Opening your eyes in the morning only to find a fresh, unexplained bruise on your arm, leg, or torso can be unsettling. You don’t recall bumping into anything. There’s no memory of injury. Yet, there it is—a purple or yellowish mark that wasn’t there the night before. While occasional bruising without clear cause may not always signal danger, frequent or unexplained bruises warrant attention. Understanding the underlying reasons—from harmless sleep behaviors to serious medical conditions—can help you determine whether it's time to consult a healthcare provider.
Common Causes of Unexplained Morning Bruises
Not every bruise comes from a dramatic fall or collision. Some develop silently during sleep due to subtle physical interactions or internal changes. Here are several everyday explanations for waking up with mystery bruises:
- Sleep-related movements: Tossing, turning, or even kicking in your sleep can cause minor impacts against bed frames, nightstands, or walls—especially if you're a restless sleeper.
- Medication side effects: Blood thinners (like warfarin or aspirin), certain antidepressants, and nonsteroidal anti-inflammatory drugs (NSAIDs) can increase bleeding under the skin, making bruising more likely—even from minimal pressure.
- Aging skin: As we age, our skin thins and loses protective fat layers, while blood vessels become more fragile. This makes older adults especially prone to easy bruising, sometimes referred to as “senile purpura.”
- Nutritional deficiencies: Low levels of vitamin C, vitamin K, or iron can impair blood vessel integrity and clotting function, increasing susceptibility to bruising.
- Hormonal fluctuations: Women may notice increased bruising around menstruation or during menopause due to shifts in estrogen, which affects capillary strength.
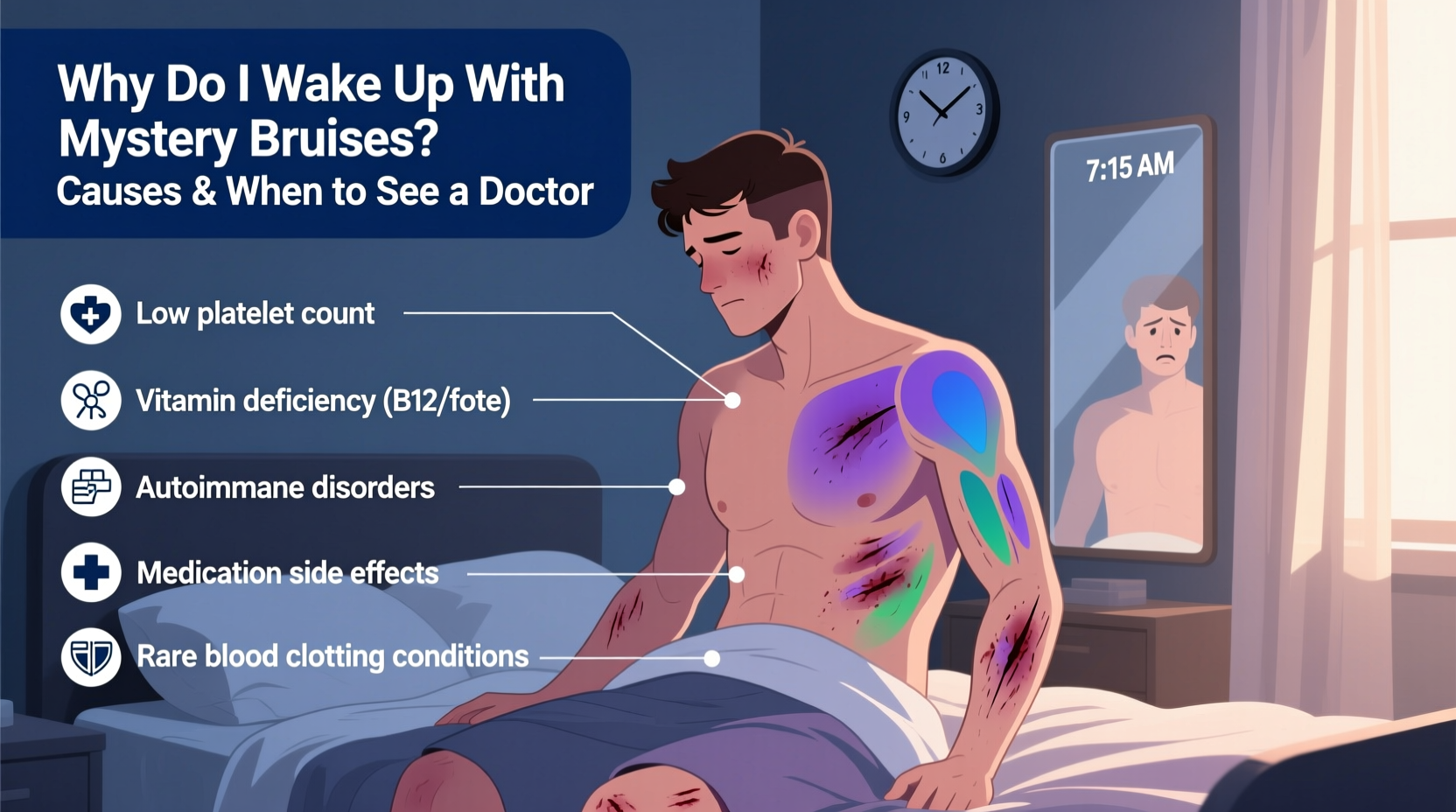
Medical Conditions Linked to Spontaneous Bruising
When bruising occurs frequently and without trauma, it may point to an underlying health issue. These conditions affect blood clotting, platelet function, or vascular integrity:
Blood Disorders
Conditions like thrombocytopenia (low platelet count), hemophilia, or von Willebrand disease interfere with the body’s ability to form clots. Even minor capillary damage can result in visible bruising.
Liver Disease
The liver produces many proteins essential for blood coagulation. Chronic liver conditions such as cirrhosis reduce this production, leading to easier bruising and prolonged bleeding.
Vasculitis and Connective Tissue Diseases
Inflammation of blood vessels (vasculitis) weakens vessel walls, causing leakage of blood into surrounding tissues. Autoimmune disorders like lupus or rheumatoid arthritis can also manifest through unexplained bruising.
Leukemia and Other Cancers
While rare, leukemia disrupts normal blood cell production, often resulting in low platelets and abnormal white blood cells. Early signs may include fatigue, frequent infections, nosebleeds, and spontaneous bruising—particularly on the legs or trunk.
“Unexplained bruising, especially when accompanied by other systemic symptoms like fatigue or weight loss, should prompt a timely evaluation.” — Dr. Lena Patel, Hematologist at Boston General Hospital
Risk Factors That Increase Likelihood of Mystery Bruising
Some people are naturally more predisposed to bruising than others. Recognizing personal risk factors helps assess whether your experience falls within a normal range or requires further investigation.
| Risk Factor | Description | What You Can Do |
|---|---|---|
| Genetics | Familial tendency toward fragile capillaries or clotting variations. | Monitor patterns and share family history with your doctor. |
| Female Sex | Women tend to have higher subcutaneous fat and thinner skin, increasing bruise visibility. | Focus on nutrition and gentle skin protection. |
| Long-term steroid use | Corticosteroids thin the skin and weaken blood vessels over time. | Discuss alternatives with your prescribing physician if possible. |
| Alcohol consumption | Heavy drinking impairs liver function and platelet activity. | Limit intake and consider liver health screening. |
| Strenuous exercise | Micro-tears in muscle fibers and increased circulation can lead to petechiae or small bruises. | Differentiate workout-related marks from random ones. |
When to See a Doctor: Red Flags to Watch For
Most isolated bruises aren't concerning. But certain warning signs suggest it’s time to schedule a medical appointment:
- Bruises appear frequently without known cause
- They occur in unusual locations (e.g., abdomen, back, face)
- You’re experiencing additional symptoms: excessive bleeding, fatigue, fever, joint pain
- Easy bleeding from gums or nose accompanies bruising
- Family history of bleeding disorders
- Recent start of new medication associated with bleeding risk
What Your Doctor Might Do
During an evaluation, your physician will likely:
- Review your full medical history, including medications and supplements.
- Perform a physical exam focusing on bruise pattern, distribution, and signs of systemic illness.
- Order lab tests such as a complete blood count (CBC), prothrombin time (PT/INR), partial thromboplastin time (aPTT), and liver function panel.
- Refer you to a hematologist if results indicate a clotting disorder or blood disease.
Mini Case Study: Sarah’s Mysterious Leg Bruises
Sarah, a 42-year-old teacher, began noticing large, painless bruises on her thighs every few weeks. She didn’t remember injuring herself and wasn’t taking any medications. Concerned, she visited her primary care provider. Initial CBC showed mild thrombocytopenia. Further testing revealed an autoimmune condition—immune thrombocytopenic purpura (ITP)—where her immune system was mistakenly destroying platelets. With early treatment involving corticosteroids and monitoring, Sarah managed her condition effectively. Her case highlights how seemingly benign bruising can be the first clue to a diagnosable, treatable disorder.
Step-by-Step Guide: How to Evaluate and Respond to Unexplained Bruising
If you're regularly finding bruises upon waking, follow this practical timeline to determine next steps:
- Week 1 – Document Everything: Note each bruise’s date, location, size, and whether you felt any impact during sleep. Use a ruler and camera for consistency.
- Week 2 – Assess Environment: Check your bedroom setup. Are sharp corners nearby? Is bedding tight enough to cause friction? Adjust layout if needed.
- Week 3 – Review Medications & Diet: List all prescriptions, OTC drugs, and supplements. Look up side effects. Evaluate dietary intake of vitamins C, K, and bioflavonoids.
- Week 4 – Consult Your Doctor: Bring your documentation. Request basic blood work if bruising persists or worsens.
- Ongoing – Monitor Changes: After initial assessment, continue tracking. Report sudden increases or new symptoms immediately.
Prevention and Skin Health Tips
While not all bruising can be prevented, strengthening your skin and circulatory system reduces vulnerability:
- Eat foods rich in vitamin C (citrus fruits, bell peppers, broccoli) to support collagen formation.
- Include vitamin K sources (leafy greens, fermented foods) to aid clotting.
- Stay hydrated—dry skin is more prone to damage.
- Use moisturizers with ingredients like shea butter or ceramides to improve skin resilience.
- Avoid excessive alcohol and smoking, both of which impair vascular health.
Frequently Asked Questions
Can stress cause bruising?
Stress itself doesn’t directly cause bruising, but chronic stress can elevate cortisol levels, which may thin the skin over time. Additionally, stress-related fatigue could make you less aware of minor bumps or injuries during the day—or more restless at night, increasing contact with hard surfaces while sleeping.
Why do bruises appear overnight when I didn’t get hurt?
Microtrauma during sleep—such as pressing your arm against a metal bed frame or rolling onto a corner of furniture—can rupture tiny blood vessels beneath the skin. Because these injuries happen unconsciously, you won’t recall them. Over hours, leaked blood accumulates, becoming visible only in the morning.
Are spider veins related to easy bruising?
Spider veins (small dilated blood vessels near the skin surface) and easy bruising can share underlying causes, such as weakened vessel walls or poor circulation. However, having spider veins doesn’t necessarily mean you’ll bruise more—but both may indicate a need for improved vascular health.
Action Checklist: Responding to Mystery Bruises
Use this concise checklist to stay proactive about unexplained bruising:
- ✅ Track new bruises weekly (location, size, color)
- ✅ Photograph each bruise for comparison over time
- ✅ Review current medications with a pharmacist or doctor
- ✅ Improve diet with vitamin-rich whole foods
- ✅ Modify bedroom environment to minimize sharp edges
- ✅ Schedule a doctor visit if bruises increase in frequency or size
- ✅ Request blood tests if red flags are present
Final Thoughts: Don’t Ignore the Signs
Waking up with a mystery bruise occasionally is usually nothing to fear. It might simply reflect a restless night or aging skin. But when bruising becomes routine, widespread, or appears alongside other symptoms, it deserves medical attention. The human body often communicates internal imbalances through subtle external cues—and unexplained bruising is one such signal. By paying attention, documenting changes, and seeking guidance when appropriate, you take control of your long-term health. Don’t dismiss recurring marks as mere quirks of aging or clumsy sleep habits. Sometimes, the answers lie beneath the surface—literally.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?