If you’re applying lip balm multiple times a day but still waking up to cracked, flaky, or painful lips, you’re not alone. Millions of people struggle with persistent chapping despite diligent use of balms and ointments. The issue often isn’t a lack of moisture—it’s what’s causing the moisture loss in the first place, or worse, what’s undermining your efforts to repair the damage.
Lips are uniquely vulnerable. Unlike the rest of your skin, they lack oil glands, hair follicles, and a thick protective barrier. This makes them prone to drying out quickly, especially when exposed to environmental stressors or internal imbalances. But when chapping becomes chronic—returning within hours of applying balm—something deeper is likely at play.
Understanding why standard lip care routines fail is the first step toward lasting relief. From ingredient sensitivities to underlying health conditions, this article explores the root causes of unrelenting lip dryness and provides actionable, dermatologist-backed strategies to restore soft, healthy lips for good.
The Hidden Reasons Lip Balm Isn’t Working
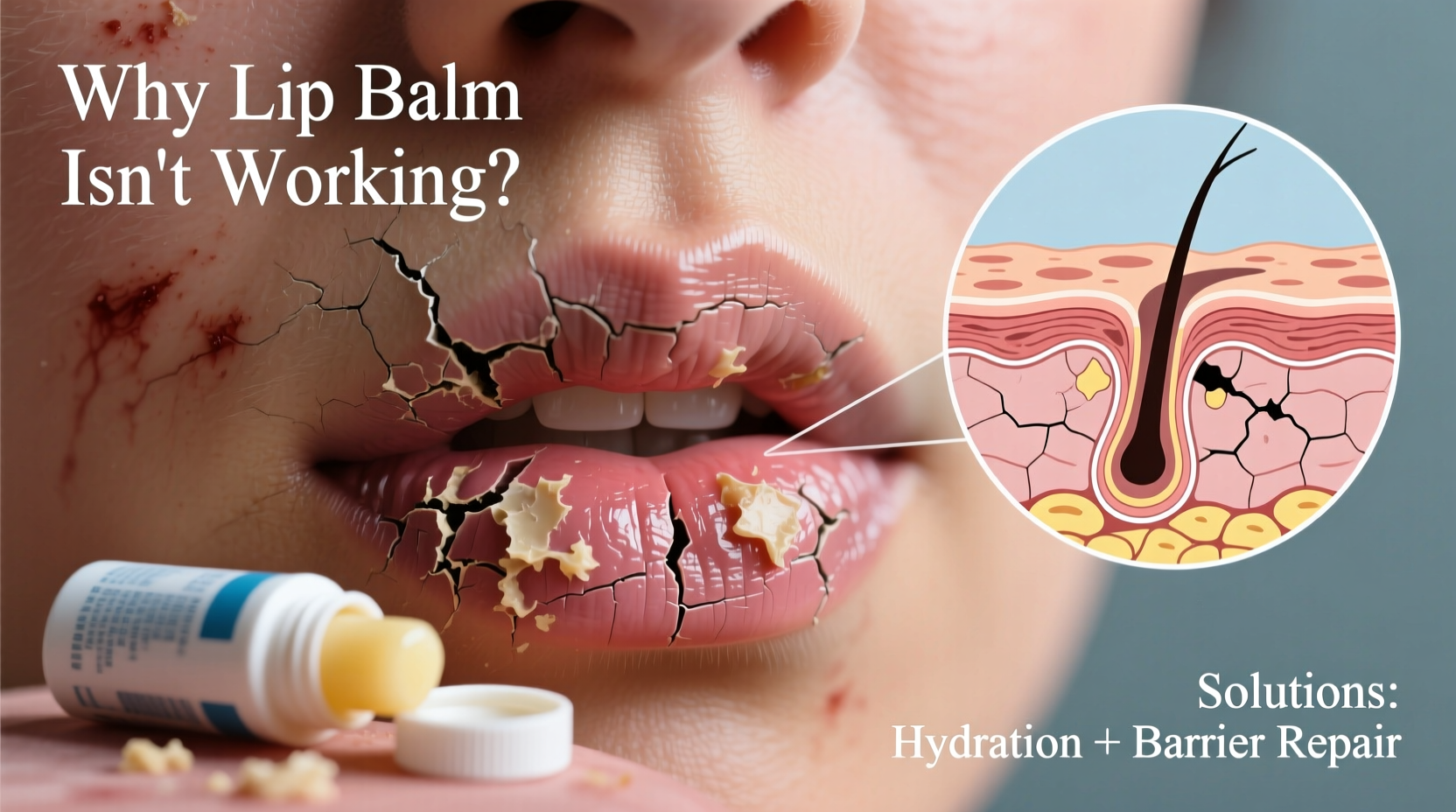
Most people assume that if their lips are dry, the solution is more moisture. So they reach for lip balm—sometimes dozens of times a day. But over-reliance on certain types of balms can actually make the problem worse.
Many popular lip products contain ingredients like menthol, camphor, phenol, or alcohol, which create a temporary cooling sensation but are highly irritating. These substances strip away natural oils and increase trans-epidermal water loss, leaving lips drier than before. Worse, they can trigger a cycle of dependency: the more you apply, the more irritated your lips become, prompting even more application.
Another common mistake is using flavored or scented balms. Artificial fragrances and flavorings (like vanilla, citrus, or cinnamon) are frequent allergens. Repeated exposure can lead to contact cheilitis—an inflammatory condition that mimics severe dryness but is actually an allergic reaction.
Underlying Medical and Environmental Triggers
Beyond product misuse, several systemic and environmental factors contribute to chronic lip chapping:
- Dehydration: Even mild dehydration reduces moisture available to the skin, including the lips. Many people don’t drink enough water, especially in dry climates or during heated indoor seasons.
- Allergies and Atopy: People with eczema, asthma, or seasonal allergies often have compromised skin barriers, making their lips more susceptible to irritation.
- Nasal Congestion: Breathing through the mouth due to allergies or sinus issues exposes lips to dry air, accelerating moisture loss.
- Vitamin Deficiencies: Low levels of B vitamins—especially B2 (riboflavin), B3 (niacin), and B12—can manifest as cracked lips, particularly at the corners (a condition called angular cheilitis).
- Fungal or Bacterial Infections: Moisture trapped in lip creases can foster yeast (Candida) or bacterial growth, leading to persistent inflammation that doesn’t respond to moisturizers.
“Chronic lip chapping is rarely just about dry weather. It’s often a sign of an irritant, allergen, or nutritional gap that needs addressing.” — Dr. Lena Patel, Board-Certified Dermatologist
Breaking the Cycle: A Step-by-Step Healing Plan
Fixing chronically chapped lips requires more than swapping balms. You need a strategic reset that removes irritants, repairs the skin barrier, and prevents recurrence.
Step 1: Stop Using Irritating Products
Immediately discontinue any lip balm with fragrances, flavors, or active cooling agents. This includes tinted balms, plumping glosses, and medicated formulas unless prescribed by a doctor.
Step 2: Cleanse Gently
Wash your lips once daily with lukewarm water and a fragrance-free facial cleanser. Avoid scrubbing or using exfoliants, which can worsen micro-tears.
Step 3: Apply a Barrier-Healing Ointment
Switch to a simple occlusive agent like pure petroleum jelly (Vaseline), white beeswax, or lanolin (if not allergic). These seal in moisture without adding irritants. Apply after every meal and before bed.
Step 4: Humidify Your Environment
Use a humidifier at night, especially in winter or dry climates. Keeping indoor humidity above 40% significantly reduces lip dryness.
Step 5: Protect from Sun and Wind
During the day, use a mineral-based lip balm with SPF 30 or higher. Zinc oxide or titanium dioxide provide physical protection without chemical irritants.
Step 6: Address Underlying Causes
If no improvement occurs within 10–14 days, consider medical evaluation. Blood tests can check for deficiencies in iron, zinc, or B vitamins. A patch test may reveal contact allergies.
Do’s and Don’ts: Lip Care Comparison Table
| Do | Don't |
|---|---|
| Use plain petroleum jelly or lanolin – creates a protective seal | Use flavored or scented balms – often contain allergens |
| Drink plenty of water – supports overall skin hydration | Lick your lips – saliva evaporates and contains enzymes that irritate |
| Apply SPF lip balm daily – prevents UV damage | Peel or bite off flakes – causes micro-injuries and bleeding |
| Take a B-complex supplement – if deficient, helps repair tissue | Over-apply lip balm – can clog pores and reduce natural repair |
Real-Life Case: Sarah’s Chronic Lip Struggle
Sarah, a 32-year-old teacher, used a popular mint-flavored lip balm religiously—up to 15 times a day. Despite this, her lips were constantly cracked, especially at the corners. She visited a dermatologist after developing a painful sore that wouldn’t heal.
Testing revealed she had both a sensitivity to menthol and a deficiency in vitamin B2 and iron. The cooling sensation she thought was “soothing” was actually irritating her skin, while her body lacked the nutrients needed to repair the damage.
Her treatment plan included switching to fragrance-free petroleum jelly, taking a B-complex and iron supplement, and using a humidifier at night. Within three weeks, her lips healed completely. She now uses only SPF lip balm during the day and avoids all flavored products.
Sarah’s case highlights how symptoms can persist when the root cause isn’t addressed—even with what seems like diligent care.
When to See a Doctor
Most cases of chapped lips resolve with proper care within two weeks. However, persistent or worsening symptoms may indicate a more serious condition requiring medical attention.
Seek professional help if you experience:
- Cracks that bleed or won’t heal after 14 days
- Painful sores or white patches on the lips
- Swelling, scaling, or dark discoloration
- Recurrent angular cheilitis (cracking at the corners of the mouth)
Potential diagnoses include:
- Angular cheilitis: Often caused by fungal or bacterial infection, especially in people with ill-fitting dentures or drooling during sleep.
- Eczematous cheilitis: A form of lip dermatitis triggered by allergens or irritants.
- Plasma cell cheilitis: A rare inflammatory condition requiring biopsy for diagnosis.
- Autoimmune disorders: Such as lupus or Crohn’s disease, which can present with oral symptoms.
“If your lips aren’t healing despite consistent care, it’s time to rule out infection or deficiency. Early intervention prevents long-term damage.” — Dr. Marcus Tran, Oral Medicine Specialist
Prevention Checklist: Keep Lips Healthy Long-Term
To prevent future flare-ups, follow this practical checklist:
- ✔ Switch to a fragrance-free, hypoallergenic lip balm or ointment
- ✔ Drink at least 8 glasses of water daily
- ✔ Use a humidifier in your bedroom at night
- ✔ Apply SPF 30+ lip protection every morning
- ✔ Avoid licking, biting, or picking at your lips
- ✔ Treat nasal congestion to reduce mouth breathing
- ✔ Consider a daily B-complex vitamin, especially if diet is limited
- ✔ Replace old lip products every 6 months to avoid bacterial contamination
Frequently Asked Questions
Can lip balm make chapping worse?
Yes. Balms containing menthol, camphor, phenol, or alcohol can irritate the skin and increase dryness. Overuse of any balm can also disrupt the lip’s natural repair process, creating dependency.
Why do my lips crack at the corners?
This is often angular cheilitis, caused by saliva buildup, fungal infection (like Candida), or nutrient deficiencies (especially B vitamins and iron). It’s common in people who breathe through their mouths or wear dentures.
Is Vaseline good for chapped lips?
Yes, pure petroleum jelly is one of the most effective treatments. It forms a protective barrier that locks in moisture without adding irritants. Just ensure it’s free of added fragrances or colors.
Conclusion: Heal Your Lips for Good
Chronic lip chapping isn’t something you have to live with. While lip balm is a helpful tool, it’s not a cure-all—especially if the product itself is part of the problem. True healing begins with identifying and removing irritants, supporting your body’s natural repair mechanisms, and protecting your lips from ongoing damage.
By switching to gentle, non-irritating products, staying hydrated, and addressing potential deficiencies, you can break the cycle of dryness and restore comfort. If problems persist, don’t hesitate to consult a dermatologist or healthcare provider. What seems like simple dryness could be a sign of an underlying condition that’s easily treatable once diagnosed.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?