Suddenly catching a whiff of smoke—burning wood, cigarette fumes, or scorched plastic—when no fire is present can be unsettling. You check your stove, inspect electrical outlets, and scan the room, only to find nothing burning. If this has happened to you more than once, you may be experiencing phantosmia: the perception of an odor that isn’t actually there. Often described as “phantom smells,” these olfactory hallucinations can range from mildly annoying to deeply distressing, especially when they persist or interfere with daily life.
Phantosmia is more common than many realize, affecting people of all ages. While it’s usually not life-threatening, it can signal underlying health conditions ranging from nasal inflammation to neurological disorders. Understanding the root causes, recognizing warning signs, and knowing when to seek help are crucial steps in managing this condition effectively.
What Is Phantosmia?
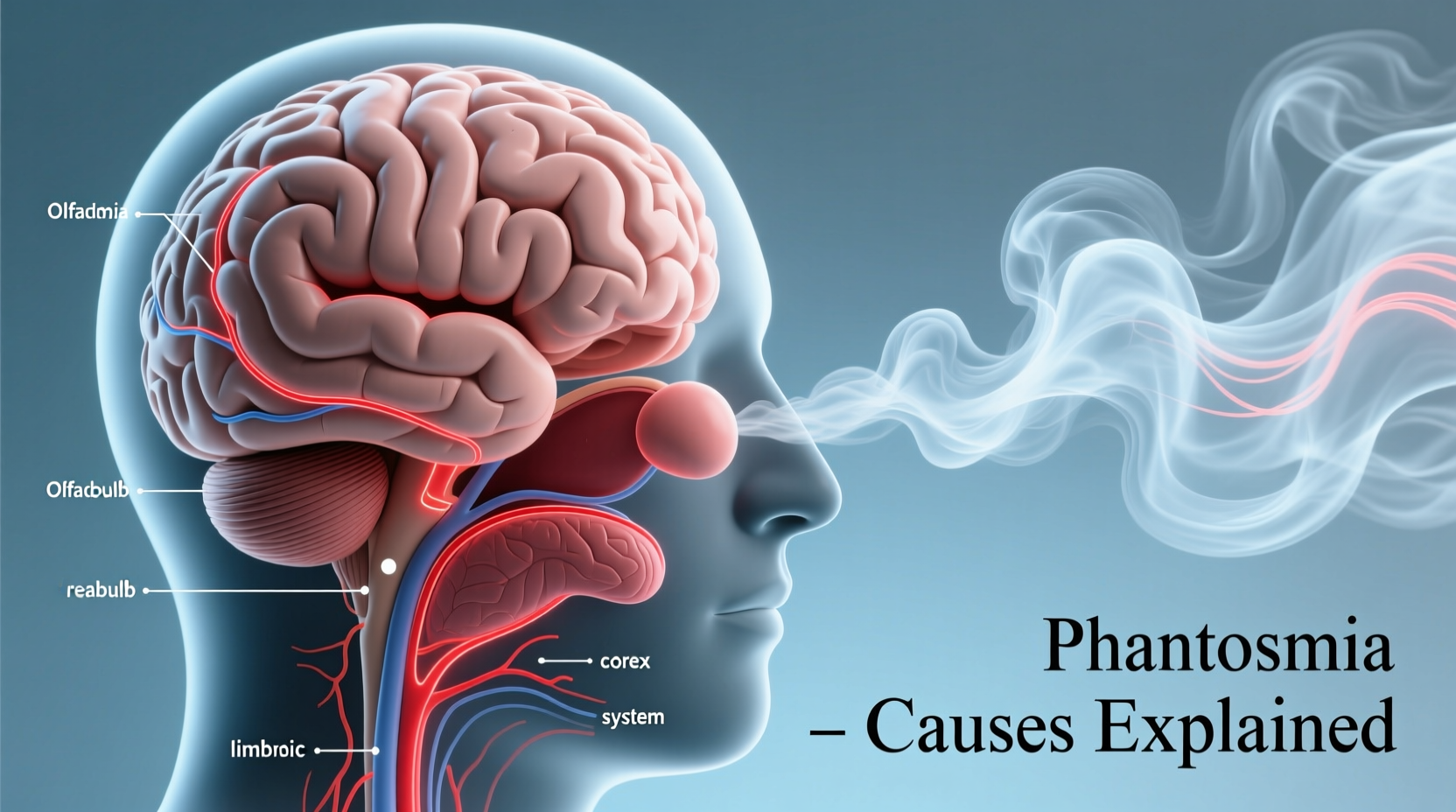
Phantosmia (from the Greek *phanto-* meaning “phantom” and *osme* meaning “smell”) is a form of olfactory hallucination. Individuals with phantosmia detect odors that have no external source. These phantom scents vary widely but often include unpleasant aromas such as:
- Burning or smoky odors
- Rotten eggs or sewage
- Chemicals or solvents
- Mold or mildew
- Fecal matter or decay
The phantom smell may affect one or both nostrils and can last seconds, minutes, or even hours. Some people experience it intermittently; others report persistent episodes that disrupt their sense of taste, appetite, and emotional well-being.
“Phantosmia is not just ‘in the nose’—it’s often a window into what’s happening in the brain or nervous system.” — Dr. Lena Torres, Neurologist & Smell Disorder Specialist, Johns Hopkins Medicine
Common Causes of Phantom Smoke Smells
The sensation of smelling smoke without a physical source can stem from several origins, broadly categorized into nasal, neurological, and systemic factors. Below are the most frequent causes supported by clinical research.
Nasal and Sinus Conditions
Issues within the nasal cavity are among the leading triggers of phantosmia. Inflammation or damage to the olfactory epithelium—the tissue responsible for detecting smells—can send false signals to the brain.
- Chronic sinusitis: Persistent inflammation of the sinuses alters mucus production and airflow, potentially distorting odor perception.
- Nasal polyps: Noncancerous growths in the nasal passages can obstruct airflow and irritate nerve endings.
- Upper respiratory infections: Viruses like the common cold or flu (including post-COVID conditions) can temporarily damage smell receptors.
- Nasal trauma: A blow to the head or surgical procedures involving the nose may disrupt olfactory nerves.
Neurological Disorders
Because smell signals travel directly to the brain via the olfactory bulb, neurological conditions often manifest through olfactory disturbances.
- Epilepsy: Temporal lobe seizures can trigger brief episodes of phantom smells as an aura before a seizure.
- Parkinson’s disease: Loss of smell (hyposmia) is an early symptom, but some patients report phantosmia before motor symptoms appear.
- Migraines: Olfactory hallucinations can precede or accompany migraine attacks in some individuals.
- Brain tumors: Rarely, tumors near the olfactory cortex or frontal lobe may cause persistent phantom odors.
Exposure to Toxins and Medications
Certain chemicals and pharmaceuticals are known to alter or damage the olfactory system.
- Chemical exposure: Prolonged contact with solvents, pesticides, or heavy metals (e.g., mercury, lead) may impair smell function.
- Medications: Antibiotics (like metronidazole), antidepressants, antihypertensives, and chemotherapy drugs list altered smell as a side effect.
Mental Health and Psychological Factors
While less common, psychiatric conditions such as depression, anxiety, and schizophrenia can involve olfactory hallucinations. In these cases, phantosmia is typically part of a broader symptom profile rather than an isolated issue.
It’s important to note that psychological causes don’t make the experience any less real to the individual. The brain processes the smell as genuinely as if it were external.
Post-Viral Smell Dysfunction (Including Long COVID)
Since the onset of the pandemic, a growing number of people have reported persistent smell distortions after recovering from SARS-CoV-2 infection. This includes:
- Parosmia (distorted smell, e.g., coffee smelling like sewage)
- Phantosmia (smelling things that aren’t there)
- Anosmia (complete loss of smell)
Studies suggest that viral damage to support cells in the olfactory epithelium leads to miswiring during recovery, resulting in phantom or distorted odors.
When to See a Doctor
Occasional, fleeting episodes of phantom smoke may not require immediate intervention. However, certain red flags warrant prompt medical evaluation:
| Symptom | Action Recommended |
|---|---|
| Smelling smoke daily for over two weeks | Consult ENT or neurologist |
| Phantom smells followed by confusion, twitching, or loss of awareness | Seek emergency evaluation for possible seizures |
| Accompanied by vision changes, headaches, or balance issues | Rule out brain abnormalities with imaging |
| Sudden smell distortion after head injury | Get assessed for cranial nerve damage |
| Loss of appetite or weight due to smell disturbance | Request referral to smell disorder clinic |
Diagnosis and Medical Evaluation
No single test confirms phantosmia, so diagnosis relies on a comprehensive assessment including:
- Medical history review: Onset, frequency, duration, and associated symptoms.
- Nasal endoscopy: Visual inspection of nasal passages for polyps, inflammation, or blockages.
- Smell identification tests: Standardized kits like the UPSIT (University of Pennsylvania Smell Identification Test).
- Imaging studies: MRI or CT scans to examine the brain and olfactory structures.
- Neurological exam: To assess cognitive function, reflexes, and seizure risk.
If no structural cause is found, doctors may explore medication side effects or refer to a psychiatrist or psychologist for further evaluation.
Treatment Options and Management Strategies
Treatment depends entirely on the underlying cause. There is no universal cure, but several approaches can reduce or eliminate phantom smells.
Medical and Surgical Interventions
- Nasal saline rinses: Help clear irritants and reduce inflammation.
- Topical steroids: Prescribed for chronic sinusitis or nasal polyps.
- Anticonvulsants: Used if phantosmia is linked to epilepsy.
- Surgery: Removal of polyps or correction of a deviated septum may restore normal smell function.
- Medication adjustment: Switching drugs that impair olfaction, under doctor supervision.
Olfactory Training (Smell Therapy)
A non-invasive, evidence-based method involves retraining the brain to interpret smells correctly. Patients sniff four strong essential oils (rose, lemon, clove, eucalyptus) twice daily for several months.
A 2020 study published in *The Laryngoscope* found that 30% of participants with post-viral phantosmia reported improvement after 12 weeks of smell training.
Lifestyle Adjustments
While healing takes time, these habits support recovery:
Real-Life Example: Sarah’s Journey with Post-COVID Phantosmia
Sarah, a 42-year-old teacher from Portland, began smelling cigarette smoke constantly—despite being a lifelong nonsmoker in a smoke-free home. It started three months after recovering from a moderate case of COVID-19.
Initially, she dismissed it as stress. But when the smell persisted and began affecting her ability to enjoy meals, she consulted an ENT specialist. After a nasal endoscopy and MRI (both normal), she was diagnosed with post-viral phantosmia.
Her doctor recommended saline rinses, nasal steroid spray, and olfactory training. Within five months, the phantom smoke faded significantly. “It wasn’t instant,” she says, “but having a plan made me feel in control again.”
Phantosmia Checklist: What You Can Do Now
If you’re experiencing unexplained smoke smells, use this actionable checklist:
- Track episodes: Note date, time, duration, and any triggers (e.g., after eating, during stress).
- Review medications: Check side effects of current prescriptions with your pharmacist.
- Perform nasal irrigation: Use a neti pot with distilled water daily.
- Schedule an ENT visit: Rule out sinus or nasal pathology.
- Start smell training: Use rose, lemon, clove, and eucalyptus oils twice daily.
- Monitor for neurological symptoms: Headaches, dizziness, memory lapses, or seizures need urgent attention.
- Reduce environmental irritants: Eliminate scented candles, air fresheners, and harsh cleaners.
Frequently Asked Questions
Can anxiety make me smell smoke when there’s none?
Yes. While anxiety doesn’t directly create phantom smells, it can heighten sensory awareness and lower the threshold for perceiving odors. In rare cases, severe anxiety or panic disorders may contribute to olfactory hallucinations, especially when combined with sleep deprivation or hyperventilation.
Is smelling smoke a sign of a brain tumor?
It’s extremely rare, but possible. Brain tumors affecting the temporal lobe or olfactory regions can cause phantosmia. However, this is almost always accompanied by other symptoms like persistent headaches, vision problems, seizures, or personality changes. If you have concerns, an MRI can rule out structural issues.
How long does phantosmia last?
Duration varies. Post-viral phantosmia often resolves within 6–18 months. Cases linked to sinusitis may improve within weeks of treatment. Chronic or neurological causes may require ongoing management. Patience and consistent care are key.
Conclusion: Take Control of Your Senses
Smelling smoke when there’s none can be confusing and alarming, but it’s rarely a sign of imminent danger. More often, it’s a signal from your body—pointing to inflammation, neurological activity, or recovery from illness. The first step toward relief is understanding the cause.
Don’t ignore persistent phantom smells, but also don’t jump to worst-case conclusions. Seek professional evaluation, document your symptoms, and engage in proven therapies like olfactory training. With the right approach, many people see significant improvement or complete resolution over time.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?