Nipple pain is more common than many people realize, yet it often goes unspoken. Whether the discomfort is sharp, dull, burning, or throbbing, it can range from mildly annoying to severely disruptive. While occasional tenderness may be normal—especially around hormonal shifts—persistent or severe pain warrants attention. Understanding the underlying reasons behind nipple soreness helps distinguish between benign changes and signs that require medical evaluation.
This article breaks down the most frequent causes of nipple pain, highlights red flags that should not be ignored, and offers practical guidance on managing symptoms and knowing when to seek help.
Hormonal Fluctuations and Menstrual Cycle
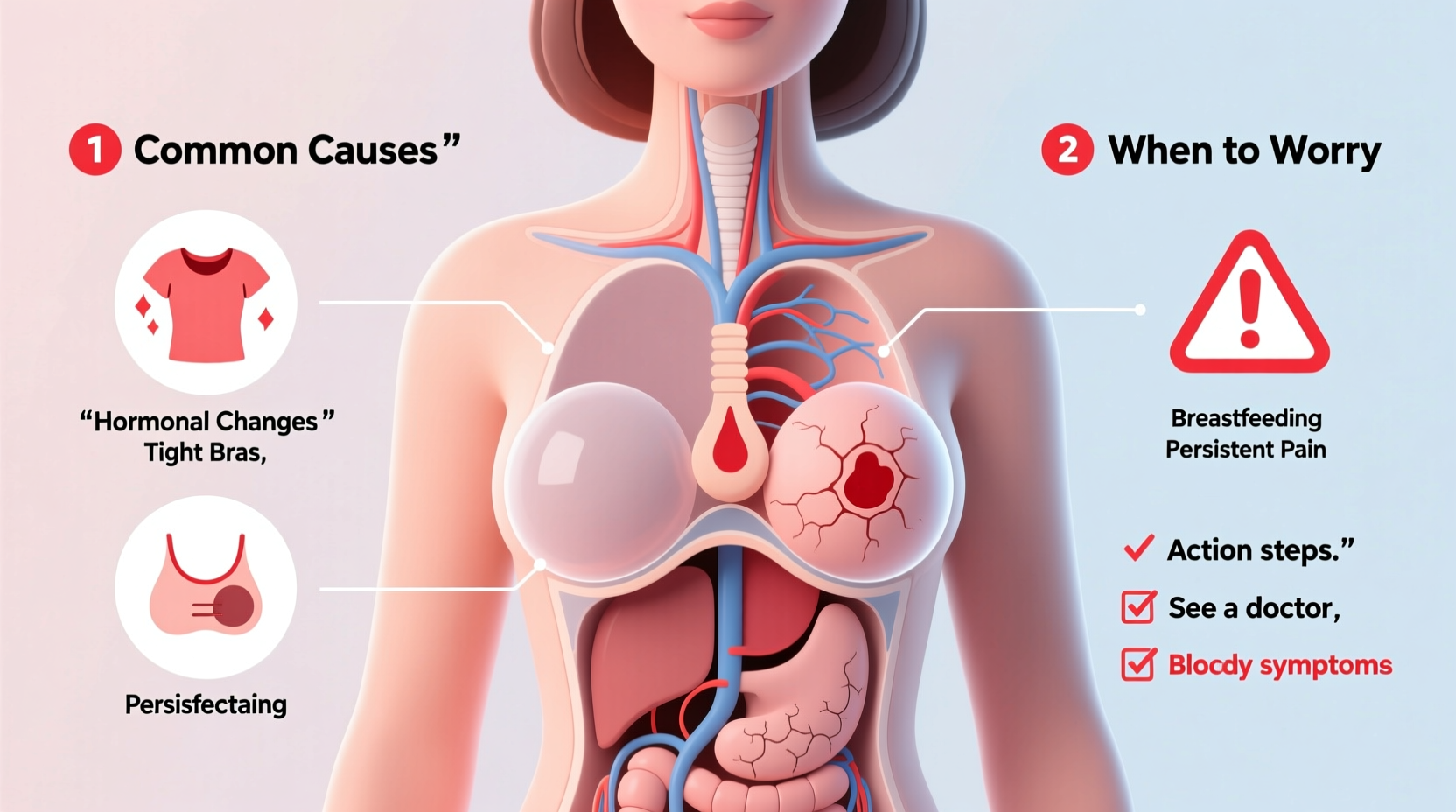
One of the most common reasons for nipple pain is linked to the menstrual cycle. Hormones such as estrogen and progesterone rise and fall throughout the month, particularly in the days leading up to menstruation. These fluctuations can cause breast tissue swelling and increased sensitivity, including in the nipples.
Many women experience nipple tenderness during the luteal phase (the two weeks before their period), often accompanied by breast fullness or lumpiness. This condition, known as cyclical mastalgia, typically resolves once menstruation begins.
Pregnancy and Breastfeeding
Nipple pain frequently occurs early in pregnancy due to hormonal changes preparing the body for lactation. Increased blood flow to the breasts and enlargement of milk ducts can make nipples extremely tender, sometimes even painful to touch.
During breastfeeding, pain may stem from improper latch, engorgement, or infections like mastitis. Cracked or blistered nipples are common among new mothers and usually improve with proper positioning and care.
“Nipple sensitivity in early pregnancy is normal, but persistent pain during breastfeeding should be evaluated for latch issues or infection.” — Dr. Lena Torres, OB-GYN Specialist
Skin Conditions and Irritation
The skin around the nipples is delicate and prone to irritation from external sources. Common dermatological causes include:
- Eczema: Can affect the areola and cause itching, flaking, and cracking.
- Psoriasis: May appear as scaly patches near or on the nipple.
- Allergic reactions: From laundry detergents, soaps, or fabrics in clothing.
- Fungal infections: Such as candidiasis, especially in breastfeeding individuals.
These conditions often respond well to topical treatments, but accurate diagnosis is essential to avoid worsening symptoms.
Physical Trauma and Friction
Exercise-induced nipple chafing is surprisingly common, especially among runners and cyclists. Repeated rubbing against clothing during long workouts can lead to soreness, bleeding, or even small abrasions.
Other forms of trauma include tight bras, rough handling, or accidental injury. In most cases, the pain subsides once the source of friction is removed and the skin heals.
Medications and Hormonal Therapies
Certain medications can induce nipple and breast tenderness as a side effect. These include:
- Birth control pills and hormonal IUDs
- Hormone replacement therapy (HRT)
- Antidepressants (particularly SSRIs)
- Some heart and blood pressure medications
If you’ve recently started a new medication and notice nipple pain beginning shortly after, discuss this with your healthcare provider. Adjustments may alleviate symptoms without compromising treatment goals.
When to Worry: Signs That Require Medical Attention
While most cases of nipple pain are harmless and temporary, certain symptoms should prompt immediate evaluation. These warning signs suggest possible underlying conditions such as infections, duct issues, or, rarely, breast cancer.
| Symptom | Possible Cause | Action |
|---|---|---|
| Unilateral pain (only one nipple) | Infection, blocked duct, Paget’s disease | See a doctor within 1–2 weeks |
| Nipple discharge (especially bloody or clear) | Duct ectasia, intraductal papilloma, malignancy | Seek evaluation promptly |
| Crusting, scaling, or ulceration | Paget’s disease of the breast | Urgent medical assessment needed |
| New lump near the nipple | Fibroadenoma, cyst, or tumor | Schedule diagnostic imaging |
| Redness, warmth, swelling with fever | Mastitis or abscess | Treat as medical emergency if severe |
Real Example: Recognizing Paget’s Disease
Sarah, a 52-year-old teacher, noticed her left nipple had become persistently itchy and cracked over several months. She initially assumed it was dry skin and used moisturizer, but the condition worsened, developing a crusty appearance. When she finally consulted her physician, a biopsy revealed Paget’s disease—a rare form of breast cancer affecting the nipple. Early detection allowed for targeted treatment, including surgery and radiation, leading to a favorable outcome.
Sarah’s case underscores the importance of not dismissing persistent changes, even if pain levels are mild.
Step-by-Step Guide to Managing Nipple Pain
Follow these steps to assess and manage nipple discomfort effectively:
- Track your symptoms: Note when the pain occurs, its intensity, and any associated factors (e.g., menstrual cycle, exercise).
- Inspect visually: Look for redness, rash, discharge, or changes in nipple shape.
- Review recent changes: Consider new products, medications, or activities that might contribute.
- Adjust clothing and hygiene: Switch to fragrance-free detergents and wear soft, non-abrasive fabrics.
- Try conservative measures: Use warm compresses, proper nursing techniques, or over-the-counter pain relief if appropriate.
- Consult a healthcare provider: If pain persists beyond a cycle, worsens, or includes any red-flag symptoms.
Frequently Asked Questions
Can stress cause nipple pain?
Stress does not directly cause nipple pain, but it can influence hormone balance and increase muscle tension, potentially exacerbating existing breast tenderness. Additionally, heightened anxiety may make individuals more aware of bodily sensations, amplifying perceived discomfort.
Is nipple pain a sign of breast cancer?
Rarely. Most nipple pain is unrelated to cancer. However, persistent unilateral pain accompanied by skin changes—such as dimpling, crusting, or discharge—should be evaluated. Paget’s disease, though uncommon, presents with nipple-specific symptoms and requires prompt diagnosis.
How long should I wait before seeing a doctor about nipple pain?
If the pain is cyclical and resolves with your period, monitoring is reasonable. However, if discomfort lasts more than two to three weeks, affects only one side, or includes other concerning symptoms, schedule an appointment within 7–10 days.
Checklist: When to Seek Medical Advice
- ☑ Pain localized to one nipple only
- ☑ Visible skin changes (scaling, ulceration, redness)
- ☑ Nipple discharge, especially if bloody or spontaneous
- ☑ New breast lump or thickening near the nipple
- ☑ Fever or signs of infection (warmth, swelling)
- ☑ No improvement after one full menstrual cycle
- ☑ History of breast cancer or high-risk factors
Conclusion
Nipple pain is often rooted in benign, treatable causes—from hormonal shifts to skin irritation or physical strain. But because it can occasionally signal something more serious, ignoring persistent or unusual symptoms isn’t worth the risk. By paying attention to patterns, making simple lifestyle adjustments, and knowing when to consult a professional, you can address discomfort confidently and protect your long-term health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?