Waking up with a headache is more than just an unpleasant way to start the day—it’s often a signal that something in your nighttime routine, sleep environment, or health needs attention. While dehydration is a well-known culprit, many people continue to experience morning headaches despite drinking enough water. The truth is, numerous underlying factors can contribute to this issue, ranging from sleep disorders and posture problems to neurological conditions and environmental triggers.
Understanding these less obvious causes is essential for finding long-term relief. Unlike headaches that arise during the day due to stress or screen fatigue, morning headaches are closely tied to what happens while you’re asleep—when your body should be recovering, not struggling. Addressing them requires looking beyond hydration and examining your sleep quality, breathing patterns, jaw alignment, and even mental health.
Sleep Apnea and Breathing Disruptions
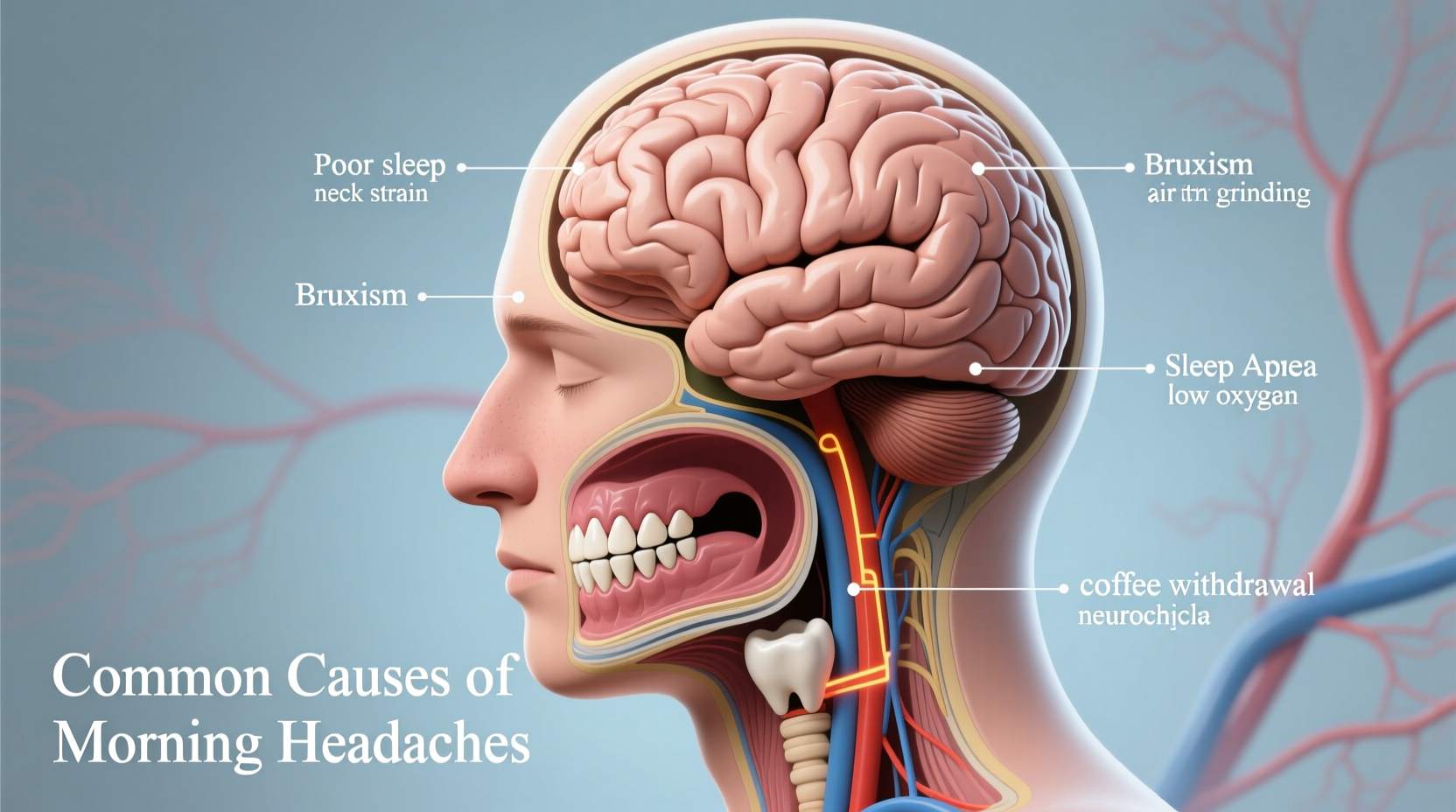
One of the most significant yet underdiagnosed causes of morning headaches is obstructive sleep apnea (OSA). This condition occurs when the airway becomes partially or completely blocked during sleep, causing breathing to stop and start repeatedly. These interruptions reduce oxygen levels in the blood and increase carbon dioxide, leading to blood vessel dilation in the brain—a key trigger for headaches upon waking.
People with OSA often report headaches localized at the back of the head, described as dull and bilateral. These typically resolve within 30 to 90 minutes after getting out of bed. Other symptoms include loud snoring, gasping during sleep, excessive daytime fatigue, and difficulty concentrating.
“Morning headaches in patients with untreated sleep apnea are a red flag. They’re not just inconvenient—they indicate poor oxygenation and disrupted sleep architecture.” — Dr. Lena Patel, Sleep Medicine Specialist
Diagnosis usually involves a sleep study, either at home or in a lab, which monitors breathing, heart rate, and oxygen levels. Treatment options like CPAP (continuous positive airway pressure) therapy can dramatically reduce or eliminate both apnea episodes and associated headaches.
Poor Sleep Posture and Neck Strain
Your sleeping position and pillow choice play a crucial role in spinal alignment. When your neck is bent awkwardly for several hours, muscles and nerves become strained, potentially triggering tension-type headaches by morning. This is especially common among stomach sleepers, whose necks are often twisted to one side throughout the night.
A pillow that’s too high, too flat, or made from unsupportive material can misalign the cervical spine, putting pressure on nerves and restricting blood flow. Over time, this leads to chronic stiffness and recurring headaches.
Optimal support varies by sleeping position:
- Back sleepers: Use a medium-height pillow that supports the natural curve of the neck.
- Side sleepers: Choose a firmer, thicker pillow to keep the head aligned with the spine.
- Stomach sleepers: Consider switching positions; if not possible, use an ultra-thin pillow or none at all.
Checklist: Evaluate Your Sleep Setup
- Is your pillow supporting your neck, not just your head?
- Does your mattress provide adequate support without sagging?
- Do you wake up with neck or shoulder tightness?
- Have you changed your pillow in the last 18–24 months?
- Are you sleeping in the same position every night?
Bruxism: The Hidden Impact of Teeth Grinding
Nocturnal bruxism—the involuntary clenching or grinding of teeth during sleep—is another frequent but overlooked cause of morning headaches. This habit places immense strain on the temporomandibular joint (TMJ) and the muscles involved in chewing, particularly the masseter and temporalis muscles. Pain often radiates from the jaw up into the temples, creating a band-like sensation across the forehead.
Bruxism is commonly linked to stress, anxiety, caffeine consumption, and certain medications. It may also occur alongside sleep apnea, as the body attempts to reopen the airway through jaw movements. Many people aren’t aware they grind their teeth until a dentist notices excessive tooth wear or a partner hears the noise at night.
Treatment includes wearing a custom-fitted night guard, managing stress through mindfulness or therapy, and reducing stimulants before bedtime. In some cases, Botox injections into the jaw muscles can help relax them and reduce grinding intensity.
| Symptom | Associated Condition | What to Do |
|---|---|---|
| Dull ache around temples | Bruxism | See a dentist for a night guard |
| Sharp pain at base of skull | Cervicogenic headache | Assess pillow height and posture |
| Headache improves after 1 hour | Sleep apnea | Consider a sleep study |
| Pulsating pain behind one eye | Hypnic or cluster headache | Consult neurologist |
| Nasal congestion with facial pressure | Sinus issues | Evaluate allergies or infections |
Medication Overuse and Rebound Headaches
Paradoxically, the very medications used to relieve headaches can become a cause of chronic morning pain. Known as medication overuse headaches (MOH), this condition develops when painkillers—especially those containing caffeine, codeine, or combination formulas—are taken more than two or three days per week over several months.
The brain adapts to frequent drug exposure, altering pain pathways and lowering the threshold for headache onset. As medication wears off overnight, withdrawal-like symptoms emerge, manifesting as a headache upon waking. Common culprits include:
- Excedrin (contains acetaminophen, aspirin, and caffeine)
- Ergotamines
- Triptans (used for migraines)
- Opioid-containing analgesics
Breaking the cycle requires discontinuing the overused medication under medical supervision. Withdrawal can initially worsen headaches for several days or weeks, but long-term outcomes are favorable with proper management and preventive therapies.
Step-by-Step Guide to Breaking the MOH Cycle
- Track your medication use: Record every dose of headache medication for at least two weeks.
- Consult a neurologist or primary care provider: Share your log and discuss a tapering plan.
- Stop overused drugs gradually: Sudden cessation can lead to severe rebound headaches.
- Start preventive treatment: Options include beta-blockers, anticonvulsants, or CGRP inhibitors for migraine sufferers.
- Adopt non-pharmacological strategies: Cognitive behavioral therapy, biofeedback, and regular exercise can reduce reliance on medication.
Other Potential Causes: Rare but Important
While most morning headaches stem from benign, treatable conditions, some may point to more serious underlying issues. Though uncommon, these require prompt evaluation:
- Hypnic headaches: Also known as “alarm clock” headaches, these occur exclusively during sleep, typically after age 50, and last 15 minutes to 4 hours. They happen at the same time each night and respond well to caffeine or lithium carbonate.
- Intracranial pressure disorders: Both high (idiopathic intracranial hypertension) and low (CSF leak) pressure can cause positional headaches worse in the morning. Accompanying symptoms may include vision changes, tinnitus, or neck stiffness.
- Nocturnal migraines: Some individuals experience migraine attacks exclusively during sleep. These are often accompanied by light/sound sensitivity, nausea, and aura upon waking.
- Environmental factors: Poor bedroom ventilation, high altitude, carbon monoxide exposure, or allergens like dust mites can contribute to morning head pain.
“Any new-onset headache after age 50, especially if daily and waking the patient, warrants imaging to rule out structural causes.” — Dr. Alan Zhou, Neurologist
Mini Case Study: Sarah’s Persistent Morning Pain
Sarah, a 38-year-old teacher, had been waking up with a dull headache for nearly six months. She drank plenty of water, avoided alcohol, and maintained a consistent sleep schedule, yet the pain persisted. Her primary care physician initially suspected tension headaches and recommended relaxation techniques.
When symptoms didn’t improve, she was referred to a sleep clinic. A home sleep test revealed moderate obstructive sleep apnea with 18 breathing interruptions per hour. After starting CPAP therapy, her headaches disappeared within three weeks. Follow-up assessments confirmed improved sleep quality and oxygen saturation.
Sarah’s case highlights how easily sleep-related causes can be missed without targeted questioning about snoring, daytime fatigue, and sleep quality. It also underscores the importance of interdisciplinary care—her dentist had previously suggested a night guard for jaw pain, but the root issue was respiratory, not dental.
Frequently Asked Questions
Can acid reflux cause morning headaches?
Yes, gastroesophageal reflux disease (GERD) can indirectly contribute. Lying flat allows stomach acid to rise, irritating the esophagus and stimulating vagus nerve pathways that influence headache centers in the brain. Elevating the head of the bed and avoiding late meals may help reduce both reflux and associated head pain.
Why do I get headaches only on weekends?
This pattern is often linked to “weekend migraines” or caffeine withdrawal. During the workweek, regular caffeine intake suppresses headaches, but reduced consumption on weekends triggers rebound effects. Alternatively, changes in sleep schedule—like sleeping in—can disrupt circadian rhythms and provoke headaches in susceptible individuals.
Should I be worried about a morning headache?
Occasional morning headaches are common and often manageable. However, seek medical advice if they are: daily or worsening, accompanied by neurological symptoms (vision loss, weakness, confusion), or occur after head trauma. New, persistent headaches after age 50 also require evaluation.
Conclusion: Take Control of Your Mornings
Waking up with a headache doesn’t have to be your normal. While dehydration is a valid concern, focusing solely on fluid intake may overlook deeper issues rooted in sleep quality, breathing, posture, or medication habits. By systematically evaluating your sleep environment, recognizing patterns, and seeking appropriate testing when needed, you can identify the real cause and take meaningful steps toward resolution.
Don’t dismiss morning head pain as inevitable. Whether it’s upgrading your pillow, treating undiagnosed sleep apnea, or reevaluating your painkiller use, small changes can lead to dramatic improvements in how you feel each morning. Your brain deserves rest—not pain—while you sleep.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?