neurologist; consider EEG |
| Follows cold or sinus infection | Sinus inflammation | ENT consultation; imaging if persistent |
| Began after head injury | Olfactory nerve damage | Neurological assessment |
| Accompanied by tremors or stiffness | Parkinson’s risk | Neurological screening |
| Started post-COVID recovery | Viral-induced parosmia | Smell training; monitor progression |
Diagnosis and Medical Evaluation
There is no single test for phantosmia, so diagnosis involves ruling out potential causes through a combination of assessments:
- Medical History Review: Doctors will ask about onset, frequency, associated symptoms, medications, infections, and head injuries.
- Nasal Endoscopy: An ENT specialist may examine your nasal passages for polyps, inflammation, or structural issues.
- Imaging: MRI or CT scans can detect brain abnormalities such as tumors, lesions, or signs of stroke.
- Neurological Testing: If a seizure disorder is suspected, an electroencephalogram (EEG) may be ordered.
- Smell Identification Tests: Standardized tests like the UPSIT (University of Pennsylvania Smell Identification Test) assess olfactory function.
Mini Case Study: Maria’s Persistent Burning Smell
Maria, a 52-year-old teacher, began noticing a sharp smell of burnt toast every morning, lasting about 30 seconds. No one else in her home smelled it, and she found no source. Initially dismissing it, she later noticed the episodes coincided with brief lapses in awareness—moments where she’d “zone out” during class. After consulting a neurologist and undergoing an EEG, she was diagnosed with complex partial seizures originating in the temporal lobe. With medication, both the seizures and phantom smells resolved within weeks.
Treatment and Management Strategies
Treatment depends entirely on the underlying cause. There is no universal cure for phantosmia, but several approaches can reduce or eliminate symptoms:
For Nasal Causes
Nasal saline rinses, corticosteroid sprays, or surgery (for polyps) may restore normal olfactory function. Treating chronic sinusitis often resolves phantom smells.
For Neurological Conditions
Antiseizure medications (e.g., carbamazepine, levetiracetam) are effective if phantosmia is seizure-related. Parkinson’s or Alzheimer’s management focuses on slowing disease progression, which may indirectly improve smell disturbances.
Post-Viral Recovery
Smell training—a daily exercise involving focused sniffing of strong, familiar scents (like lemon, rose, clove, and eucalyptus)—has shown promise in restoring normal olfactory function after viral damage. Studies suggest improvement in up to 30–60% of patients over several months.
Surgical Options
In rare, severe cases where phantosmia is debilitating and unresponsive to treatment, surgical intervention such as olfactory bulb ablation may be considered. However, this is reserved for extreme circumstances due to risks of permanent anosmia.
Checklist: What You Can Do Now
- ✅ Document when phantom smells occur and any patterns (time of day, triggers, duration).
- ✅ Note any related symptoms: headaches, memory lapses, nasal congestion, or dizziness.
- ✅ Review current medications with your doctor to identify possible side effects.
- ✅ Schedule an appointment with an ENT or neurologist if symptoms persist beyond two weeks.
- ✅ Start smell training if recovering from a viral infection.
- ✅ Avoid strong chemical irritants that could worsen nasal sensitivity.
Frequently Asked Questions
Can stress cause me to smell burning?
While stress doesn’t directly create phantom smells, it can heighten sensory awareness and lower seizure thresholds in susceptible individuals. Anxiety may amplify concern about the smell, making it seem more intense or frequent, but it’s rarely the primary cause.
Is smelling burning a sign of a brain tumor?
It’s uncommon, but possible. Brain tumors affecting the temporal lobe or olfactory regions can cause phantosmia. However, tumors usually present with additional symptoms like persistent headaches, vision changes, nausea, or cognitive decline. Isolated phantom smells are more likely due to less serious causes.
How long do phantom smells last?
Duration varies. Some resolve in days (e.g., after a cold), while others persist for months or longer—especially if linked to neurological conditions or post-viral complications. With proper treatment, many people see gradual improvement over time.
Conclusion: Take Action, Not Panic
Smelling burning when there’s no source is disconcerting, but it’s rarely an emergency. Most causes are treatable, and understanding the root issue brings clarity and control. Whether it’s a sinus infection, a neurological condition, or a post-viral effect, identifying the trigger is key to relief. Don’t ignore persistent symptoms, but avoid jumping to worst-case conclusions. Instead, take practical steps: document your experience, consult a specialist, and follow evidence-based interventions.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?