Waking up at 3 a.m. with a racing mind or an inexplicable sense of alertness is more common than many realize. While the world outside remains dark and quiet, your internal clock may be signaling something deeper—whether it’s stress, hormonal shifts, or poor sleep habits. This pattern isn’t just inconvenient; it can erode your energy, focus, and emotional resilience over time. The good news? Most causes are manageable with targeted lifestyle adjustments and improved sleep hygiene. Understanding what triggers these middle-of-the-night awakenings is the first step toward restoring restful, uninterrupted sleep.
The Science Behind Waking at 3 a.m.
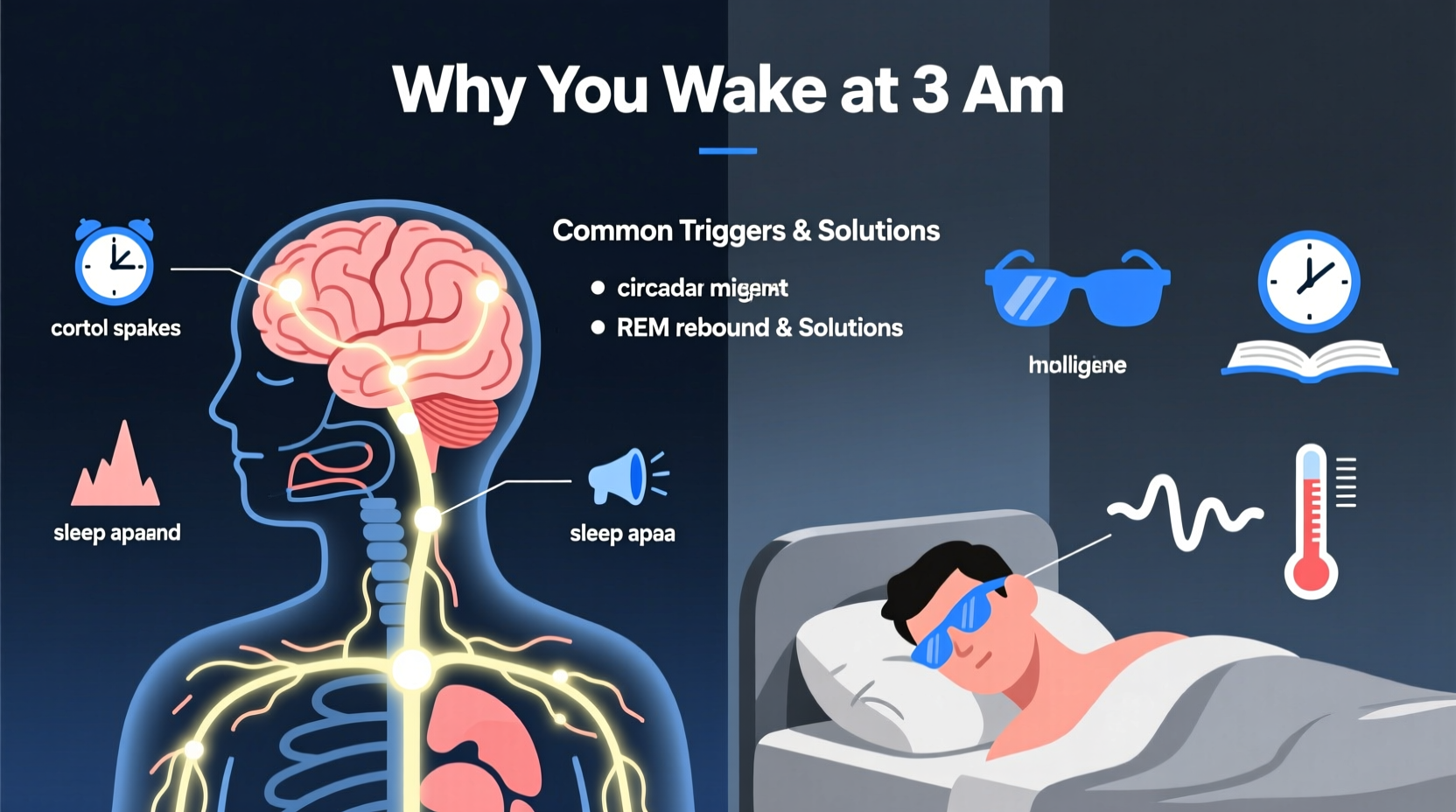
The human sleep cycle operates in roughly 90-minute phases, moving through light sleep, deep sleep, and REM (rapid eye movement) stages. Around 3 a.m., most people are in their final cycles, often entering a lighter phase of sleep that makes them more susceptible to waking. But while brief awakenings are normal, staying awake for extended periods indicates an underlying disruption.
This timing also coincides with natural dips and surges in key hormones. Cortisol, the body’s primary stress hormone, begins rising around 3–4 a.m. as part of the circadian rhythm preparing you for the day ahead. In individuals under chronic stress or with dysregulated cortisol levels, this rise can be premature or exaggerated, jolting them into full wakefulness. Meanwhile, melatonin—the hormone responsible for sleep onset—peaks earlier in the night and begins to decline by 3 a.m., reducing its sedative effect.
“The early morning awakening pattern is one of the hallmark signs of hyperarousal states, commonly seen in anxiety and depression.” — Dr. Rebecca Turner, Sleep Neurologist, Stanford Center for Sleep Sciences
Potential Causes of 3 a.m. Awakenings
Repeatedly waking at the same time each night is rarely random. It often reflects a consistent physiological or psychological trigger. Below are some of the most common contributors:
1. Stress and Anxiety
Mental load doesn’t shut off when you lie down. Unresolved worries, work pressure, or subconscious rumination can activate the sympathetic nervous system during vulnerable sleep phases. At 3 a.m., when external stimuli are minimal, the brain may shift focus inward, amplifying anxious thoughts.
2. Blood Sugar Imbalances
Going to bed on an empty stomach or consuming high-glycemic foods late at night can lead to nocturnal hypoglycemia (low blood sugar). When glucose drops, the body releases adrenaline and cortisol to compensate, triggering wakefulness. People with insulin resistance or prediabetes are especially prone.
3. Hormonal Shifts
In women, fluctuating estrogen and progesterone during perimenopause or menopause can destabilize sleep architecture. Night sweats and hot flashes often peak between 2–4 a.m., disrupting continuity. Similarly, thyroid imbalances—particularly hyperthyroidism—can increase metabolic rate and neural excitability at night.
4. Sleep Apnea and Breathing Disruptions
Obstructive sleep apnea (OSA) frequently causes micro-awakenings due to breathing interruptions. These events may not fully rouse consciousness but prevent sustained deep sleep. Over time, they condition the brain to expect interruption, making 3 a.m. awakenings habitual even when oxygen levels stabilize.
5. Circadian Rhythm Misalignment
Shift workers, frequent travelers, or those with irregular bedtimes may experience a phase-delayed or fragmented circadian rhythm. If your internal clock is out of sync with environmental cues like light and darkness, your body may interpret 3 a.m. as a natural transition point rather than a time to remain asleep.
6. Medications and Stimulants
Certain medications—including antidepressants, corticosteroids, and beta-blockers—can interfere with sleep maintenance. Likewise, caffeine consumed after noon or nicotine use can linger in the system, increasing arousal during late sleep cycles.
Sleep Hygiene Fixes That Work
Improving sleep quality isn’t about drastic changes—it’s about consistency and precision. Small, evidence-based adjustments can significantly reduce 3 a.m. awakenings over time.
Optimize Your Evening Routine
Your pre-sleep habits set the tone for the entire night. Begin winding down 60–90 minutes before bed with low-stimulation activities such as reading, gentle stretching, or listening to calming music. Avoid screens that emit blue light, which suppresses melatonin production.
Regulate Food and Drink Timing
Eat dinner at least 3 hours before bedtime. Include complex carbohydrates and protein to stabilize blood sugar overnight. A small snack rich in tryptophan—like a banana with almond butter or a handful of walnuts—can support serotonin and melatonin synthesis without causing digestive discomfort.
Create a Sleep-Conducive Environment
Your bedroom should be cool (60–67°F), dark, and quiet. Use blackout curtains, a white noise machine, or earplugs if needed. Consider removing clocks from view—knowing it’s 3:17 a.m. only intensifies frustration and anxiety about being awake.
Step-by-Step Guide to Breaking the 3 a.m. Wake-Up Cycle
Follow this 7-day reset plan to retrain your sleep patterns and reduce early awakenings:
- Day 1–2: Audit Your Habits – Track bedtime, wake time, food intake, screen use, and mood. Note when you wake and how long it takes to return to sleep.
- Day 3: Adjust Light Exposure – Spend at least 15–30 minutes outdoors in the morning sunlight. Dim indoor lights after 8 p.m. to support natural melatonin release.
- Day 4: Implement a Wind-Down Ritual – Choose a sequence of relaxing activities (e.g., tea, journaling, breathing exercises) and repeat them nightly.
- Day 5: Eliminate Late Stimulants – Cut off caffeine by 12 p.m. and avoid intense exercise within 3 hours of bedtime.
- Day 6: Optimize Bedroom Conditions – Lower room temperature, remove electronics, and invest in a comfortable mattress or pillow if needed.
- Day 7: Practice the 15-Minute Rule – If you can’t fall back asleep within 15 minutes, get out of bed. Sit in dim light and do something calming (e.g., read a book) until drowsy.
Repeat this protocol weekly until improvements stabilize. Consistency matters more than perfection.
Do’s and Don’ts of Managing 3 a.m. Wakefulness
| Do’s | Don’ts |
|---|---|
| Maintain a consistent sleep schedule—even on weekends | Check the time if you wake up |
| Practice slow breathing or mindfulness when awake at night | Use your phone or turn on bright lights |
| Keep a glass of water by the bed to prevent dehydration-related wakefulness | Force yourself to “try harder” to fall asleep |
| Expose yourself to natural daylight within 30 minutes of waking | Consume sugary snacks during nighttime awakenings |
| Seek professional help if insomnia persists beyond 4 weeks | Self-diagnose or rely on sleeping pills long-term |
Real-Life Example: Maria’s Journey Back to Rest
Maria, a 42-year-old marketing director, began waking at 3 a.m. three times a week after a major project deadline. Initially, she dismissed it as temporary stress. But after six weeks of worsening fatigue and irritability, she consulted a sleep coach. Her assessment revealed elevated evening cortisol, late dinners, and a habit of checking work emails in bed.
She implemented a strict digital curfew at 8 p.m., started daily walking in the morning sun, and replaced late-night scrolling with gratitude journaling. Within 10 days, her nighttime awakenings dropped to once a week. By week four, she was sleeping through the night consistently. “I didn’t realize how much my routine was sabotaging my rest,” she said. “Now I protect my wind-down time like it’s a meeting with my CEO.”
Frequently Asked Questions
Is waking up at 3 a.m. a sign of depression?
Early morning awakening—especially when accompanied by difficulty returning to sleep and low mood upon waking—is a recognized symptom of depression. However, isolated 3 a.m. awakenings without other depressive symptoms may stem from stress, lifestyle factors, or sleep disorders. Consult a healthcare provider for proper evaluation.
Can diet really affect my ability to stay asleep?
Absolutely. Blood sugar fluctuations, dehydration, and stimulant intake all impact sleep continuity. Eating balanced meals throughout the day and avoiding heavy, spicy, or sugary foods at night supports stable energy and reduces nocturnal disruptions.
Should I nap if I’m tired after a 3 a.m. wake-up?
Short naps (10–20 minutes) early in the afternoon can help recovery without interfering with nighttime sleep. However, long or late naps (after 3 p.m.) may reduce sleep pressure and worsen the cycle of early awakenings.
When to Seek Medical Help
Occasional 3 a.m. awakenings are normal. But if you experience any of the following, consider consulting a sleep specialist:
- Waking at the same time for more than three weeks
- Excessive daytime fatigue despite adequate time in bed
- Loud snoring, gasping, or choking at night (signs of sleep apnea)
- Persistent anxiety or intrusive thoughts keeping you awake
- Hormonal symptoms like night sweats or heart palpitations
A sleep study, blood tests (for thyroid, glucose, or hormone levels), or cognitive behavioral therapy for insomnia (CBT-I) may be recommended based on your profile.
Final Thoughts: Reclaim Your Night
Waking at 3 a.m. doesn’t have to become your new normal. The body is designed for consolidated, restorative sleep—and with intentional adjustments, you can reset your rhythm. Start with one change: perhaps eliminating screens after dinner, adjusting your wake-up time, or practicing breathwork when you’re unable to sleep. Small steps compound into lasting transformation.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?