Waking up with a parched mouth is more than just an annoyance—it can affect your morning energy, oral health, and overall sleep quality. If you frequently reach for water the moment you open your eyes, you're not alone. Millions experience nocturnal dry mouth, often without understanding its root cause. While occasional dryness may result from mild dehydration, persistent symptoms point to deeper lifestyle, medical, or environmental factors. Understanding why this happens—and how to address it—is essential for restorative sleep and long-term wellness.
Understanding Dry Mouth (Xerostomia)
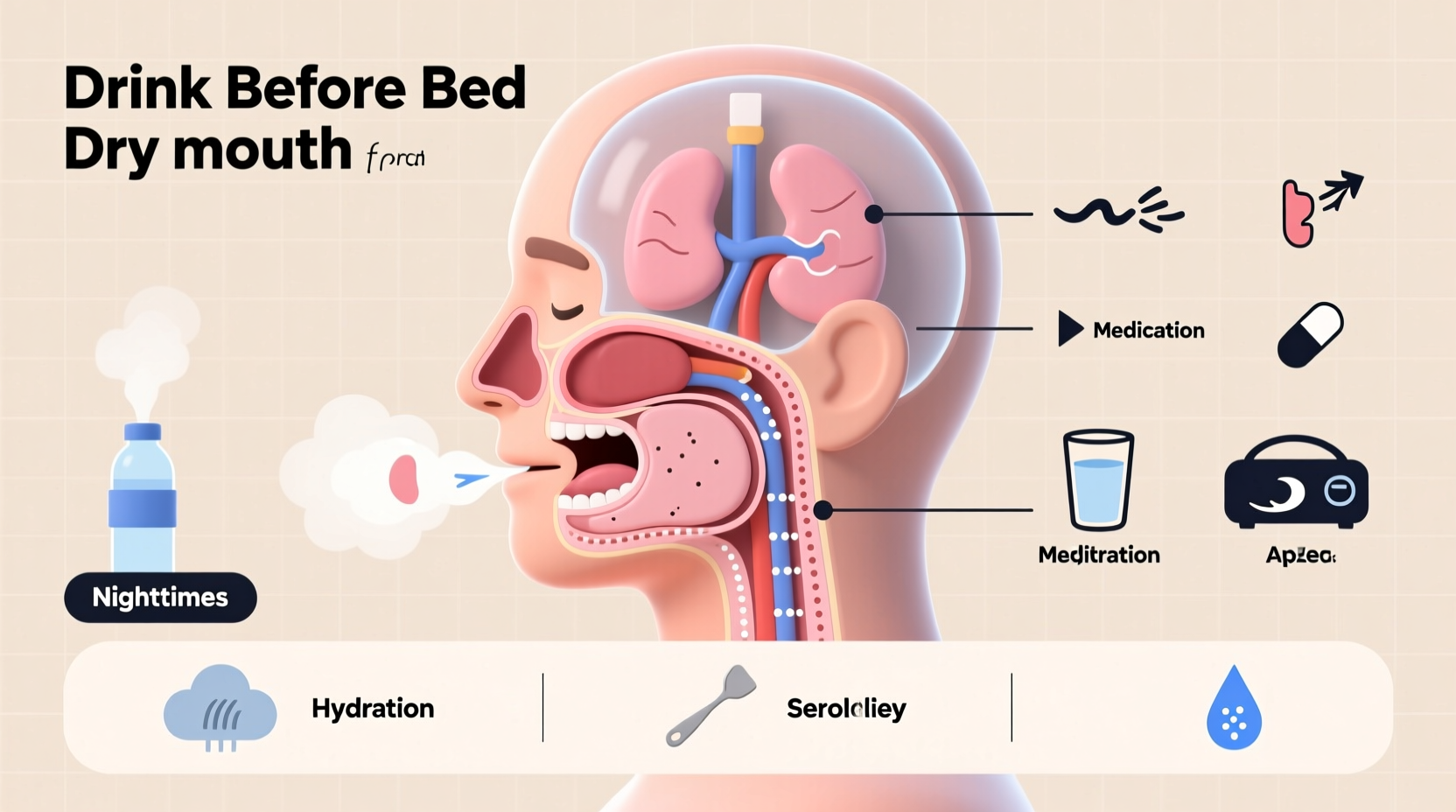
Dry mouth, medically known as xerostomia, occurs when salivary glands don’t produce enough saliva to keep the mouth moist. Saliva plays a critical role in digestion, oral hygiene, and tissue protection. It neutralizes acids, washes away food particles, and helps prevent tooth decay and infections. During sleep, saliva production naturally decreases, but significant dryness upon waking suggests an imbalance that needs attention.
Chronic dry mouth isn’t something to ignore. Left unaddressed, it increases the risk of cavities, gum disease, bad breath, and even difficulty swallowing or speaking over time. Identifying the triggers behind your nighttime dryness is the first step toward lasting relief.
Common Causes of Nighttime Dry Mouth
Dry mouth at night stems from a variety of sources—some behavioral, others medical. Recognizing these causes allows for targeted solutions rather than temporary fixes.
1. Mouth Breathing During Sleep
One of the most frequent culprits is breathing through your mouth instead of your nose while asleep. This often results from nasal congestion due to allergies, sinus issues, or structural problems like a deviated septum. Mouth breathing bypasses the natural humidification process of the nasal passages, leading to rapid moisture loss in the oral cavity.
2. Dehydration
Not drinking enough fluids during the day reduces overall hydration levels, which becomes especially noticeable at night. Alcohol consumption, caffeine intake, and high-sodium diets can all contribute to fluid loss, worsening dry mouth symptoms.
3. Medications
Over 400 commonly prescribed medications list dry mouth as a side effect. These include:
- Antihistamines and decongestants
- Antidepressants
- Diuretics
- Blood pressure medications
- Pain relievers
If you're on any regular prescriptions, check the patient information leaflet or consult your doctor about potential impacts on saliva production.
4. Medical Conditions
Certain chronic illnesses directly affect salivary function. Notable examples include:
- Sjögren’s syndrome: An autoimmune disorder that attacks moisture-producing glands.
- Diabetes: High blood sugar levels can lead to increased urination and dehydration.
- Obstructive sleep apnea (OSA): Often involves mouth breathing and disrupted breathing patterns that dry out the mouth.
- Autoimmune diseases: Such as lupus or rheumatoid arthritis, which may impair gland function.
5. Environmental Factors
Your bedroom environment plays a surprisingly large role. Sleeping in a room with low humidity—especially in winter when indoor heating is used—can suck moisture from the air and your mouth. Air conditioning units and fans also contribute by circulating dry air throughout the night.
Effective Nightly Fixes to Prevent Dry Mouth
While some causes require medical intervention, many cases of nighttime dry mouth can be significantly improved—or even resolved—with simple lifestyle adjustments and environmental changes.
1. Optimize Your Sleep Environment
Controlling humidity is one of the most impactful steps you can take. Using a humidifier in your bedroom adds moisture back into the air, counteracting the drying effects of heating and cooling systems.
“Maintaining indoor humidity between 40% and 60% can dramatically reduce symptoms of dry mouth and nasal congestion,” says Dr. Lena Torres, a board-certified sleep specialist.
Place the humidifier near your bed, clean it regularly to prevent mold buildup, and use distilled water to minimize mineral dispersion.
2. Stay Hydrated Throughout the Day
Don’t wait until bedtime to drink water. Aim for consistent hydration starting in the morning. The general recommendation is about 2.7 liters (91 oz) for women and 3.7 liters (125 oz) for men daily, including fluids from food and beverages.
Avoid excessive alcohol and caffeine, particularly in the evening, as both are diuretics that promote fluid loss. Instead, opt for herbal teas or infused water to maintain hydration without disrupting sleep.
3. Address Nasal Congestion
If you’re a habitual mouth breather, improving nasal airflow is crucial. Try these strategies:
- Use saline nasal sprays before bed to clear passages.
- Apply nasal strips to gently widen nostrils during sleep.
- Treat allergies with antihistamines—but choose non-drying formulas if possible.
- Consider seeing an ENT specialist if structural issues like a deviated septum are suspected.
4. Practice Good Oral Hygiene
Even if dry mouth isn’t caused by poor dental care, maintaining oral health minimizes complications. Use fluoride toothpaste and alcohol-free mouthwash to avoid further drying. Brush twice daily and floss once to reduce bacterial growth that thrives in dry environments.
Some dentists recommend products specifically formulated for dry mouth, such as Biotène or ACT Restoring Mouthwash, which help lubricate tissues and support pH balance.
5. Adjust Medication Timing or Alternatives
If medication is contributing to dryness, speak with your healthcare provider. In some cases, switching to an alternative drug or adjusting the timing of doses (e.g., taking certain meds earlier in the day) can reduce nighttime symptoms.
“Never stop or change prescription medications without consulting your physician, but always report bothersome side effects—they may have safer options available,” advises Dr. Alan Reeves, internal medicine specialist.
Step-by-Step Guide to Eliminate Nighttime Dry Mouth
Follow this practical, seven-day plan to identify and correct the source of your dry mouth:
- Day 1–2: Track Symptoms and Habits
Keep a journal noting when dryness occurs, what you eat/drink, medications taken, and how you feel upon waking. Include details like snoring, nasal stuffiness, or throat soreness. - Day 3: Assess Bedroom Environment
Measure room humidity using a hygrometer. If below 40%, introduce a cool-mist humidifier. Remove fans or AC units directed at your face. - Day 4: Improve Daytime Hydration
Increase water intake gradually. Replace one caffeinated beverage with herbal tea or fruit-infused water. Avoid salty snacks. - Day 5: Clear Nasal Passages
Use a saline rinse or spray before bed. Elevate your head slightly with an extra pillow to encourage nasal breathing. - Day 6: Review Medications
List all current prescriptions and supplements. Schedule a consultation with your doctor to discuss dry mouth side effects. - Day 7: Implement Oral Care Routine
Switch to a dry-mouth-friendly toothpaste and mouthwash. Avoid alcohol-based products that exacerbate dryness. - Ongoing: Monitor Progress
After one week, reassess symptom frequency. If no improvement, consider a sleep study or referral to a dentist or ENT specialist.
Do’s and Don’ts: Quick Reference Table
| Do’s | Don’ts |
|---|---|
| Drink water consistently throughout the day | Wait until you're thirsty to drink—thirst is a late sign of dehydration |
| Use a humidifier in your bedroom | Sleep with a fan blowing directly on your face |
| Treat allergies and nasal congestion proactively | Ignore chronic snoring or gasping during sleep |
| Choose alcohol-free oral care products | Use mouthwashes containing alcohol |
| See a doctor if symptoms persist beyond two weeks | Assume dry mouth is normal and unavoidable |
Mini Case Study: Resolving Chronic Dry Mouth Through Lifestyle Changes
Sarah, a 42-year-old teacher, had been waking up with severe dry mouth for over six months. She attributed it to her busy schedule and coffee habit but noticed increasing tooth sensitivity and bad breath despite good brushing habits. After reading about the link between mouth breathing and dryness, she decided to investigate.
She started tracking her symptoms and realized she often woke with a sore throat and stuffy nose. A visit to an ear, nose, and throat specialist revealed mild allergic rhinitis and a slightly deviated septum. With a combination of nightly saline rinses, an anti-allergy regimen, and a bedside humidifier, Sarah saw dramatic improvement within three weeks. Her morning dryness decreased significantly, and her dentist noted fewer signs of enamel erosion at her next checkup.
This case illustrates how seemingly minor issues—like untreated allergies—can compound into persistent discomfort. Targeted interventions made a meaningful difference without requiring medication changes or invasive procedures.
When to See a Doctor
Occasional dry mouth is common, but persistent symptoms warrant professional evaluation. Seek medical advice if you experience:
- Dryness every morning for more than two weeks
- Frequent thirst, even during the day
- Difficulty speaking, chewing, or swallowing
- Cracked lips, mouth sores, or persistent bad breath
- Known risk factors like diabetes or autoimmune disorders
A healthcare provider may perform blood tests, assess salivary flow, or recommend a sleep study if sleep apnea is suspected. Early diagnosis prevents complications and guides appropriate treatment.
FAQ
Can sleeping with your mouth open cause long-term damage?
Yes. Chronic mouth breathing dries oral tissues, increases plaque buildup, and raises the risk of gum disease and tooth decay. It can also alter facial development in children and contribute to sleep-disordered breathing in adults.
Is dry mouth a sign of sleep apnea?
It can be. Many people with obstructive sleep apnea breathe through their mouths due to blocked airways. Other warning signs include loud snoring, daytime fatigue, and witnessed breathing pauses during sleep. A sleep study can confirm the diagnosis.
Are there natural remedies for dry mouth at night?
Yes. Staying hydrated, using a humidifier, chewing sugar-free gum during the day to stimulate saliva, and practicing nasal breathing techniques can all help. Some find relief with aloe vera juice or coconut oil swishing (oil pulling), though scientific evidence is limited.
Conclusion: Take Control of Your Morning Comfort
Waking up with a dry mouth doesn’t have to be your new normal. By identifying the root cause—whether it’s dehydration, medication side effects, or undiagnosed sleep issues—you can implement targeted, sustainable solutions. Small changes like adding a humidifier, adjusting your fluid intake, or treating nasal congestion can yield significant improvements in sleep quality and oral health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?