Vomiting after eating is more than just an unpleasant experience—it can signal underlying health issues that need attention. While occasional nausea may result from overeating or food intolerance, frequent post-meal vomiting warrants investigation. Understanding the root causes and knowing when to seek help can make a significant difference in your digestive health and overall well-being.
This article explores the most common reasons people vomit after eating, from benign triggers to serious medical conditions. It also provides actionable solutions, expert insights, and a clear path forward for those struggling with this distressing symptom.
Digestive Triggers and Dietary Factors
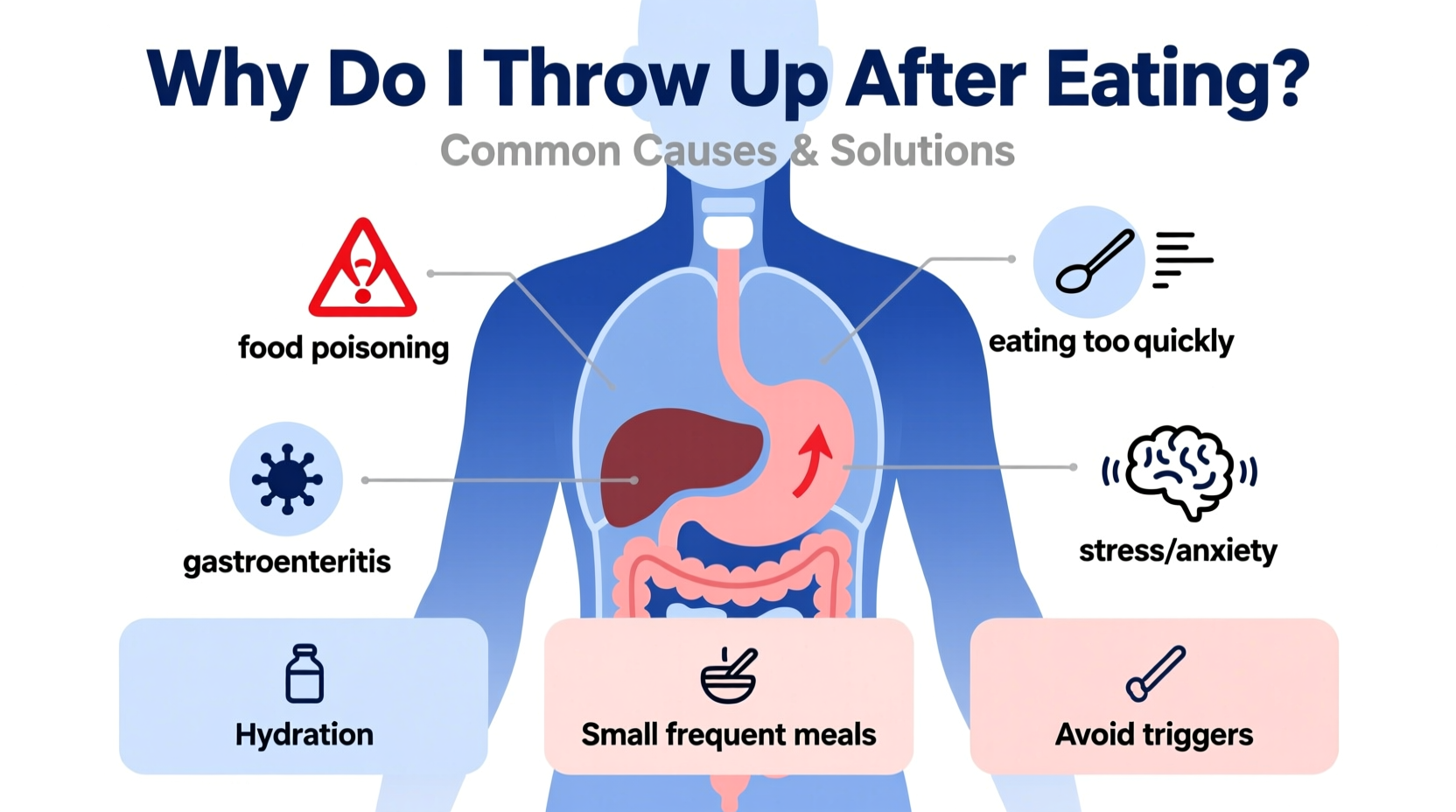
One of the most frequent reasons for vomiting after meals lies in what you eat and how you eat it. Certain foods, eating habits, and sensitivities can overwhelm the digestive system, leading to nausea and vomiting.
- Overeating: Consuming large portions stretches the stomach, triggering pressure-sensitive nerves that can induce vomiting.
- Fatty or spicy foods: These delay gastric emptying and irritate the stomach lining, increasing the risk of nausea.
- Food intolerances: Lactose intolerance, gluten sensitivity (non-celiac), or reactions to food additives can cause gastrointestinal distress within minutes to hours after eating.
- Eating too quickly: Rapid consumption leads to poor chewing and excess air intake, contributing to bloating and reflux.
Medical Conditions That Cause Post-Meal Vomiting
Beyond dietary choices, several medical conditions are known to cause vomiting after eating. Recognizing these can prompt timely diagnosis and treatment.
Gastroparesis
A condition where the stomach empties too slowly due to nerve damage—often from diabetes or surgery. Symptoms include early satiety, bloating, nausea, and vomiting hours after eating.
Gastroesophageal Reflux Disease (GERD)
Chronic acid reflux can cause stomach contents to back up into the esophagus, sometimes leading to regurgitation or vomiting, especially when lying down after meals.
Pyloric Stenosis
More common in infants but possible in adults due to scarring or tumors, this narrowing of the stomach’s exit valve blocks food from moving into the small intestine.
Peptic Ulcers and Gastritis
Inflammation or sores in the stomach lining can make digestion painful and trigger vomiting, particularly if the ulcer obstructs the digestive tract.
Pregnancy and Hormonal Changes
Morning sickness affects many pregnant individuals, often worsening after meals due to heightened sensitivity to smells and hormonal shifts.
“Persistent vomiting after eating should never be ignored. It can lead to dehydration, malnutrition, and may indicate a motility disorder like gastroparesis.” — Dr. Lena Patel, Gastroenterology Specialist
When Psychological Factors Play a Role
Mental health significantly influences digestive function. Conditions such as anxiety, bulimia nervosa, and rumination syndrome can manifest as vomiting after eating.
- Anxiety and stress: Activate the autonomic nervous system, disrupting normal digestion and causing nausea or vomiting.
- Bulimia nervosa: An eating disorder involving binge eating followed by self-induced vomiting. Requires psychological and medical intervention.
- Rumination syndrome: A rare condition where undigested food returns to the mouth without nausea or retching, often due to subconscious habit.
These conditions are not simply “in the head”—they have real physical consequences and require compassionate, multidisciplinary care.
Solutions and Management Strategies
Addressing vomiting after eating involves both immediate relief tactics and long-term lifestyle adjustments. The right approach depends on the underlying cause.
Step-by-Step Guide to Managing Symptoms
- Track your symptoms: Keep a food and symptom diary noting what you eat, when you vomit, and associated factors (stress, posture, timing).
- Modify portion sizes: Eat smaller, more frequent meals to reduce stomach distension.
- Avoid trigger foods: Eliminate greasy, spicy, or acidic foods temporarily to see if symptoms improve.
- Stay upright after eating: Wait at least 2–3 hours before lying down to prevent reflux.
- Hydrate wisely: Sip water between meals rather than during to avoid overfilling the stomach.
- Seek medical evaluation: If vomiting persists beyond a few days or is accompanied by weight loss, pain, or dehydration, consult a doctor.
| Cause | Key Signs | Solutions |
|---|---|---|
| Overeating | Fullness, bloating, immediate nausea | Smaller portions, mindful eating |
| Gastroparesis | Vomiting hours after eating, early satiety | Low-fat/low-fiber diet, medication, gastric stimulants |
| GERD | Heartburn, regurgitation, sour taste | Antacids, elevate head while sleeping, avoid late meals |
| Food Intolerance | Gas, diarrhea, delayed nausea | Elimination diet, enzyme supplements (e.g., lactase) |
| Bulimia Nervosa | Self-induced vomiting, secrecy around food | Therapy, nutritional counseling, medical monitoring |
Real-Life Example: Sarah’s Journey with Gastroparesis
Sarah, a 34-year-old teacher with type 1 diabetes, began experiencing nausea and vomiting 2–3 hours after every meal. She initially assumed it was food poisoning or stress. Over months, she lost 15 pounds unintentionally and felt constantly fatigued.
After visiting a gastroenterologist, she underwent a gastric emptying study, which confirmed gastroparesis. Her treatment plan included a low-residue diet, metoclopramide to stimulate stomach contractions, and strict blood sugar management. Within six weeks, her symptoms improved significantly.
Sarah’s case highlights the importance of not dismissing chronic vomiting as mere indigestion. Early diagnosis prevented further complications like malnutrition and bezoar formation.
Checklist: When to See a Doctor
- ✅ Vomiting occurs regularly after meals for more than a week
- ✅ You notice blood in vomit (red or coffee-ground appearance)
- ✅ Unintentional weight loss accompanies the vomiting
- ✅ Severe abdominal pain or chest pain is present
- ✅ Signs of dehydration: dark urine, dizziness, dry mouth
- ✅ History of diabetes, gastric surgery, or neurological conditions
Frequently Asked Questions
Is it normal to throw up after eating one bad meal?
Occasional vomiting after consuming spoiled food, alcohol, or an unusually rich meal can be normal. The body uses vomiting to expel harmful substances. However, if it happens frequently or without clear cause, it’s not normal and should be evaluated.
Can anxiety really make me vomit after eating?
Yes. Anxiety activates the gut-brain axis, altering digestive motility and increasing stomach sensitivity. Some people experience “nervous stomach” symptoms, including nausea and vomiting, especially in high-stress situations or after meals associated with anxiety.
What tests diagnose the cause of post-meal vomiting?
Common diagnostic tools include endoscopy, gastric emptying studies, upper GI series, blood tests (for infection, electrolytes, or diabetes), and abdominal ultrasound. Your doctor will choose based on suspected cause.
Take Control of Your Digestive Health
Vomiting after eating is not something you should learn to live with. Whether it stems from poor eating habits, a treatable condition like GERD, or a complex disorder like gastroparesis, effective solutions exist. Start by adjusting your diet and eating patterns, monitor your symptoms, and don’t hesitate to seek professional help when needed.
Your digestive system plays a vital role in your energy, mood, and overall health. Addressing vomiting after meals isn’t just about comfort—it’s about protecting your long-term well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?