Waking up suddenly at 3 a.m., staring at the ceiling, heart calm but mind racing—this experience is more common than most realize. It’s not just an occasional disturbance; for many, it’s a recurring pattern that undermines sleep quality, energy levels, and overall well-being. While the clock strikes 3 a.m. with eerie consistency, the reasons behind this phenomenon are complex, involving biology, psychology, and lifestyle. Understanding why this happens—and how to respond—is essential for anyone seeking deeper, uninterrupted rest.
The Science Behind Early Morning Awakenings
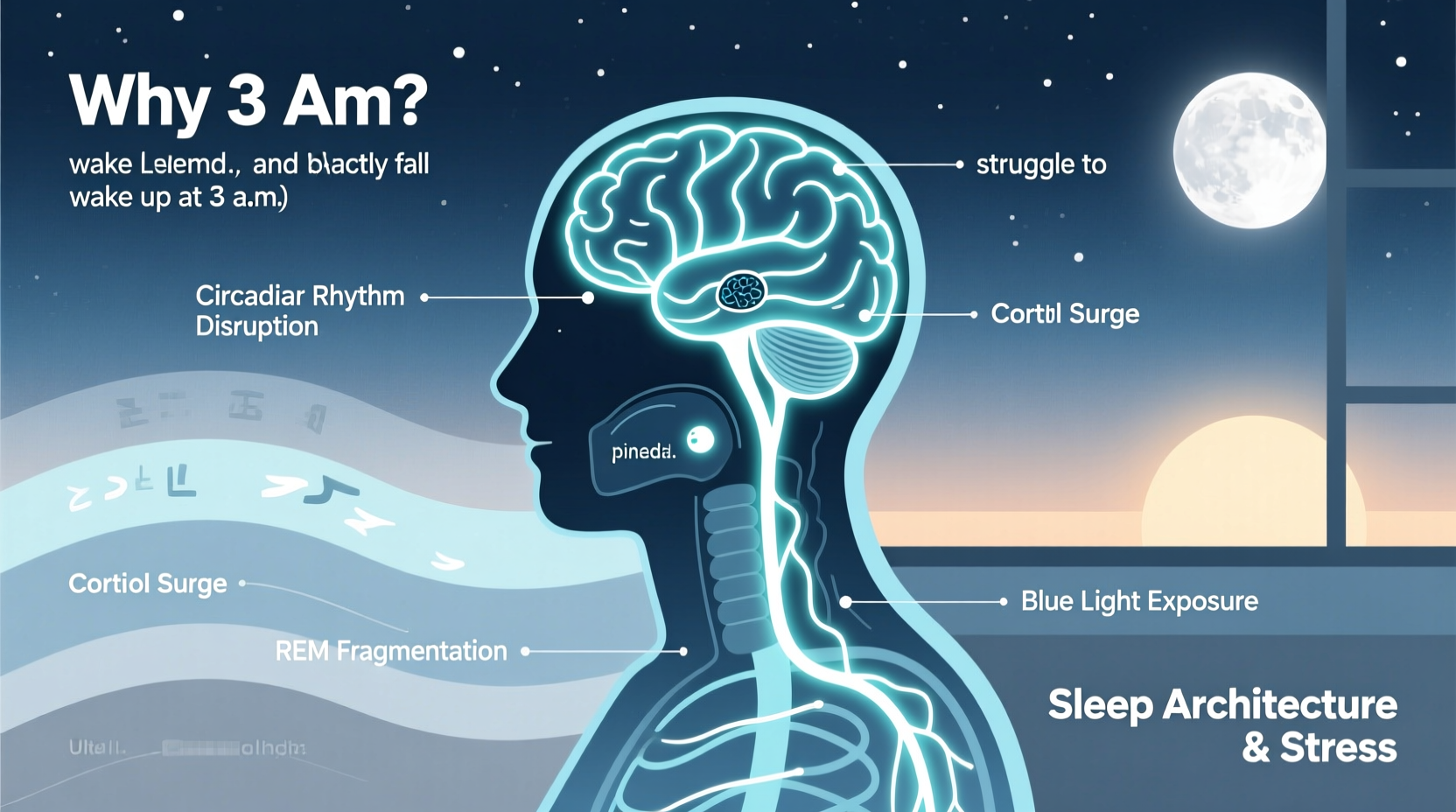
Sleep isn’t a uniform state of unconsciousness. It cycles through stages: light sleep, deep sleep, and REM (rapid eye movement) sleep, each lasting roughly 90 minutes. By the early morning hours—typically between 2 a.m. and 4 a.m.—you’re in your final sleep cycles, which are richer in REM sleep. This stage is associated with heightened brain activity, vivid dreams, and lighter sleep, making awakenings more likely.
At around 3 a.m., cortisol—a hormone involved in wakefulness—begins to rise as part of the body’s natural circadian rhythm. This prepares you for waking in the morning. However, if stress, anxiety, or poor sleep regulation is present, this hormonal shift can trigger full awakening instead of gradual transition. Additionally, melatonin—the sleep-promoting hormone—peaks earlier in the night and begins to decline by 3 a.m., reducing its ability to keep you asleep.
“Waking at 3 a.m. often coincides with a natural dip in sleep pressure and a surge in alerting signals from the brain. For some, this becomes a daily trap.” — Dr. Lena Reyes, Sleep Neurologist, Stanford Center for Sleep Sciences
Common Causes of 3 a.m. Wakefulness
While biological rhythms set the stage, several factors can turn a normal physiological shift into chronic sleep disruption.
Stress and Anxiety
Mental load accumulates during the day and often resurfaces at night. When awake at 3 a.m., the quiet darkness amplifies intrusive thoughts. Financial worries, work deadlines, relationship concerns—these can dominate the mind when distractions are absent. The brain, no longer occupied by external stimuli, defaults to rumination.
Disrupted Circadian Rhythms
Modern lifestyles interfere with natural sleep-wake cycles. Exposure to blue light from screens after sunset delays melatonin release, pushing sleep onset later. Inconsistent bedtimes, shift work, or frequent travel across time zones further confuse the internal clock, increasing the likelihood of mid-sleep awakenings.
Underlying Health Conditions
Certain medical issues contribute to fragmented sleep. Sleep apnea causes breathing interruptions that jolt the sleeper awake—often without full awareness. Gastroesophageal reflux disease (GERD) can flare when lying flat, causing discomfort that disrupts sleep. Hormonal imbalances, such as those seen in menopause or hyperthyroidism, also affect sleep stability.
Lifestyle and Environmental Triggers
Diet plays a role. Consuming caffeine after noon, heavy meals late at night, or alcohol before bed may seem harmless but significantly impact sleep architecture. Alcohol, for instance, suppresses REM sleep early in the night, leading to a REM rebound later—often around 3 a.m.—which increases dream intensity and arousal.
Environmental factors like room temperature, noise, or an uncomfortable mattress can also prompt awakenings. A bedroom that’s too warm (above 68°F) interferes with the body’s natural drop in core temperature needed for sustained sleep.
Breaking the Cycle: Practical Solutions
Reversing chronic 3 a.m. awakenings requires a multi-pronged approach. Addressing root causes—not just symptoms—is key to restoring restorative sleep.
Establish a Consistent Sleep Schedule
Going to bed and waking up at the same time every day—even on weekends—reinforces your circadian rhythm. This consistency reduces the chance of premature awakenings by aligning your internal clock with environmental cues like light and darkness.
Optimize Your Sleep Environment
Create a bedroom sanctuary designed for sleep. Use blackout curtains, maintain a cool temperature (60–67°F), and eliminate electronic distractions. Consider white noise machines if external sounds are disruptive.
Practice Cognitive Behavioral Techniques
For those caught in cycles of nighttime anxiety, cognitive behavioral therapy for insomnia (CBT-I) is highly effective. It helps reframe negative thoughts about sleep and teaches relaxation strategies such as progressive muscle relaxation and guided imagery.
| Factor | Do | Avoid |
|---|---|---|
| Evening Routine | Wind down with reading or gentle stretching | Screen use, intense exercise |
| Diet | Light snack if hungry; herbal tea like chamomile | Caffeine, alcohol, large meals |
| Bedroom Use | Reserve bed only for sleep and intimacy | Working, watching TV, scrolling |
| Night Awakenings | Stay calm; leave bed if awake >20 min | Checking the clock repeatedly |
Step-by-Step Guide to Managing 3 a.m. Wakeups
If you consistently wake at 3 a.m., follow this structured response plan to prevent frustration and improve long-term outcomes.
- Stay Calm: Remind yourself that brief awakenings are normal. Panic increases heart rate and makes re-sleeping harder.
- Don’t Check the Time: Seeing 3:07 a.m. triggers anxiety about lost sleep. Turn clocks away from view.
- Breathe Deeply: Try the 4-7-8 method: inhale for 4 seconds, hold for 7, exhale slowly for 8. Repeat 4 times.
- Leave Bed If Needed: After 20–30 minutes of wakefulness, move to another dimly lit room. Read a physical book until drowsy.
- Resume Sleep Only When Sleepy: Return to bed only when yawning or feeling physically heavy.
- Reflect Daily: Keep a sleep journal noting bedtime, wake time, diet, stress levels, and nighttime awakenings.
Real-Life Example: Maria’s Journey Back to Rest
Maria, a 42-year-old project manager, began waking at 3 a.m. three times a week. Initially dismissed as stress, the pattern persisted for months. She’d lie awake, worrying about upcoming presentations and her children’s school schedules. Attempts to “force” herself back to sleep only increased frustration.
After consulting a sleep specialist, Maria discovered she was consuming afternoon lattes and working late on her laptop. Her wind-down routine included checking emails in bed. She started tracking her habits and implemented changes: cutting caffeine after 12 p.m., using blue-light filters, and practicing mindfulness meditation at 8 p.m.
Within four weeks, her awakenings dropped to once a week. She now keeps a notebook by the bed to jot down thoughts if they arise, then uses diaphragmatic breathing to return to sleep. “I realized I wasn’t broken,” she said. “I just needed better tools.”
When to Seek Professional Help
Occasional 3 a.m. awakenings are normal. But if they happen more than three nights a week for over a month and impair daytime functioning, it may indicate chronic insomnia. Other red flags include:
- Excessive daytime fatigue
- Irritability or difficulty concentrating
- Reliance on sleep aids
- Symptoms of sleep apnea (snoring, gasping)
In such cases, a visit to a healthcare provider or sleep clinic is warranted. Polysomnography (sleep study) can diagnose underlying conditions. CBT-I, prescribed medications, or treatment for sleep apnea may be recommended.
“Insomnia is not just ‘not sleeping.’ It’s a learned pattern of arousal that can be unlearned with the right support.” — Dr. Alan Zhou, Clinical Psychologist & Sleep Therapist
Frequently Asked Questions
Is waking at 3 a.m. a sign of depression?
It can be. Early morning awakening—waking hours before intended and unable to return to sleep—is a diagnostic criterion for major depressive disorder. However, it’s not definitive on its own. If accompanied by low mood, loss of interest, or fatigue, consult a mental health professional.
Why do I feel more alert at 3 a.m. than during the day?
This paradox occurs because nighttime wakefulness activates the brain’s default mode network, linked to introspection and creativity. With fewer distractions, thoughts feel sharper. But this alertness is misleading—it’s driven by stress hormones, not true cognitive readiness.
Can supplements help me stay asleep?
Melatonin may help regulate timing but is less effective for maintaining sleep. Magnesium glycinate and L-theanine show promise in promoting relaxation. Always consult a doctor before starting supplements, especially if taking other medications.
Checklist: How to Prevent 3 a.m. Wakeups
- ✅ Set a consistent bedtime and wake-up time
- ✅ Eliminate caffeine after noon
- ✅ Avoid alcohol within 3 hours of bedtime
- ✅ Create a relaxing pre-sleep routine (e.g., bath, reading)
- ✅ Keep your bedroom cool, dark, and quiet
- ✅ Limit screen exposure 1 hour before bed
- ✅ Practice mindfulness or meditation to reduce nighttime anxiety
- ✅ Use your bed only for sleep and intimacy
- ✅ Track sleep patterns in a journal or app for 2 weeks
- ✅ Consult a sleep specialist if problems persist beyond a month
Conclusion: Reclaim Your Night, Restore Your Energy
Waking at 3 a.m. isn’t mystical or inevitable—it’s often the result of intersecting lifestyle, biological, and psychological factors. The good news is that most causes are modifiable. Small, consistent changes in routine, environment, and mindset can dramatically improve sleep continuity. You don’t have to resign yourself to years of silent ceiling-staring. By understanding your body’s rhythms and responding with intention, you can transform fragmented nights into restorative ones.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?