Platelets, also known as thrombocytes, are tiny blood cells essential for clotting. When their numbers fall below normal—typically less than 150,000 platelets per microliter of blood—it leads to a condition called thrombocytopenia. This drop can range from mild to severe, increasing the risk of excessive bleeding or bruising. Understanding why platelets drop is crucial for timely diagnosis and effective management.
What Are Platelets and Why Do They Matter?
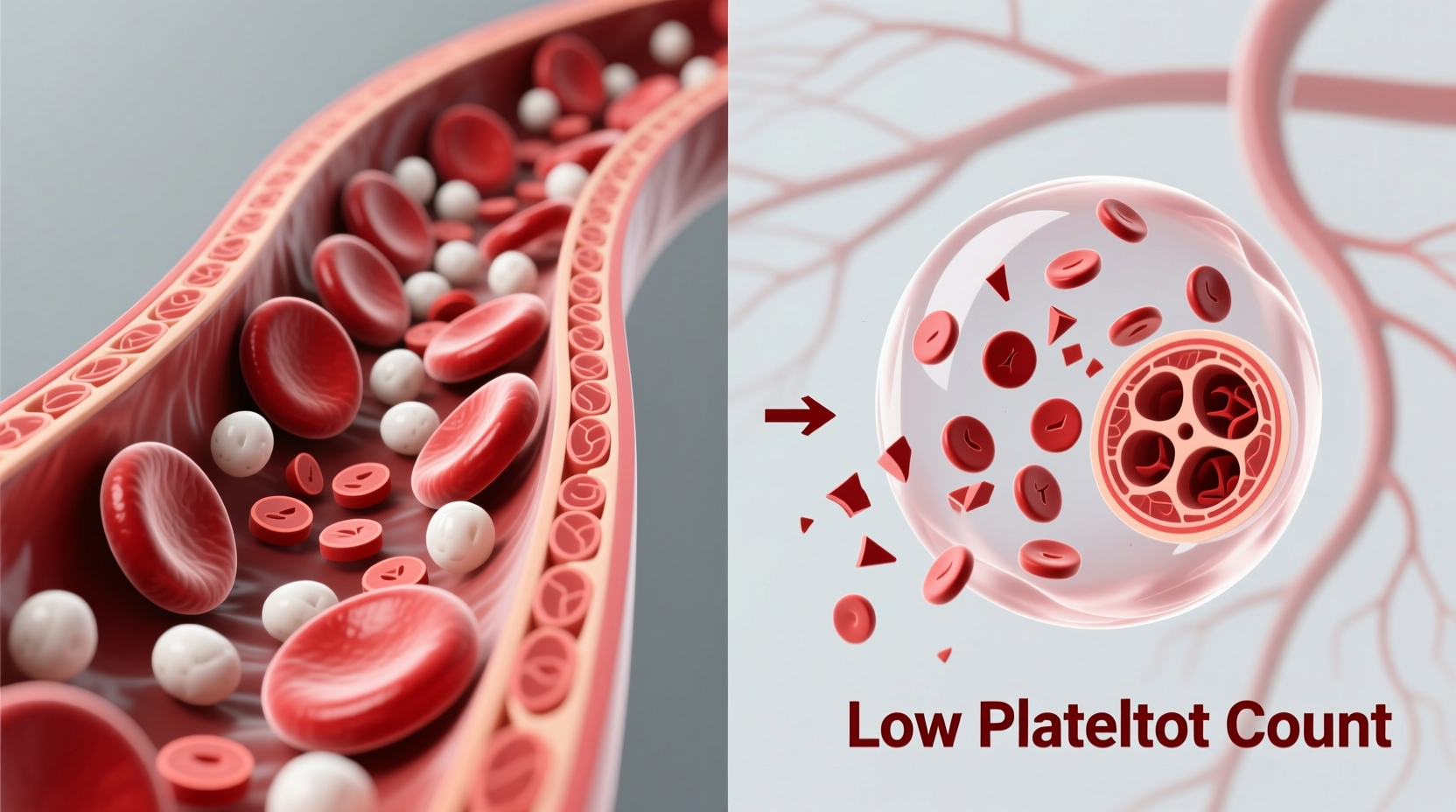
Produced in the bone marrow, platelets circulate in the bloodstream and rush to sites of injury to form clots and prevent blood loss. A healthy platelet count ranges between 150,000 and 450,000 per microliter. When counts fall significantly, even minor injuries can lead to prolonged bleeding, spontaneous nosebleeds, or internal hemorrhaging in extreme cases.
The body maintains platelet levels through a balance of production, consumption, and destruction. Disruptions in any of these processes can cause a decline. The reasons are diverse—from medication side effects to autoimmune disorders—and identifying the root cause is key to proper treatment.
Common Causes of Low Platelet Count
Thrombocytopenia arises from one or more of three primary mechanisms: decreased production, increased destruction, or sequestration (trapping) of platelets. Below are the most frequent causes grouped by category:
1. Decreased Platelet Production
When the bone marrow fails to produce enough platelets, counts drop. Contributing factors include:
- Viral infections: Hepatitis C, HIV, Epstein-Barr virus, and dengue fever can impair bone marrow function.
- Leukemia and other cancers: Cancerous cells may crowd out healthy marrow tissue.
- Chemotherapy and radiation: These treatments damage rapidly dividing cells, including those in the bone marrow.
- Nutritional deficiencies: Lack of vitamin B12, folate, or iron hampers cell production.
- Alcohol abuse: Chronic alcohol use suppresses bone marrow activity.
2. Increased Platelet Destruction
In some conditions, the immune system mistakenly targets and destroys platelets:
- Immune thrombocytopenia (ITP): An autoimmune disorder where antibodies attack platelets.
- Drug-induced thrombocytopenia: Medications like heparin, quinine, or certain antibiotics trigger immune responses.
- Thrombotic thrombocytopenic purpura (TTP): A rare disorder causing widespread microclot formation and platelet consumption.
- Hemolytic uremic syndrome (HUS): Often linked to E. coli infection, it damages red blood cells and platelets.
3. Platelet Sequestration
Sometimes platelets are removed from circulation without being destroyed:
- Splenomegaly (enlarged spleen): An enlarged spleen traps excess platelets, reducing circulating levels.
Recognizing Symptoms and When to Seek Help
Many people with mild thrombocytopenia show no symptoms. However, as counts fall, warning signs appear:
- Petechiae—tiny red or purple spots on the skin, especially on legs
- Easy or excessive bruising (purpura)
- Nosebleeds or gum bleeding that won’t stop
- Prolonged bleeding from cuts
- Heavy menstrual flow
- Blood in urine or stool
- Fatigue (often due to underlying illness)
“Not all low platelet counts require emergency intervention, but persistent unexplained bruising should never be ignored.” — Dr. Linda Reyes, Hematology Specialist
Severe thrombocytopenia (platelets below 20,000/µL) increases the risk of spontaneous internal bleeding, including intracranial hemorrhage—a life-threatening condition requiring immediate care.
Diagnosis and Testing Process
A complete blood count (CBC) is the first step in diagnosing low platelets. If results show thrombocytopenia, further tests help determine the cause:
| Test | Purpose | What It Reveals |
|---|---|---|
| Peripheral blood smear | Microscopic examination of blood cells | Abnormal size, shape, or distribution of platelets |
| Bone marrow biopsy | Assess marrow health and cell production | Detects leukemia, aplasia, or fibrosis |
| Autoimmune panels | Check for immune-mediated destruction | Confirms ITP or lupus-related causes |
| Liver and kidney function tests | Evaluate organ involvement | Rules out cirrhosis or renal failure as contributors |
| Viral serology | Test for infections affecting platelets | Identifies HIV, hepatitis, or dengue |
Doctors also review medical history, medications, alcohol use, and recent illnesses to build a comprehensive picture.
Treatment Options Based on Cause
Treatment depends entirely on the underlying reason for the drop. There is no one-size-fits-all solution.
Mild Cases
If platelet counts are only slightly low and no bleeding occurs, monitoring may be sufficient. Addressing reversible factors—like stopping a triggering medication or treating an infection—can restore counts naturally.
Immune Thrombocytopenia (ITP)
- Corticosteroids: Prednisone reduces immune system activity.
- IVIG (intravenous immunoglobulin): Provides temporary boost by blocking platelet destruction.
- Rituximab: Targets B-cells involved in antibody production.
- TPO receptor agonists: Romiplostim or eltrombopag stimulate platelet production.
Severe or Acute Cases
In emergencies such as active bleeding or very low counts, platelet transfusions may be necessary. However, they are used cautiously—especially in conditions like TTP—because they can worsen clotting complications.
Lifestyle and Supportive Measures
Avoid activities with high injury risk, such as contact sports. Use soft-bristle toothbrushes and electric razors to minimize bleeding. Limit alcohol and NSAIDs (e.g., ibuprofen), which can impair platelet function.
Real-World Example: A Case of Drug-Induced Thrombocytopenia
Sarah, a 48-year-old woman, began taking a new antibiotic for a urinary tract infection. Within a week, she noticed small red dots on her lower legs and developed frequent nosebleeds. Her CBC revealed a platelet count of 42,000/µL. After reviewing her medication history, her physician suspected drug-induced thrombocytopenia. The antibiotic was discontinued, and within 10 days, her platelet levels returned to normal without additional treatment. This case highlights how quickly certain drugs can impact platelet counts—and how prompt recognition can prevent serious complications.
Prevention and Monitoring Checklist
While not all causes of low platelets can be prevented, proactive habits reduce risks and support early detection:
- Review all medications annually with your doctor, including supplements.
- Limit alcohol consumption to moderate levels or less.
- Get routine blood work, especially if you have chronic conditions.
- Avoid overuse of NSAIDs unless medically supervised.
- Report unusual bruising or bleeding promptly.
- Manage autoimmune conditions with specialist care.
- Practice safe sex and avoid IV drug use to reduce viral infection risks.
Frequently Asked Questions
Can stress cause low platelets?
Stress alone doesn’t directly reduce platelet production, but chronic stress may exacerbate autoimmune conditions like ITP. While not a primary cause, it can influence immune regulation and disease flares.
Is low platelet count always dangerous?
No. Mild thrombocytopenia often causes no symptoms and resolves on its own. Danger increases when counts fall below 50,000/µL, especially if bleeding signs appear. Context matters—underlying cause and overall health are critical.
Can diet improve platelet count?
While no single food cures thrombocytopenia, a balanced diet rich in vitamin B12, folate, iron, and antioxidants supports healthy blood cell production. Foods like leafy greens, eggs, lean meats, and citrus fruits contribute to overall hematologic health.
Conclusion: Taking Control of Your Blood Health
Understanding why platelets drop empowers individuals to seek timely care and participate actively in their treatment. Whether caused by medication, infection, or an immune disorder, identifying the root issue is the first step toward recovery. With proper diagnosis, targeted therapy, and lifestyle awareness, most people with low platelet counts can manage their condition effectively and safely.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?