Rectal bleeding can be alarming, especially when it occurs without pain. One of the most common causes is internal hemorrhoids—swollen veins inside the lower rectum that may bleed during bowel movements. While often benign, persistent or heavy bleeding should never be ignored. Understanding why internal hemorrhoids bleed, what triggers it, and when to seek medical attention is essential for managing symptoms and ruling out more serious conditions.
What Are Internal Hemorrhoids?
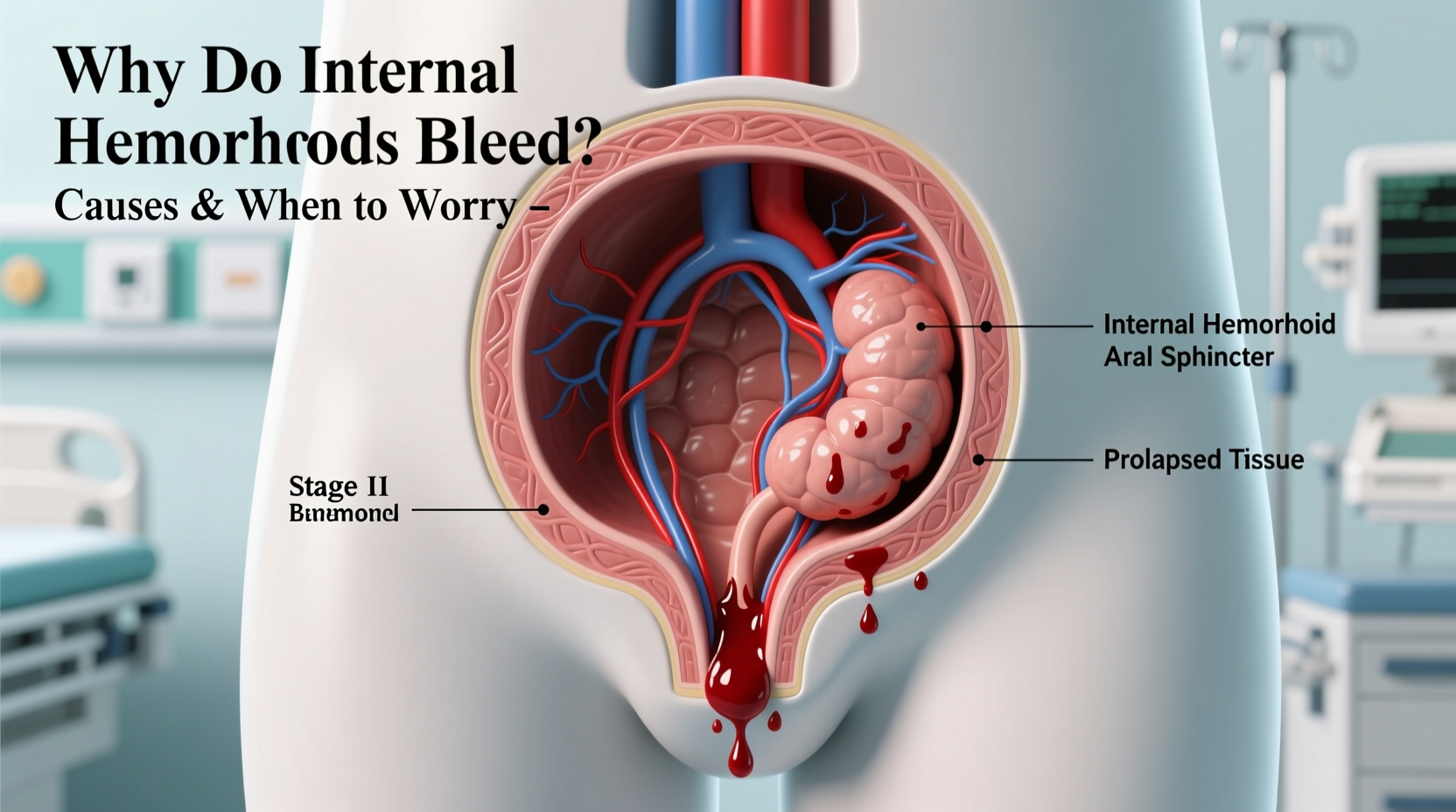
Internal hemorrhoids develop within the anal canal, above the dentate line—the anatomical boundary where nerve supply changes. Because this area lacks pain-sensitive nerves, internal hemorrhoids typically don’t cause discomfort unless they prolapse (protrude outside the anus) or become thrombosed. Instead, their most noticeable symptom is bright red blood on toilet paper, in the bowl, or coating the stool.
These vascular structures are part of normal anatomy but become problematic when increased pressure causes them to swell. This pressure commonly results from chronic constipation, straining during bowel movements, pregnancy, obesity, or prolonged sitting.
Why Do Internal Hemorrhoids Bleed?
Bleeding occurs when the delicate lining over an internal hemorrhoid is irritated or eroded, usually by hard stools passing through the rectum. The blood vessels in hemorrhoids are under pressure and close to the surface, making them prone to rupture even with minor trauma.
The typical presentation includes:
- Bright red blood—distinct from darker blood seen in upper gastrointestinal bleeding
- Intermittent bleeding, often linked to bowel movements
- No pain accompanying the bleeding (in early stages)
- Occasional mucus discharge
As internal hemorrhoids progress, they may prolapse. Initially, they might retract on their own; later, manual reduction may be needed. Prolapsed hemorrhoids are more likely to bleed due to exposure and friction.
Common Triggers of Bleeding
- Hard stools: Caused by low fiber intake or dehydration, leading to straining.
- Chronic diarrhea: Repeated irritation from frequent bowel movements.
- Pregnancy: Increased abdominal pressure and hormonal changes weaken vein walls.
- Lifting heavy objects: Creates sudden spikes in intra-abdominal pressure.
- Sedentary lifestyle: Prolonged sitting increases venous pressure in the pelvic region.
When to Worry: Red Flags That Require Medical Attention
While occasional light bleeding from internal hemorrhoids is common and often manageable at home, certain signs indicate a need for prompt evaluation. Rectal bleeding can mimic other serious conditions such as colorectal cancer, inflammatory bowel disease (IBD), or diverticulosis.
“Not all rectal bleeding is from hemorrhoids. In patients over 40, unexplained bleeding warrants colonoscopy to rule out malignancy.” — Dr. Alan Kim, Gastroenterologist
Warning Signs You Should Never Ignore
- Heavy or persistent bleeding: Soaking through toilet paper or requiring pads.
- Dark red or maroon blood: May suggest bleeding higher in the colon.
- Anemia symptoms: Fatigue, dizziness, pale skin, shortness of breath.
- Change in bowel habits: New-onset constipation, diarrhea, or narrow stools.
- Unintentional weight loss: A potential sign of underlying cancer.
- Family history of colorectal cancer: Increases risk and lowers threshold for investigation.
Patients over age 40 with new-onset rectal bleeding should undergo screening such as colonoscopy—even if hemorrhoids are visible—because two conditions can coexist.
Diagnosis and Treatment Options
A healthcare provider will typically begin with a digital rectal exam and may use an anoscope to visualize internal hemorrhoids. For those with risk factors or atypical symptoms, further testing like sigmoidoscopy or colonoscopy is recommended.
Non-Surgical Treatments
| Treatment | How It Works | Effectiveness |
|---|---|---|
| Rubber band ligation | Blocks blood flow to hemorrhoid; causes it to shrink and fall off | 70–80% success rate |
| Sclerotherapy | Injection of chemical to shrink tissue | Moderate effectiveness, less invasive |
| Infrared coagulation | Uses heat to seal vessels | Good for small hemorrhoids |
Lifestyle modifications remain foundational. Increasing dietary fiber, staying hydrated, and avoiding prolonged straining can prevent recurrence.
Surgical Options
For severe or recurrent cases, procedures like hemorrhoidectomy (surgical removal) or stapled hemorrhoidopexy may be necessary. These offer high cure rates but involve longer recovery times.
Real Example: Recognizing When Home Care Isn’t Enough
James, a 52-year-old office worker, noticed streaks of blood on his stool for several months. Assuming it was hemorrhoids—common since he often strained—he used over-the-counter creams and wipes. He improved temporarily but then began feeling unusually tired. After a routine blood test revealed iron-deficiency anemia, his doctor ordered a colonoscopy. To his surprise, he was diagnosed with early-stage colorectal cancer located near the rectum. The bleeding had been attributed to hemorrhoids, delaying diagnosis by nearly a year.
This case highlights a critical point: self-diagnosis of rectal bleeding can be dangerous. Even if hemorrhoids are present, they may not be the sole source of bleeding.
Prevention Checklist: Reduce Your Risk of Bleeding Hemorrhoids
Follow this actionable checklist to minimize strain and protect rectal health:
- ✅ Eat at least 25–30 grams of fiber daily (fruits, vegetables, whole grains, legumes)
- ✅ Drink 6–8 glasses of water per day
- ✅ Avoid delaying bowel movements when the urge arises
- ✅ Limit time spent on the toilet (no reading or phone use)
- ✅ Exercise regularly to support bowel motility
- ✅ Use a small footstool to elevate legs while sitting on the toilet (squatting position reduces strain)
- ✅ Avoid heavy lifting or use proper technique with core bracing
Frequently Asked Questions
Can internal hemorrhoids stop bleeding on their own?
Yes, mild bleeding often resolves with conservative care such as improved hydration, fiber intake, and avoiding straining. However, recurrence is common without long-term lifestyle changes.
Is it safe to use hemorrhoid suppositories long-term?
No. Overuse of topical treatments containing steroids or vasoconstrictors can damage sensitive rectal tissues. These should only be used short-term (usually no more than one week) unless directed by a physician.
Do internal hemorrhoids always require surgery?
No. Most cases respond well to non-surgical interventions like rubber band ligation or lifestyle adjustments. Surgery is reserved for large, prolapsing, or treatment-resistant hemorrhoids.
Conclusion: Take Control of Your Digestive Health
Bleeding from internal hemorrhoids is common but not something to dismiss lightly. While many cases stem from benign causes, ignoring persistent or worsening symptoms can have serious consequences. By understanding the triggers, recognizing warning signs, and seeking timely medical evaluation, you protect not only your comfort but your long-term health.
Don’t let embarrassment delay care. Speak openly with your doctor about any rectal bleeding, no matter how minor it seems. Early intervention leads to better outcomes, faster relief, and peace of mind.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?