Suddenly seeing flashes of light while in a dark room or with eyes closed can be startling. These brief bursts of illumination—often described as streaks, sparks, or flickering lights—are not always a sign of trouble, but they can sometimes signal underlying health issues. While many experiences are benign and fleeting, others may point to changes in the eye, brain activity, or neurological function. Understanding the science behind these visual events helps distinguish between normal physiological quirks and symptoms that require medical attention.
These phenomena occur across age groups and often go unreported because people assume they’re imagining things or experiencing momentary glitches. However, flashes of light in darkness are rooted in real biological processes involving the retina, optic nerve, and visual cortex. Some are linked to aging, while others arise from migraines, trauma, or systemic diseases. This article explores the primary causes, mechanisms, risk factors, and clinical significance of perceiving light without an external source.
The Science Behind Seeing Light Without Light
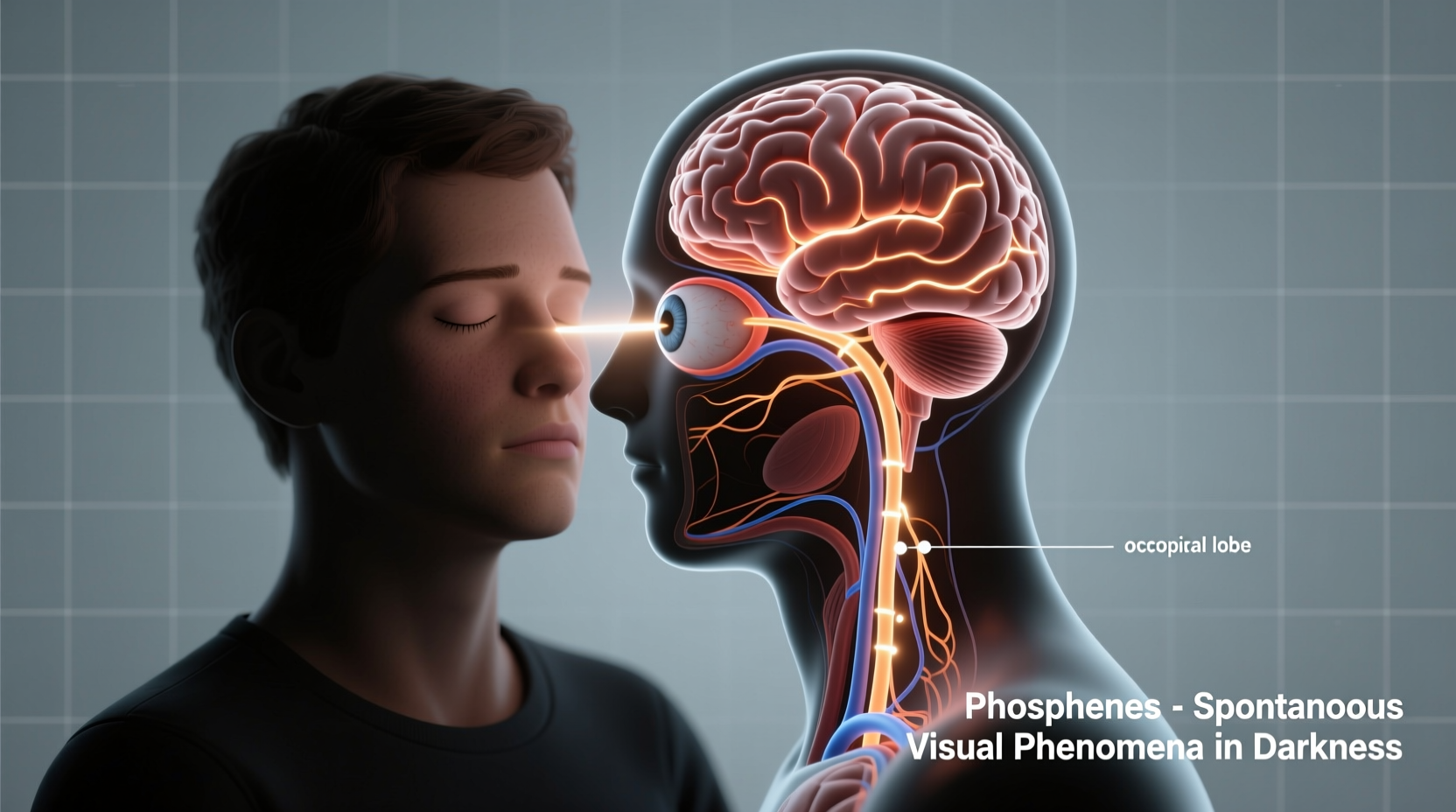
The human visual system is designed to detect photons through photoreceptor cells in the retina. But it doesn’t need actual light to generate the sensation of brightness. Mechanical pressure, electrical stimulation, or chemical changes within the eye or brain can trigger signals that the brain interprets as light—a phenomenon known as phosphene.
Phosphenes have been documented for centuries. Ancient physicians noted that rubbing the eyes could produce starbursts of color and light. Modern neuroscience confirms this: stimulating the retina or visual cortex artificially (even via magnetic fields) can evoke vivid perceptions of light patterns. In everyday life, phosphenes appear during sudden movements, pressure on the eyeball, or transitions between light and dark environments.
In low-light conditions, the retina becomes more sensitive. When internal stimuli activate retinal cells—such as vitreous gel movement pulling on the retina—these signals travel along the optic nerve just like real visual input. The brain receives them and constructs an image of flashing light, even though no external source exists.
Common Causes of Flashes in Darkness
Not all flashes indicate pathology. Several normal and age-related changes account for most cases:
- Vitreous detachment: As we age, the gel-like substance inside the eye (vitreous humor) shrinks and pulls away from the retina. This tugging stimulates retinal nerves, causing brief arcs or streaks of light, especially noticeable in dim settings.
- Migraine aura: Some individuals experience visual disturbances before or during migraines. These include zigzag lines, shimmering spots, or pulsating lights—even in total darkness. Known as ocular or retinal migraines, they typically last 20–30 minutes and resolve without lasting damage.
- Eye pressure or trauma: Rubbing the eyes, sneezing forcefully, or minor impacts can mechanically stimulate the retina, producing temporary flashes.
- Low blood pressure or orthostatic hypotension: Standing up too quickly can reduce blood flow to the brain momentarily, leading to lightheadedness and visual snow or sparkles, particularly in dark-adapted states.
- Sleep onset hallucinations: During the transition into sleep, the brain may generate sensory experiences, including flashes of light, geometric shapes, or colors—commonly reported by those with irregular sleep patterns.
While these causes are generally harmless, their frequency and context matter. A single flash after blinking hard is likely insignificant; recurrent episodes over days warrant evaluation.
When Flashes Signal Serious Eye Conditions
Some causes of light flashes are medically significant and demand prompt attention. The most critical concern is retinal detachment—a condition where the retina peels away from its supportive tissue, potentially leading to permanent vision loss if untreated.
Flashes associated with retinal issues tend to be:
- Repetitive and recurring over hours or days
- Localized to one area of the visual field
- Accompanied by a sudden increase in floaters (dark spots or cobwebs)
- Followed by a curtain-like shadow moving across vision
According to Dr. Alan Kimura, Retina Specialist at Pacific Eye Institute:
“Patients often dismiss early flashes as ‘eye strain’ or fatigue. But when combined with new floaters, especially after age 50, it’s crucial to get examined within 24–48 hours. Early intervention prevents blindness in 90% of retinal detachment cases.”
Other concerning conditions include:
- Posterior vitreous detachment (PVD): Though common and usually benign, PVD carries a 10–15% risk of causing retinal tears due to strong traction on the retina.
- Diabetic retinopathy: Advanced diabetes weakens retinal blood vessels, increasing the chance of hemorrhage or tractional detachment, both capable of triggering abnormal light signals.
- Ocular inflammation (uveitis): Inflammation inside the eye can irritate neural layers, mimicking flash-like symptoms.
Risk Factors for Pathological Flashes
| Risk Factor | Description | Action Recommended |
|---|---|---|
| Age over 50 | Natural vitreous shrinkage increases risk of retinal traction | Annual eye exams with pupil dilation |
| Nearsightedness (myopia) | Longer eyeball shape stresses peripheral retina | Monitor for sudden visual changes |
| Prior eye surgery or trauma | Structural vulnerability increases detachment risk | Immediate assessment after new symptoms |
| Family history of retinal issues | Genetic predisposition to weak retinal areas | Prophylactic laser treatment if indicated |
Neurological Origins: Migraines and Beyond
Not all flashes originate in the eye. The brain’s visual cortex plays a central role in interpreting sensory data—and sometimes generates false positives. Visual aura linked to migraines is one of the most frequent neurological explanations.
In migraine with aura, cortical spreading depression—a wave of altered neuronal activity—moves across the occipital lobe. This disrupts normal processing and creates illusions of light, shimmering zones, or blind spots. These episodes:
- Occur with or without headache
- Last 5–60 minutes
- Are bilateral (affect both eyes)
- Often progress gradually rather than appearing suddenly
A less common but important differential diagnosis is occipital epilepsy. Seizures originating in the visual cortex can cause brief, repetitive flashes—sometimes mistaken for eye problems. Unlike migraines, epileptic visual auras may be followed by muscle twitching, confusion, or loss of awareness.
“Many patients come in worried about their eyes, only to discover the issue lies in brain signaling,” says Dr. Lena Patel, Neuro-Ophthalmologist at Boston Vision Center. “EEG testing and detailed history-taking are key to accurate diagnosis.”
Mini Case Study: Recognizing a Medical Emergency
Sarah Thompson, a 58-year-old librarian, began noticing intermittent flashes in her right eye while reading in bed. At first, she assumed it was eye fatigue. Over three days, the flashes became more frequent, and she started seeing dozens of new floaters. One evening, she noticed a dark shadow creeping into her lower peripheral vision.
She called her optometrist the next morning. After urgent dilation, the doctor detected a small retinal tear caused by posterior vitreous detachment. Sarah was referred immediately to a retinal surgeon, who performed laser photocoagulation to seal the tear. Within a week, the flashes subsided, and her vision stabilized.
This case illustrates how timely action prevented full detachment. Had Sarah delayed care, she might have faced irreversible central vision loss.
Step-by-Step Guide: What to Do If You See Flashes in the Dark
If you begin experiencing unexplained flashes, follow this evidence-based protocol:
- Assess the pattern: Note whether flashes are occasional or constant, unilateral or bilateral, and whether they coincide with headaches or dizziness.
- Check for additional symptoms: Look for increased floaters, blurred vision, shadows, or vision loss—especially in peripheral sight.
- Avoid self-diagnosis: Don’t assume it’s “just stress” or aging without professional input.
- Contact an eye care provider: Schedule an appointment with an optometrist or ophthalmologist within 24–48 hours.
- Request a dilated fundus exam: This allows direct visualization of the retina and vitreous. It’s the gold standard for ruling out tears or detachment.
- Follow up as advised: Even if initial results are normal, return if symptoms persist or worsen.
FAQ: Common Questions About Flashes in the Dark
Can stress cause me to see flashes of light?
Stress alone does not directly create retinal flashes. However, high anxiety can heighten awareness of normal bodily sensations, including phosphenes. Stress may also trigger migraines in susceptible individuals, which can include visual aura resembling flashing lights. Managing stress through mindfulness or therapy may reduce such episodes.
Is it normal to see flashes when I close my eyes?
Occasional faint flickers or static-like patterns when closing your eyes in darkness are normal. These result from spontaneous retinal activity and are part of baseline neural noise. However, bright, structured, or directional flashes—especially if new or worsening—should be evaluated.
Do floaters always accompany dangerous flashes?
Most serious cases involving retinal traction or detachment involve both flashes and a sudden increase in floaters. Floaters occur when clumps form in the vitreous or when pigment is released from retinal damage. Their presence significantly raises concern and necessitates immediate examination.
Conclusion: Stay Informed, Stay Proactive
Seeing flashes of light in the dark isn’t inherently alarming, but it shouldn’t be ignored either. The distinction between harmless phosphenes and warning signs of retinal detachment hinges on timing, frequency, and accompanying symptoms. Knowledge empowers action—understanding what’s normal versus what demands urgency can preserve vision and prevent complications.
Regular eye checkups, especially after age 50 or with pre-existing risk factors, remain essential. Never hesitate to seek care when visual changes feel unusual. Your eyes communicate through subtle cues; learning to interpret them could protect your sight for years to come.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?