Dry eyes are a common, often frustrating condition affecting millions worldwide. You might reach for lubricating eye drops expecting instant relief—only to find that the discomfort lingers or returns shortly after. This paradox leaves many wondering: if treatment is applied, why does the dryness persist? The answer isn't always simple. While artificial tears can help, they don’t address every underlying cause of dry eye symptoms. In fact, continued discomfort after drop use may point to misdiagnosis, improper product selection, environmental factors, or systemic health conditions that require more than surface-level treatment.
Understanding why your eyes remain dry despite using drops involves looking beyond temporary relief and examining the full picture of ocular health, tear composition, lifestyle habits, and medical history. This article breaks down the science behind persistent dry eye symptoms, identifies common pitfalls in self-treatment, and offers actionable strategies to achieve lasting comfort.
The Complexity of Tear Film and Dry Eye Disease
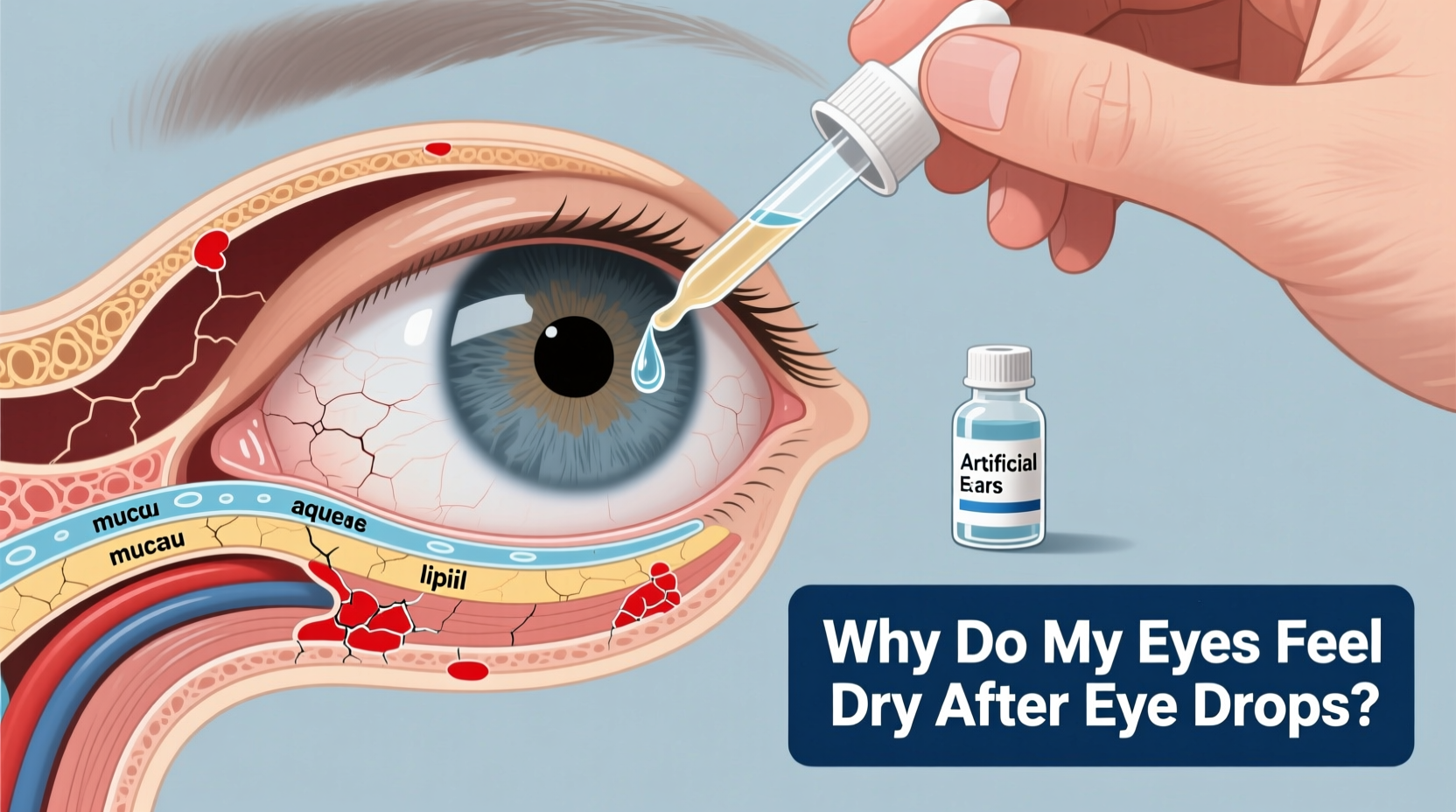
Your eyes rely on a delicate balance known as the tear film—a three-layered structure essential for moisture, clarity, and protection. These layers include:
- Lipid layer (outer): Prevents evaporation, produced by meibomian glands in the eyelids.
- Aqueous layer (middle): Provides hydration and nutrients, made by the lacrimal glands.
- Mucin layer (inner): Helps tears adhere to the eye surface, secreted by goblet cells.
Dry eye disease occurs when one or more of these layers is compromised. For example, evaporative dry eye—accounting for up to 86% of cases—is caused by meibomian gland dysfunction (MGD), where poor oil quality leads to rapid tear evaporation. In such cases, standard aqueous-based eye drops may offer only fleeting relief because they don’t replenish the lipid layer or treat gland blockage.
“Many patients come in using preserved artificial tears multiple times a day without realizing they’re worsening inflammation over time.” — Dr. Lena Patel, Cornea and External Disease Specialist
Common Reasons Eye Drops Don’t Provide Lasting Relief
1. Using the Wrong Type of Drop
Not all eye drops are created equal. Some contain vasoconstrictors that reduce redness but don’t improve hydration. Others have preservatives like benzalkonium chloride (BAK), which can damage the corneal surface with frequent use. Meanwhile, thick gels or ointments may blur vision and aren’t suitable for daytime use.
2. Underlying Meibomian Gland Dysfunction (MGD)
If your glands are clogged or underperforming, no amount of water-based drops will stop tears from evaporating too quickly. MGD often goes undiagnosed because symptoms mimic ordinary dryness, yet it requires warm compresses, lid hygiene, or in-office treatments like LipiFlow.
3. Environmental Triggers Persist
Dry air from heaters, air conditioning, fans, or prolonged screen use reduces blink rate and increases tear evaporation. Even with drops, exposure to these elements can undo any short-term benefit.
4. Systemic Health Conditions
Autoimmune diseases like Sjögren’s syndrome, rheumatoid arthritis, or lupus directly impair tear production. Medications including antihistamines, antidepressants, acne treatments, and blood pressure drugs also contribute to dry eye. Treating symptoms with drops won’t override these root causes.
5. Poor Application Technique
Many people blink immediately after applying drops, causing them to drain into the nasal cavity instead of spreading across the eye. Others touch the dropper tip to their eye or lashes, risking contamination and reducing shelf life.
Do’s and Don’ts When Managing Persistent Dry Eyes
| Do’s | Don’ts |
|---|---|
| Use preservative-free drops if applying more than 4x/day | Use redness-reducing drops long-term—they can worsen rebound redness |
| Apply warm compresses daily to support oil secretion | Rub your eyes aggressively—it damages delicate tissues |
| Blink fully and frequently during screen work | Sleep with ceiling fans blowing directly on your face |
| Stay hydrated and consume omega-3 fatty acids | Ignore worsening symptoms—seek evaluation before complications arise |
| Wear wraparound sunglasses outdoors to reduce wind exposure | Use expired or shared eye drops—risk of infection and reduced efficacy |
Step-by-Step Guide to Addressing Chronic Dry Eye Symptoms
If your eyes remain dry despite regular drop use, follow this structured approach to identify and resolve the issue:
- Pause and Assess Usage: Track how often you use drops, what type, and whether symptoms improve temporarily or not at all.
- Switch to Preservative-Free Drops: Replace preserved formulas with single-dose vials to eliminate chemical irritation.
- Implement Daily Lid Hygiene: Use a gentle cleanser or pre-moistened wipe to clean eyelid margins and remove debris.
- Apply Warm Compresses Twice Daily: Heat helps liquefy hardened oils in meibomian glands. Use a clean cloth soaked in warm water for 5–10 minutes.
- Optimize Your Environment: Add a humidifier, position computer screens below eye level, and take 20-second breaks every 20 minutes (20-20-20 rule).
- Evaluate Medications: Consult your doctor about alternatives to drugs known to cause dryness.
- Schedule a Comprehensive Eye Exam: An optometrist or ophthalmologist can perform tests like tear breakup time (TBUT), Schirmer test, or meibography to assess gland structure.
- Consider Advanced Treatments: Options include prescription drops (e.g., cyclosporine or lifitegrast), intense pulsed light therapy (IPL), or thermal pulsation devices.
Real-Life Example: Sarah’s Journey to Relief
Sarah, a 42-year-old graphic designer, used over-the-counter \"refreshing\" eye drops six times a day for months. Her eyes felt gritty and tired by mid-afternoon, especially after long design sessions. She assumed she just needed stronger drops. After visiting a cornea specialist, she learned she had moderate meibomian gland dropout visible on meibography. The drops she used contained BAK, which was irritating her already inflamed ocular surface.
Her treatment plan included switching to preservative-free artificial tears, daily warm compresses with lid massage, and twice-weekly use of an eyelid-cleaning foam. Within three weeks, her comfort improved significantly. By week six, she reduced drop usage to once daily and reported better focus and less fatigue. Sarah’s case highlights how symptom management without diagnosis can prolong suffering—and how targeted care brings real results.
When to See a Specialist
Occasional dryness is normal, especially in dry climates or during allergy season. However, persistent discomfort despite consistent drop use warrants professional evaluation. Red flags include:
- Pain or burning that interferes with daily tasks
- Blurred vision that clears with blinking
- Excessive tearing (a reflex response to dryness)
- Sensitivity to light or difficulty wearing contact lenses
- Visible redness or eyelid crusting
An eye care provider can differentiate between aqueous deficiency, evaporative dry eye, allergic conjunctivitis, or blepharitis—each requiring distinct management. Diagnostic tools now allow precise imaging of meibomian glands and measurement of tear osmolarity, enabling personalized treatment plans.
Frequently Asked Questions
Can using too many eye drops make dryness worse?
Yes. Preserved drops contain chemicals that can disrupt the ocular surface with frequent use. Overuse may trigger inflammation or desensitize natural tear production over time. Stick to preservative-free options for chronic use.
Why do my eyes water if they’re dry?
This is called reflex tearing. When the eye surface is irritated due to poor-quality tears, the brain signals the lacrimal gland to produce excess fluid. However, this reflex tear lacks proper composition and doesn’t lubricate effectively, leading to overflow and continued discomfort.
Are there natural ways to improve dry eyes?
Diet plays a key role. Omega-3 fatty acids found in flaxseed, chia seeds, walnuts, and fatty fish help reduce inflammation and improve meibum quality. Staying well-hydrated, avoiding smoke, and using indoor humidity levels above 40% also support ocular comfort.
Conclusion: Move Beyond Temporary Fixes
Dry eyes that persist after using drops are not a lost cause—they’re a signal that deeper investigation is needed. Artificial tears serve a purpose, but they’re only one piece of a larger puzzle. True relief comes from understanding the type of dry eye you have, addressing contributing lifestyle factors, and seeking expert guidance when necessary.
Don’t settle for temporary fixes that mask symptoms without healing the root issue. Take control of your eye health with informed choices, consistent self-care, and timely professional input. Your eyes deserve more than quick patches—they deserve sustainable comfort.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?