Snoring is a widespread issue affecting millions of adults worldwide. While often dismissed as a mere annoyance, chronic snoring can signal deeper health concerns and significantly disrupt sleep quality—for both the snorer and their partner. Understanding the root causes, recognizing risk factors, and exploring practical solutions are essential steps toward restful, healthier nights.
The Science Behind Snoring
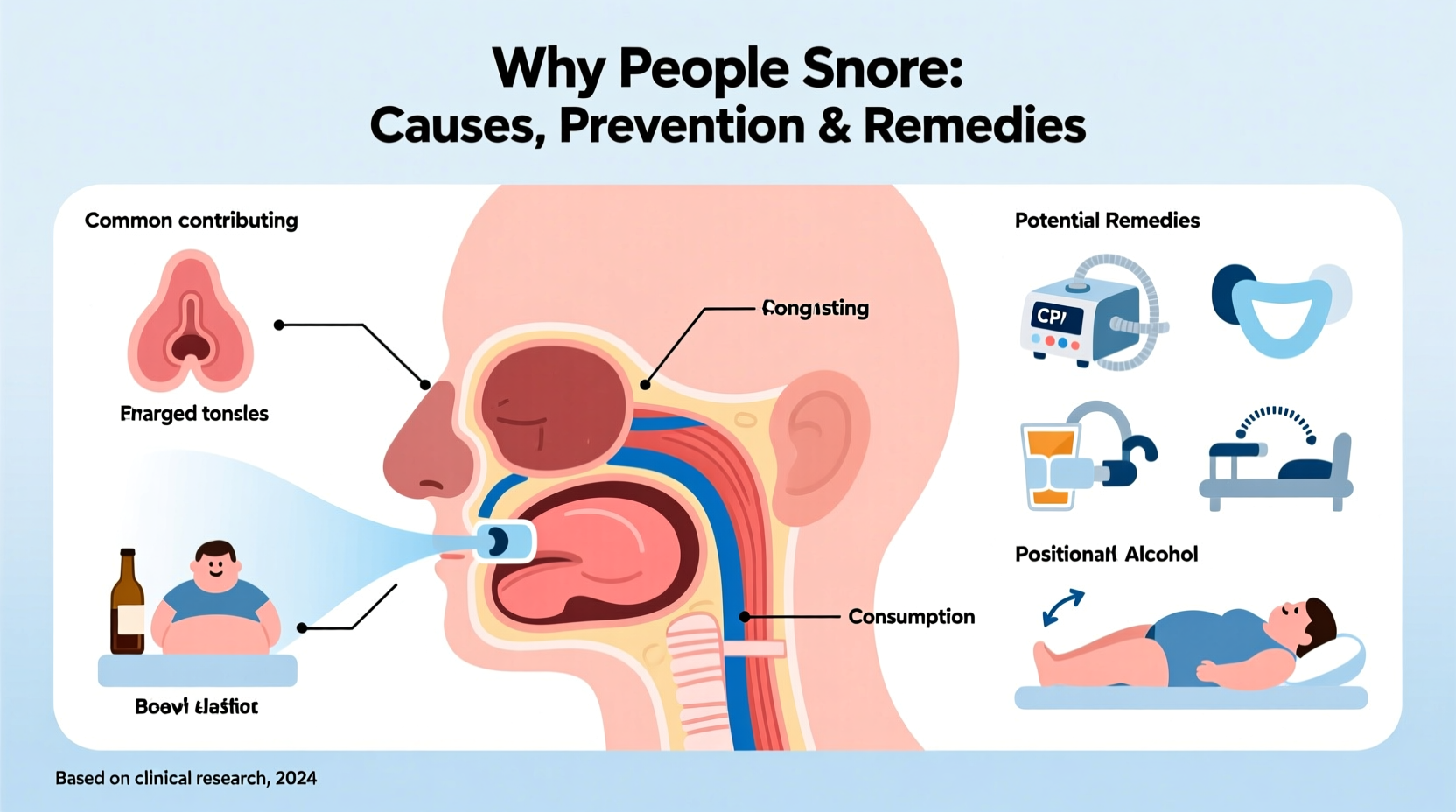
Snoring occurs when airflow through the mouth and nose is partially obstructed during sleep. This restriction causes the surrounding tissues—particularly the soft palate, uvula, and throat walls—to vibrate, producing the familiar rumbling or rasping sound. The intensity and frequency of snoring depend on the degree of airway narrowing and individual anatomy.
While occasional snoring may result from temporary conditions like congestion or alcohol consumption, habitual snoring could indicate underlying issues such as obstructive sleep apnea (OSA), obesity, or structural abnormalities in the airway.
Common Causes of Snoring
Several physiological and lifestyle factors contribute to snoring. Identifying these can help determine whether the issue is benign or requires medical attention.
- Anatomical structure: Enlarged tonsils, a long soft palate, or a deviated septum can narrow the airway.
- Obesity: Excess weight, especially around the neck, increases tissue pressure on the airway.
- Nasal congestion: Allergies, sinus infections, or structural issues like a crooked septum restrict airflow.
- Alcohol and sedatives: These relax throat muscles excessively, increasing the likelihood of airway collapse.
- Aging: Muscle tone in the throat decreases with age, making tissue vibration more likely.
- Sleep position: Back sleeping promotes tongue displacement into the airway.
“Snoring isn’t just a nuisance—it’s often a red flag for disrupted breathing during sleep.” — Dr. Lena Patel, Sleep Medicine Specialist
Prevention Strategies to Reduce Snoring
Many cases of snoring can be mitigated or eliminated through consistent lifestyle adjustments and environmental changes. Prevention is most effective when tailored to the individual’s primary triggers.
Weight Management
Even a modest weight loss of 5–10% can significantly reduce or eliminate snoring, particularly in individuals with excess neck circumference. Fat deposits around the upper airway compress the passage, increasing resistance during breathing.
Diet and Hydration
Staying well-hydrated helps keep mucosal secretions thin, reducing tissue stickiness and vibration. Conversely, dairy products before bedtime may increase mucus production in some people, worsening snoring.
Optimize Sleep Environment
Elevating the head of the bed by 4–6 inches using risers (not just extra pillows) encourages better airway alignment. Humidifiers can also prevent dry air from irritating nasal passages and throat tissues.
| Prevention Method | Effectiveness | Time to See Results |
|---|---|---|
| Lose 5–10% body weight | High (especially with OSA) | 2–6 months |
| Sleep on side | Moderate to high | Immediate |
| Avoid alcohol before bed | Moderate | Immediate |
| Treat allergies | Varies by cause | Days to weeks |
Potential Remedies and Treatments
When lifestyle changes aren’t enough, various interventions—from over-the-counter devices to clinical therapies—can offer relief.
Nasal Strips and Dilators
External nasal strips gently pull open the nostrils, improving airflow. Internal dilators fit inside the nose for similar effect. These are most helpful for those whose snoring stems from nasal congestion or narrow nasal valves.
Oral Appliances
Fitted by dentists specializing in sleep medicine, mandibular advancement devices (MADs) reposition the lower jaw and tongue forward, preventing airway blockage. They are effective for mild to moderate sleep apnea and non-apneic snoring.
CPAP Therapy
Continuous Positive Airway Pressure (CPAP) machines deliver steady airflow through a mask, keeping the airway open throughout the night. It remains the gold standard treatment for moderate to severe obstructive sleep apnea, which often presents with loud, disruptive snoring.
Surgical Options
In select cases, surgery may be recommended:
- Uvulopalatopharyngoplasty (UPPP): Removes excess tissue from the throat.
- Septoplasty: Corrects a deviated septum.
- Tonsillectomy: Removes enlarged tonsils, especially in children.
Mini Case Study: Mark’s Journey from Chronic Snoring to Restful Sleep
Mark, a 48-year-old accountant, had been snoring for over a decade. His wife reported frequent gasping episodes at night, and Mark often woke feeling unrefreshed. After his doctor suspected sleep apnea, he underwent a home sleep test confirming moderate OSA.
Initially resistant to CPAP, Mark tried weight loss and positional therapy. He lost 18 pounds over five months and used a wearable device that vibrates when he rolls onto his back. While this reduced snoring, follow-up testing showed persistent breathing interruptions.
He then began CPAP therapy. Within two weeks, both he and his wife noticed dramatic improvements. His daytime alertness increased, blood pressure stabilized, and his overall mood improved. Today, Mark credits CPAP with transforming his health and relationship.
Step-by-Step Guide to Addressing Snoring
- Assess the severity: Ask a partner about snoring patterns or record yourself sleeping.
- Identify contributing factors: Review alcohol use, medications, weight, and allergies.
- Try conservative measures: Change sleep position, lose weight, treat nasal congestion.
- Use supportive devices: Try nasal strips, humidifiers, or oral appliances.
- Consult a healthcare provider: If snoring persists or is accompanied by choking, daytime fatigue, or witnessed breathing pauses, seek evaluation for sleep apnea.
- Follow through with treatment: Adhere to prescribed therapies like CPAP and attend follow-up appointments.
FAQ
Can children snore, and should I be concerned?
Yes, children can snore. Occasional snoring due to colds is normal, but chronic snoring—especially with mouth breathing, bedwetting, or behavioral issues—may indicate enlarged tonsils or adenoids. Pediatric sleep apnea requires medical evaluation.
Is snoring always a sign of sleep apnea?
No. Many people snore without having sleep apnea. However, loud, irregular snoring accompanied by gasping, choking, or excessive daytime sleepiness increases the likelihood of OSA and warrants professional assessment.
Are anti-snoring apps effective?
Some apps can track snoring sounds and sleep patterns, helping identify trends. However, they cannot diagnose sleep disorders. Use them as awareness tools, not substitutes for clinical testing.
Conclusion
Snoring is more than a nighttime disturbance—it’s a potential indicator of compromised sleep and long-term health risks. By understanding its causes, taking proactive steps to prevent it, and seeking appropriate remedies when needed, individuals can reclaim quiet, restorative sleep. Whether through simple habit changes or medical intervention, addressing snoring improves not only personal well-being but also the quality of relationships and daily functioning.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?