When you stand up from a seated or lying position, your body must quickly adjust to ensure blood continues flowing efficiently to the brain. For most people, this transition happens seamlessly. However, in some individuals, blood pressure drops significantly upon standing—a condition medically termed *orthostatic hypotension*. This sudden decline can lead to dizziness, lightheadedness, blurred vision, or even fainting. Understanding the physiological mechanisms behind this phenomenon, its contributing factors, and management strategies is essential for maintaining daily function and preventing falls, especially in older adults.
How the Body Regulates Blood Pressure During Position Changes
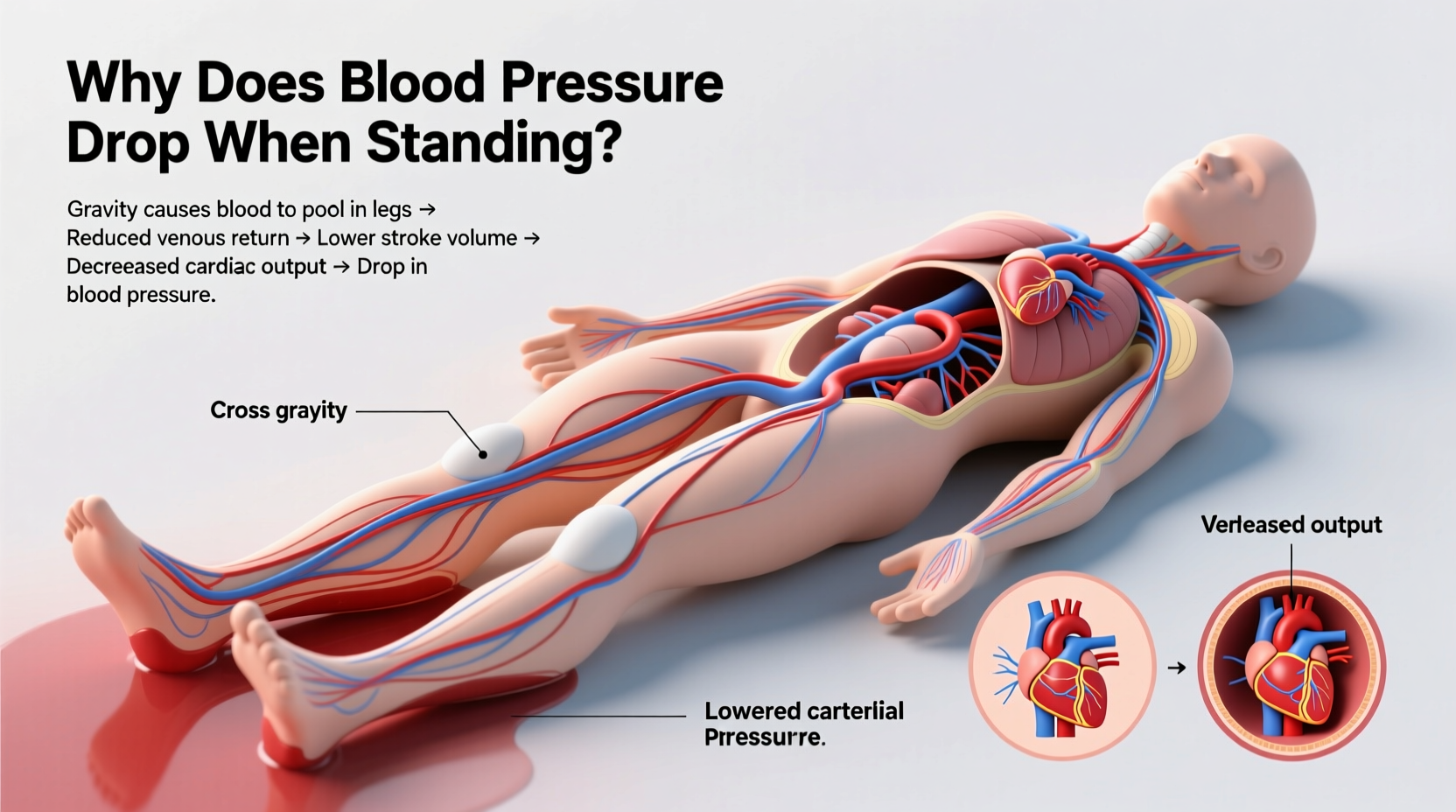
Gravity pulls blood downward when you stand. To counteract this, the autonomic nervous system initiates a rapid series of adjustments. Baroreceptors—specialized sensors located in the carotid arteries and aortic arch—detect the change in pressure and signal the brainstem. In response, the sympathetic nervous system increases heart rate and triggers vasoconstriction (narrowing of blood vessels), helping maintain adequate blood flow to the brain.
In individuals with orthostatic hypotension, this regulatory mechanism fails or responds too slowly. The result is reduced cerebral perfusion—meaning the brain receives less oxygenated blood—leading to transient symptoms. A drop of 20 mm Hg in systolic pressure or 10 mm Hg in diastolic pressure within three minutes of standing confirms the diagnosis.
Common Causes of Orthostatic Hypotension
Orthostatic hypotension is not a disease in itself but rather a sign of an underlying issue. It may stem from impaired autonomic regulation, volume depletion, or medication side effects. Common causes include:
- Dehydration: Reduced blood volume decreases venous return to the heart, limiting cardiac output upon standing.
- Medications: Diuretics, alpha-blockers, beta-blockers, antidepressants, and Parkinson’s drugs can interfere with vascular tone or heart rate control.
- Aging: Natural stiffening of blood vessels and slower autonomic responses increase susceptibility in older adults.
- Neurological disorders: Parkinson’s disease, multiple system atrophy, and diabetic neuropathy damage nerves involved in blood pressure regulation.
- Heart conditions: Bradycardia, heart failure, and arrhythmias impair the heart’s ability to compensate for postural changes.
- Prolonged bed rest: Immobility reduces circulatory efficiency and muscle pump activity in the legs.
“Orthostatic hypotension is more than just occasional dizziness—it’s a red flag that warrants clinical evaluation, particularly when recurrent.” — Dr. Lena Patel, Neurologist and Autonomic Specialist
Risk Factors and Vulnerable Populations
Certain groups face higher risks due to physiological or environmental factors. These include:
- Adults over 65: Age-related decline in baroreflex sensitivity and vascular compliance increases vulnerability.
- People with diabetes: Long-term hyperglycemia damages autonomic nerves, leading to neurogenic orthostatic hypotension.
- Those on antihypertensive therapy: Over-treatment of high blood pressure can push baseline levels too low, exacerbating drops when upright.
- Individuals with chronic illnesses: Conditions like adrenal insufficiency, anemia, or kidney disease contribute to poor volume status or impaired hormone regulation.
Even healthy individuals may experience temporary episodes after intense exercise, alcohol consumption, or large meals—especially those rich in carbohydrates—which divert blood to the digestive tract.
Step-by-Step Guide to Managing Symptoms
If you frequently feel lightheaded upon standing, implementing structured lifestyle adjustments can reduce symptom frequency and severity. Follow this practical sequence:
- Monitor symptoms: Keep a log of when dizziness occurs, including posture changes, time of day, and recent activities.
- Hydrate adequately: Aim for at least 1.5–2 liters of water daily unless contraindicated by heart or kidney conditions.
- Increase salt intake moderately: Under medical supervision, additional sodium helps retain fluid and boost blood volume.
- Perform counterpressure maneuvers: Cross your legs while standing or tense leg muscles to enhance venous return.
- Elevate the head of your bed: Sleeping with the upper body slightly raised reduces nighttime diuresis and morning drops.
- Review medications: Consult your physician about adjusting dosages or switching drugs that may contribute to hypotension.
- Engage in gradual physical conditioning: Regular aerobic and resistance training improve cardiovascular resilience.
Do’s and Don’ts: Daily Habits That Make a Difference
| Action | Do | Don’t |
|---|---|---|
| Standing Up | Rise slowly; pause sitting first | Jump up quickly from bed or chair |
| Hydration | Drink water throughout the day | Wait until thirsty to drink |
| Diet | Eat smaller, frequent meals | Consume large carbohydrate-heavy meals |
| Alcohol | Limits intake, especially in heat | Drink heavily, which dilates blood vessels |
| Compression | Wear abdominal binders or compression stockings | Ignore swelling or pooling in legs |
Real-Life Example: Managing Orthostatic Hypotension After Diagnosis
John, a 72-year-old retired teacher, began experiencing frequent dizziness when getting out of bed. One morning, he fainted while brushing his teeth, resulting in a minor concussion. His primary care doctor conducted a tilt-table test and confirmed orthostatic hypotension. John was taking amlodipine for hypertension and had reduced his fluid intake due to nocturia concerns.
His treatment plan included lowering his amlodipine dose, increasing daytime hydration, wearing waist-high compression stockings, and raising the head of his bed by six inches. Within three weeks, his symptoms improved dramatically. He now rises slowly each morning and reports no further episodes of syncope.
Frequently Asked Questions
Can orthostatic hypotension be reversed?
While some cases are chronic, especially those tied to neurological disease, many instances improve with proper hydration, medication adjustment, and lifestyle changes. Early intervention often prevents progression.
Is it dangerous to ignore occasional dizziness when standing?
Occasional mild lightheadedness may not be concerning, but frequent or severe symptoms increase fall risk and could indicate cardiovascular or neurological issues. Persistent symptoms should always be evaluated by a healthcare provider.
Are there tests to diagnose orthostatic hypotension?
Yes. The standard method involves measuring blood pressure and heart rate after five minutes of lying down, then again at one and three minutes after standing. Additional tests like the tilt-table test or autonomic reflex screen may be used if the cause is unclear.
Conclusion: Take Control of Your Circulatory Health
Orthostatic hypotension is more common than many realize, yet it often goes unreported or dismissed as normal aging. Recognizing the signs—dizziness, dimming vision, or near-fainting upon standing—is the first step toward effective management. By understanding the causes, adjusting daily habits, and working with healthcare providers to address underlying conditions, individuals can regain stability and confidence in their movements.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?