Snoring is a common nighttime occurrence that affects millions of adults worldwide. While often dismissed as a mere annoyance, snoring can be a sign of deeper physiological issues, ranging from poor sleep posture to serious conditions like obstructive sleep apnea. Understanding the root causes of snoring and recognizing when it crosses the line from benign to concerning is essential for maintaining long-term health and ensuring restful sleep—for both the snorer and their partner.
What Causes Snoring?
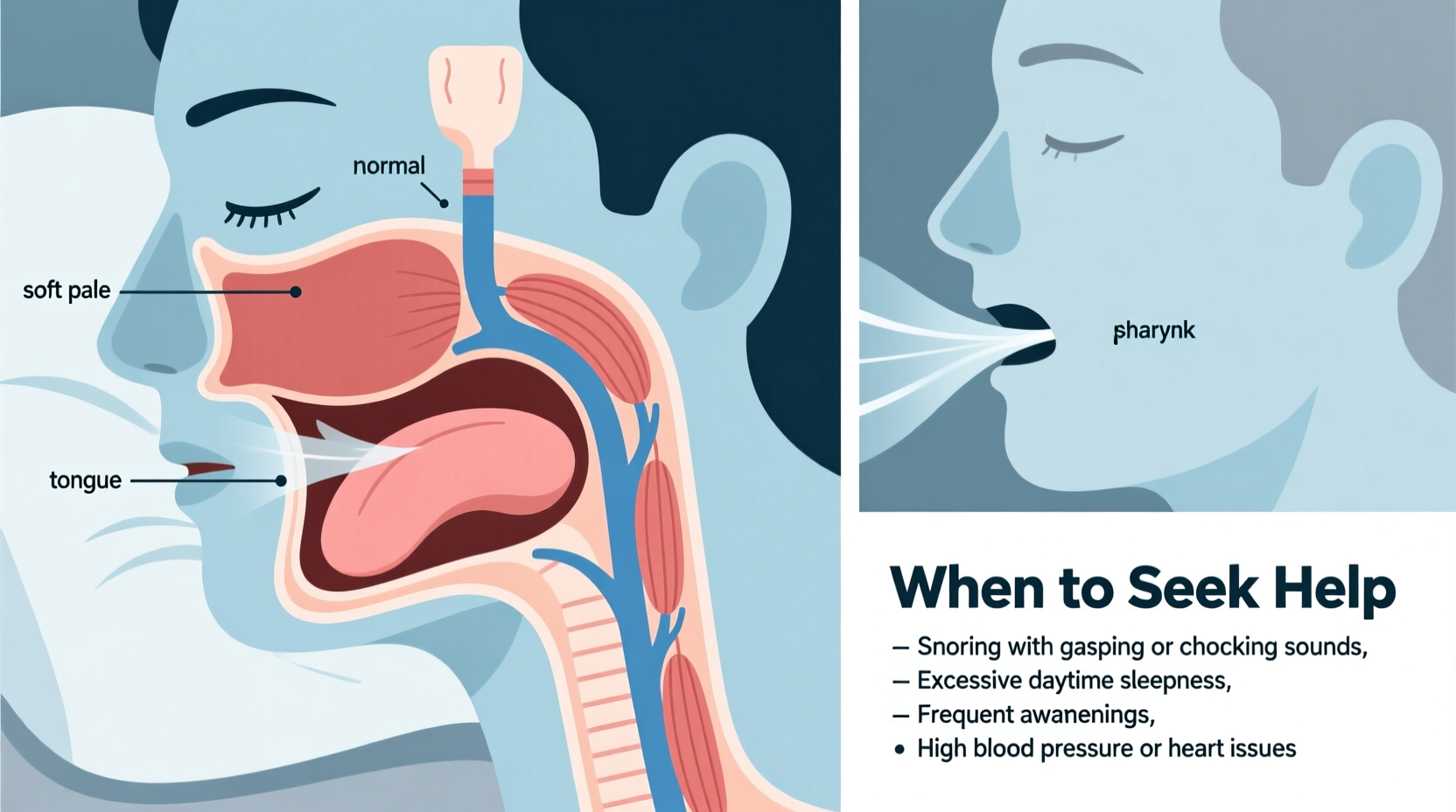
Snoring occurs when airflow through the mouth and nose is partially blocked during sleep. This obstruction causes the tissues in the throat—such as the soft palate, uvula, and tongue—to vibrate, producing the familiar rumbling or rattling sound. Several anatomical and lifestyle factors contribute to this restriction of airflow.
One primary cause is relaxed throat muscles. During deep sleep, especially REM sleep, muscles naturally relax. In some individuals, this relaxation leads to a narrowing of the airway. When combined with other risk factors such as excess weight or structural abnormalities, even slight muscle laxity can result in significant vibration.
Nasal congestion plays a major role as well. Allergies, colds, or a deviated septum can limit nasal breathing, forcing air through the mouth and increasing the likelihood of tissue vibration. Similarly, enlarged tonsils or adenoids—common in children but also present in some adults—can physically obstruct airflow.
Anatomical and Physiological Contributors
- Soft palate and uvula length: A longer soft palate or uvula increases surface area for vibration.
- Narrow airway: Some people are born with narrower throats, making them more prone to snoring.
- Tongue position: A large or posteriorly positioned tongue can fall back into the airway during sleep.
- Excess throat tissue: Weight gain, particularly around the neck, adds pressure on the airway.
Lifestyle Factors That Worsen Snoring
Beyond anatomy, daily habits significantly influence whether someone snores—and how loudly. These modifiable behaviors are often overlooked but represent critical leverage points for reducing or eliminating snoring.
Alcohol consumption before bedtime is a major contributor. Alcohol acts as a central nervous system depressant, intensifying muscle relaxation in the throat. Even moderate drinking in the evening can trigger snoring in otherwise non-snoring individuals.
Sedatives and certain medications, including antihistamines and muscle relaxants, produce similar effects. People taking these substances should be aware of their potential impact on breathing during sleep.
Smoking irritates the airways, leading to inflammation and swelling of nasal and throat tissues. Chronic smokers are statistically more likely to snore than non-smokers, and quitting can lead to noticeable improvement within weeks.
Sleep position matters too. Sleeping on your back allows gravity to pull the tongue and soft tissues backward, obstructing airflow. Side sleeping is generally recommended to minimize this effect.
“Over 50% of adults report occasional snoring, but persistent loud snoring should never be ignored—it’s often the first red flag for sleep-disordered breathing.” — Dr. Laura Nguyen, Sleep Medicine Specialist
Weight and Snoring: The Connection
Excess body weight, especially around the neck and upper airway, is one of the most significant predictors of chronic snoring. Fat deposits around the trachea compress the airway, reducing its diameter. Even a modest weight loss of 5–10% can dramatically reduce or eliminate snoring in overweight individuals.
This doesn’t mean only heavier individuals snore—thin people with narrow airways or structural issues can also be affected—but weight remains a key modifiable factor in treatment plans.
When Snoring Signals a Bigger Problem: Obstructive Sleep Apnea
Not all snoring is equal. Occasional, mild snoring due to temporary congestion or alcohol use is usually harmless. However, loud, chronic snoring accompanied by gasping, choking, or pauses in breathing may indicate obstructive sleep apnea (OSA).
In OSA, the airway becomes completely blocked for several seconds at a time, sometimes hundreds of times per night. The brain briefly wakes the person to resume breathing, disrupting sleep architecture and preventing deep, restorative rest. This cycle leads to excessive daytime fatigue, morning headaches, irritability, and long-term cardiovascular strain.
| Feature | Simple Snoring | Obstructive Sleep Apnea |
|---|---|---|
| Sound Level | Moderate, rhythmic | Loud, irregular, with pauses |
| Breathing Pauses | None | Frequent (10+ seconds) |
| Daytime Symptoms | None or mild | Excessive sleepiness, foggy thinking |
| Gasping or Choking | Rare | Common during sleep |
| Blood Pressure Impact | Minimal | Increased risk of hypertension |
Who Is at Higher Risk for Sleep Apnea?
- Men over 40 years old
- Postmenopausal women
- Individuals with a family history of OSA
- People with high blood pressure or type 2 diabetes
- Those with a neck circumference greater than 17 inches (43 cm)
When Should You Seek Medical Help?
Many people live with disruptive snoring for years without seeking help, assuming it’s normal or untreatable. But there are clear signs that indicate it’s time to consult a healthcare provider.
Red Flags That Require Evaluation
- Loud, disruptive snoring every night – If your snoring regularly wakes others or yourself, it’s not just a nuisance—it’s a signal.
- Witnessed breathing pauses – Any report of stopped breathing, even if brief, demands investigation.
- Excessive daytime sleepiness – Falling asleep during meetings, while driving, or after meals is not normal fatigue.
- Morning headaches or dry mouth – These suggest poor overnight oxygenation and mouth breathing.
- Difficulty concentrating or mood changes – Chronic sleep fragmentation impairs cognitive function and emotional regulation.
- High blood pressure or heart issues – Untreated sleep apnea increases the risk of stroke, heart attack, and arrhythmias.
Primary care physicians can conduct initial screenings, but diagnosis typically requires a sleep study. These can be done at home or in a sleep lab and measure breathing patterns, oxygen levels, brain activity, and limb movements throughout the night.
Mini Case Study: Recognizing the Signs
James, a 52-year-old accountant, had been snoring for over a decade. His wife initially joked about needing earplugs, but over time, she began noticing he would stop breathing for up to 15 seconds, followed by a loud gasp. James felt constantly tired despite sleeping eight hours. He struggled to focus at work and gained 30 pounds over two years. After his doctor ordered a home sleep test, James was diagnosed with moderate obstructive sleep apnea. With CPAP therapy, his energy returned within weeks, his blood pressure improved, and his wife reported peaceful nights again.
Effective Treatments and Management Strategies
The right treatment depends on the underlying cause and severity. Mild snoring may respond well to lifestyle adjustments, while sleep apnea often requires medical intervention.
Step-by-Step Guide to Reducing Snoring
- Assess your habits: Eliminate alcohol and sedatives 4–6 hours before bed.
- Change sleep position: Use a body pillow or positional device to encourage side sleeping.
- Address nasal issues: Treat allergies with antihistamines or use saline sprays and nasal strips.
- Lose weight if needed: Aim for gradual, sustainable weight reduction through diet and exercise.
- Upgrade your pillow: Use a supportive pillow that keeps your neck aligned.
- Consider oral appliances: Custom-fitted dental devices can reposition the jaw and tongue to open the airway.
- Seek professional evaluation: If symptoms persist, schedule a sleep consultation.
For diagnosed sleep apnea, continuous positive airway pressure (CPAP) machines remain the gold standard. These devices deliver steady airflow through a mask, keeping the airway open all night. Modern models are quieter and more comfortable than ever, with features like heated humidifiers and auto-adjusting pressure.
In select cases, surgery may be considered—such as removing tonsils, correcting a deviated septum, or performing procedures like uvulopalatopharyngoplasty (UPPP). However, surgical outcomes vary, and they are typically reserved for patients who cannot tolerate CPAP.
Checklist: Actions to Take If You or a Loved One Snores
- ☐ Monitor for breathing pauses or gasping during sleep
- ☐ Evaluate lifestyle factors (alcohol, smoking, medications)
- ☐ Try positional therapy (sleeping on your side)
- ☐ Use nasal strips or treat congestion
- ☐ Track daytime symptoms like fatigue or concentration issues
- ☐ Consult a doctor if snoring is loud, frequent, or disruptive
- ☐ Consider a sleep study if OSA is suspected
Frequently Asked Questions
Can children snore, and should I be concerned?
Yes, children can snore, often due to enlarged tonsils or adenoids. While occasional snoring is common, chronic snoring with pauses or restless sleep may indicate pediatric sleep apnea, which can affect growth, behavior, and academic performance. Evaluation by a pediatric ENT specialist is recommended.
Is snoring dangerous if I feel fine during the day?
Even without obvious symptoms, chronic snoring can strain the cardiovascular system over time. It may also progress to sleep apnea. Regular snoring should be monitored, especially if risk factors like obesity or high blood pressure are present.
Are anti-snoring apps or devices effective?
Some apps can record snoring and help identify patterns, which may support a discussion with a doctor. However, over-the-counter gadgets like chin straps or vibrating collars lack strong clinical evidence. For persistent snoring, professional assessment is far more reliable.
Conclusion: Listen to Your Body—and Your Partner
Snoring is more than a bedroom inconvenience—it’s a potential window into your respiratory and cardiovascular health. While not every snore signals danger, ignoring persistent, loud, or disruptive snoring can come at a cost. From strained relationships to increased risks of hypertension and heart disease, the consequences extend far beyond the bedroom.
The good news is that most causes of snoring are manageable. Simple changes in habits, posture, or weight can yield dramatic improvements. And when medical intervention is needed, treatments like CPAP are highly effective and can transform quality of life.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?