Stepping outside on a crisp winter morning should be refreshing—not painful. Yet for millions of people, a sharp, stabbing sensation shoots through their teeth at the first breath of cold air. This sudden discomfort isn’t just an annoyance; it’s a sign that something beneath the surface is off. Tooth sensitivity to cold air affects daily life, from jogging in the winter to sipping iced coffee on a summer day. Understanding the root causes, how enamel protection works, and what you can do to reduce or eliminate this pain is essential for long-term oral health.
The Science Behind Cold Air and Tooth Pain
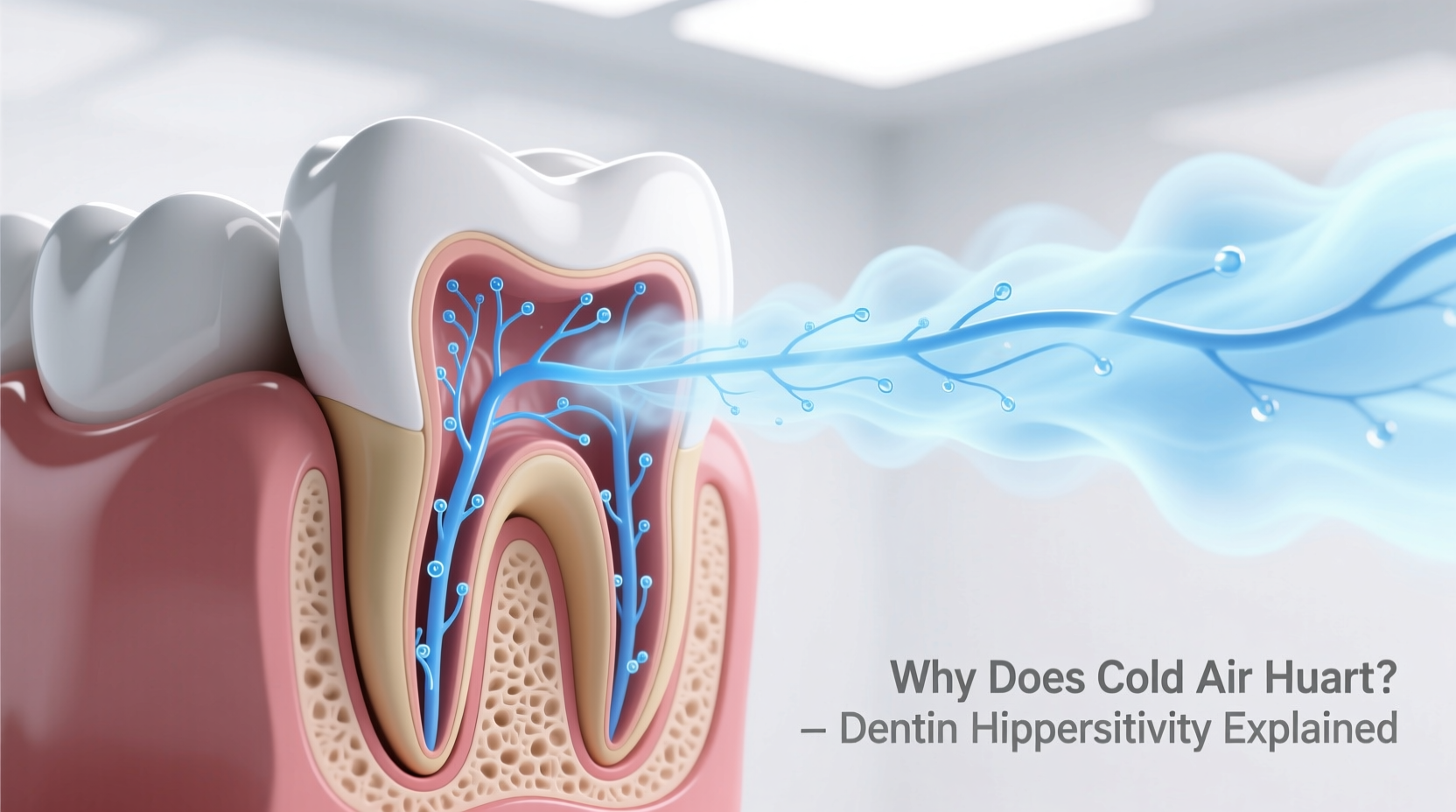
Tooth sensitivity occurs when the inner layer of the tooth, known as dentin, becomes exposed. Dentin lies beneath the hard outer enamel and contains thousands of microscopic tubules that lead directly to the nerve center of the tooth. When cold air hits these exposed pathways, it triggers rapid changes in fluid movement within the tubules, stimulating the nerves and causing a jolt of pain.
Unlike skin or muscle tissue, teeth don’t have pain receptors spread throughout—they respond acutely to temperature shifts, pressure, and chemical changes because the pulp (the innermost part) is densely innervated. Cold air, though not liquid like ice water, still conducts enough thermal energy to create a shock response when enamel is compromised.
This reaction is especially common during seasonal transitions, high-altitude activities, or even breathing through the mouth while exercising outdoors. The drier and colder the air, the more intense the sensation tends to be.
Common Causes of Exposed Dentin
Several factors contribute to the exposure of dentin, making teeth vulnerable to environmental triggers like cold air. These include:
- Enamel erosion: Caused by acidic foods, beverages (like citrus juice or soda), or acid reflux, which gradually wear down protective enamel.
- Gum recession: Often due to aggressive brushing, periodontal disease, or aging, leading to roots becoming exposed—roots lack enamel and are naturally sensitive.
- Tooth grinding (bruxism): Chronic grinding wears down enamel over time, particularly along the biting surfaces and near the gumline.
- Dental procedures: Recent whitening treatments, fillings, or professional cleanings can temporarily increase sensitivity.
- Cracked or chipped teeth: Even minor fractures can expose inner layers and trap bacteria, increasing sensitivity and risk of infection.
- Plaque buildup: Poor oral hygiene allows plaque to accumulate near the gumline, promoting decay and gum detachment.
It's important to note that occasional sensitivity doesn't always indicate serious damage. However, persistent or worsening pain should never be ignored—it may signal underlying issues requiring professional attention.
Who Is Most at Risk?
While anyone can experience cold-air-induced tooth pain, certain groups are more susceptible:
- People aged 20–50: This demographic reports the highest incidence of sensitivity, often linked to lifestyle habits such as diet, teeth whitening, and bruxism.
- Individuals with gum disease: Periodontitis leads to receding gums, exposing root surfaces directly to air and temperature changes.
- Frequent consumers of acidic foods: Regular intake of wine, tomatoes, pickles, or carbonated drinks accelerates enamel demineralization.
- Mouth breathers: Whether due to nasal congestion or sleep apnea, breathing through the mouth increases direct exposure of teeth to cold, dry air.
- Athletes and outdoor enthusiasts: Runners, cyclists, and skiers often inhale large volumes of cold air rapidly, heightening sensitivity episodes.
“Cold-induced tooth pain is one of the most underreported dental concerns. Patients often dismiss it until it interferes with eating or speaking. Early intervention prevents progression.” — Dr. Lena Torres, Clinical Dentist and Oral Health Researcher
Prevention and Management Strategies
Managing sensitivity to cold air involves both immediate relief techniques and long-term preventive care. The goal is to either block the transmission of pain signals or strengthen the tooth’s natural defenses.
Step-by-Step Guide to Reducing Sensitivity
- Switch to a desensitizing toothpaste: Use products containing potassium nitrate or stannous fluoride, which help block nerve signaling and reinforce weakened enamel. Apply with a soft-bristled brush twice daily.
- Improve brushing technique: Use gentle circular motions instead of harsh horizontal scrubbing. Focus on angling the brush 45 degrees toward the gumline to avoid further recession. <
- Rinse after acidic meals: Wait 30 minutes after consuming acidic foods before brushing. In the meantime, rinse with water or a neutral pH mouthwash to minimize erosion.
- Wear a night guard if you grind: Custom-fitted guards protect enamel from nocturnal wear and reduce stress on teeth.
- Stay hydrated: Dry mouth reduces saliva’s buffering effect, allowing acids to linger longer on teeth. Drink water regularly, especially in heated indoor environments during winter.
- Use a fluoride mouth rinse: Daily use strengthens enamel and reduces permeability of dentinal tubules.
- Visit your dentist every six months: Professional cleanings remove tartar below the gumline and allow early detection of cracks or decay.
| Cause | Symptom Pattern | Recommended Action |
|---|---|---|
| Enamel erosion | Pain when consuming cold, hot, or sweet items | Limit acidic foods; use fluoride treatments |
| Gum recession | Visible root exposure; sensitivity near gumline | Gentle brushing; possible gum graft consultation |
| Tooth grinding | Generalized sensitivity; worn flat surfaces | Night guard; stress management |
| Recent dental work | Temporary sensitivity lasting 1–4 weeks | Desensitizing toothpaste; avoid extreme temps |
| Cracked tooth | Sharp pain when biting or exposed to air | Immediate dental evaluation |
When to See a Dentist
Not all sensitivity resolves with home care. Persistent or escalating pain requires clinical assessment. Warning signs include:
- Pain lasting more than 30 seconds after stimulus removal
- Spontaneous pain without any trigger
- Swelling, bleeding gums, or visible cracks
- Increased sensitivity following a dental procedure beyond four weeks
Treatment options vary based on diagnosis. Your dentist may apply bonding agents to cover exposed roots, recommend root canal therapy if nerve damage is suspected, or prescribe high-concentration fluoride gels for home use. In cases of severe gum recession, surgical interventions like gum grafting can restore protective tissue.
Mini Case Study: Recovering from Winter Sensitivity
Sarah, a 34-year-old runner from Minnesota, began experiencing sharp tooth pain every time she jogged in temperatures below freezing. Initially dismissing it as \"just the cold,\" she eventually avoided outdoor exercise altogether. After visiting her dentist, she was diagnosed with moderate gum recession caused by years of overzealous brushing. She also admitted to frequent consumption of lemon water—a known enamel eroder.
Her treatment plan included switching to a soft electric toothbrush, using a prescription-strength desensitizing toothpaste, and wearing a custom-fitted mouthguard during runs. Within six weeks, her symptoms decreased significantly. A follow-up fluoride varnish application provided additional protection. Today, Sarah runs year-round without discomfort, attributing her recovery to early professional intervention and consistent self-care.
FAQ
Can cold air permanently damage my teeth?
No, cold air itself does not cause permanent damage. However, repeated exposure can worsen existing conditions like enamel loss or gum recession, especially if combined with poor oral hygiene or dietary habits.
Is tooth sensitivity a sign of cavities?
It can be. Cavities near the gumline or between teeth often present as sensitivity to temperature before progressing to constant pain. Only an X-ray and clinical exam can confirm decay.
Are electric toothbrushes better for sensitive teeth?
Yes, many electric brushes have pressure sensors and oscillating heads that promote gentler cleaning. Just ensure you’re using a soft brush head and not applying excessive force.
Conclusion: Take Control of Your Comfort
Cold air shouldn’t dictate when or where you go. Tooth sensitivity is not something you must endure—it’s a signal from your body asking for attention. By understanding the mechanisms behind the pain and taking proactive steps, you can reclaim comfort in everyday activities. From adjusting your brushing habits to seeking timely dental care, each action builds a stronger defense against sensitivity.
Start today: examine your routine, identify potential risks, and implement at least one change from this guide. Your teeth are built to last a lifetime—treat them with the care they deserve.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?