Itching—medically known as pruritus—is a sensation that triggers the urge to scratch. While it’s a normal bodily response to minor irritants, persistent or severe itching can signal underlying health issues. It affects people of all ages and can arise from simple dry skin to complex neurological conditions. Understanding why itching occurs, what factors contribute to it, and how to effectively manage it is essential for both comfort and long-term skin health.
The Science Behind the Itch
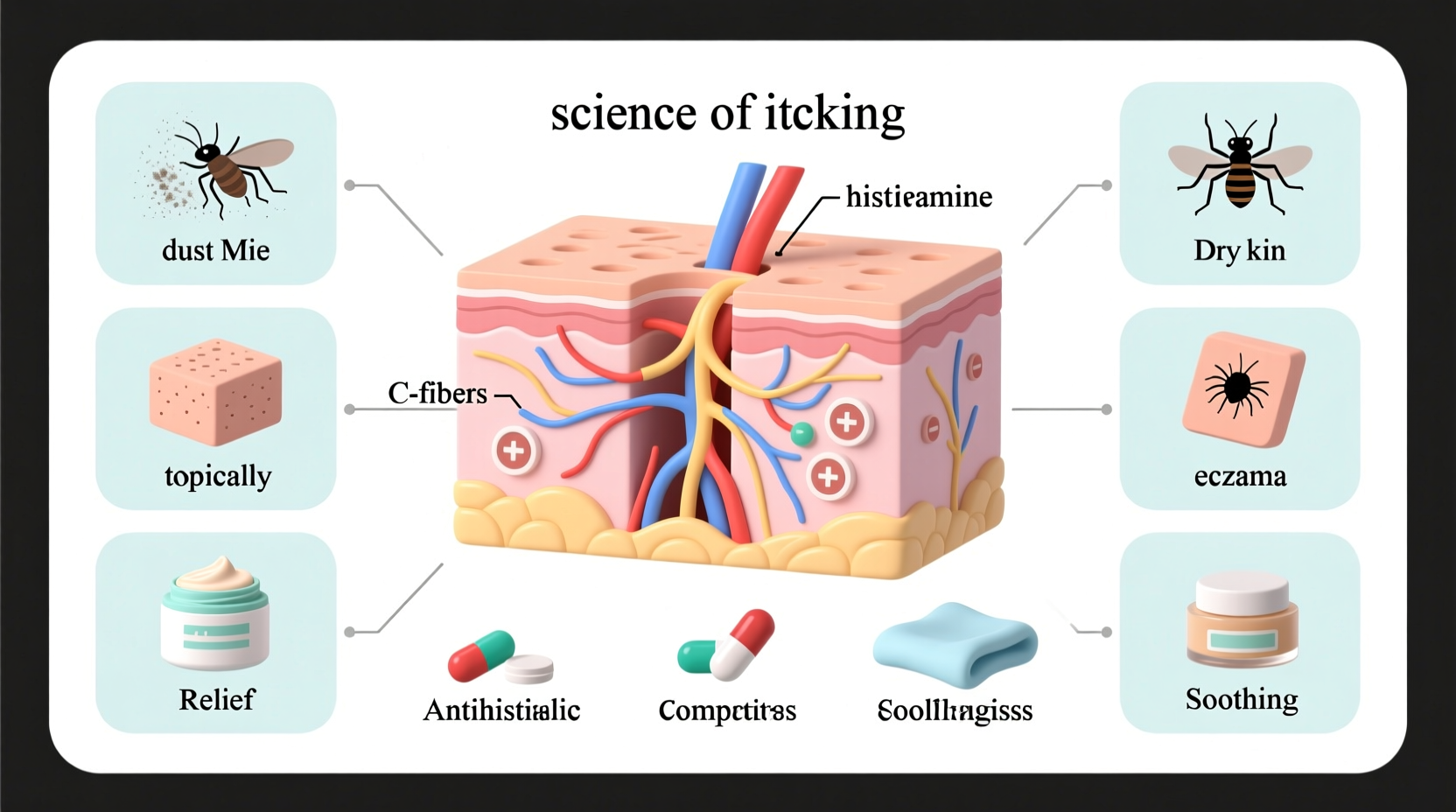
Itching begins in the skin, where specialized nerve fibers detect potential threats such as allergens, insect bites, or chemical irritants. These nerves send signals through the spinal cord to the brain, which interprets them as an itch. Unlike pain, which prompts withdrawal, itching encourages scratching—a reflex meant to remove parasites or irritants from the skin surface.
However, chronic scratching can damage the skin barrier, leading to inflammation, infection, and a vicious cycle of more itching. Histamine, a chemical released by immune cells during allergic reactions, is one of the most well-known mediators of itch. But other substances like serotonin, proteases, and cytokines also play critical roles, especially in non-allergic forms of pruritus.
“Chronic itching isn’t just a nuisance—it can significantly impair quality of life, affecting sleep, mental health, and daily functioning.” — Dr. Linda Chen, Dermatology Specialist, Johns Hopkins Medicine
Common Causes of Itching
Itching can stem from a wide range of sources, broadly categorized into skin-related (dermatological) and systemic (internal) causes.
Skin-Related Causes
- Dry skin (xerosis): Especially common in winter or low-humidity environments, dry skin lacks natural oils, leading to flaking and irritation.
- Eczema (atopic dermatitis): A chronic condition causing red, inflamed, and intensely itchy patches, often appearing in folds of elbows and knees.
- Psoriasis: An autoimmune disorder resulting in thick, scaly plaques that may be itchy or sore.
- Insect bites and stings: Mosquitoes, bed bugs, and fleas inject saliva that triggers localized histamine release and itching.
- Contact dermatitis: Caused by exposure to irritants (like detergents) or allergens (such as nickel or poison ivy).
Systemic & Internal Causes
- Liver disease: Conditions like cholestasis impair bile flow, leading to toxin buildup that causes widespread itching, particularly on palms and soles.
- Kidney failure: Accumulation of waste products in uremic patients often results in generalized pruritus.
- Thyroid disorders: Both hyperthyroidism and hypothyroidism can disrupt skin moisture and cause itching.
- Diabetes: Poor circulation and nerve damage (neuropathy) contribute to dry, itchy skin, especially on the lower legs.
- Medications: Opioids, certain antibiotics, and antihypertensives are known to induce itching as a side effect.
- Pregnancy: Some women develop pruritic urticarial papules and plaques of pregnancy (PUPPP) or intrahepatic cholestasis, which causes intense itching without rash.
Effective Relief Strategies
Managing itching depends on identifying and addressing its root cause. However, several general strategies can provide immediate relief while longer-term treatments take effect.
Topical Treatments
- Moisturizers: Use fragrance-free creams containing ceramides, glycerin, or hyaluronic acid immediately after bathing to lock in moisture.
- Cool compresses: Apply a damp cloth to itchy areas for 5–10 minutes to soothe irritated skin.
- Over-the-counter hydrocortisone cream (1%): Reduces inflammation and itching due to eczema or allergic reactions. Limit use to short durations (up to 7 days).
- Calamine lotion or colloidal oatmeal baths: Provide cooling relief for rashes, chickenpox, or poison ivy.
Oral Medications
- Antihistamines: First-generation options like diphenhydramine (Benadryl) are effective for nighttime relief due to their sedative effects. Second-gen drugs like loratadine (Claritin) offer daytime control without drowsiness.
- Prescription therapies: For severe cases, doctors may prescribe stronger corticosteroids, immunosuppressants (e.g., cyclosporine), or newer biologics like dupilumab for atopic dermatitis.
| Itch Type | Recommended Treatment | Avoid |
|---|---|---|
| Dry skin | Fragrance-free moisturizer, humidifier | Hot showers, harsh soaps |
| Eczema | Topical steroids, wet wrap therapy | Scratching, wool clothing |
| Allergic reaction | Oral antihistamines, cold compress | Known allergens, tight fabrics |
| Internal disease-related | Treat underlying condition (e.g., dialysis, liver meds) | Self-medicating with steroids |
Step-by-Step Guide to Managing Daily Itch Triggers
For those dealing with recurring itching, adopting a structured routine can dramatically reduce flare-ups:
- Identify triggers: Keep a symptom diary noting when and where itching occurs, along with diet, activities, and products used.
- Shower wisely: Use lukewarm water and limit showers to 10 minutes. Avoid scrubbing with loofahs or harsh washcloths.
- Choose gentle cleansers: Opt for soap-free, pH-balanced body washes labeled “for sensitive skin.”
- Moisturize within 3 minutes of bathing: Apply ointment or cream while skin is still damp to seal in hydration.
- Wear soft, breathable fabrics: Cotton and bamboo are less likely to irritate than synthetic or wool materials.
- Control your environment: Use a humidifier in dry seasons and avoid overheating rooms, which dries the air.
- Trim nails and wear gloves at night: Prevents unconscious scratching during sleep.
Real-Life Example: Managing Eczema in Children
Six-year-old Maya had suffered from eczema since infancy. Her parents noticed worsening itching during winter months, especially at night. After multiple steroid creams provided only temporary relief, they consulted a pediatric dermatologist. The doctor recommended a comprehensive plan: switching to fragrance-free laundry detergent, using a humidifier in her bedroom, applying petroleum jelly twice daily, and giving a nightly dose of non-drowsy antihistamine. Within three weeks, Maya’s flare-ups decreased significantly, and her sleep improved. This case highlights how combining environmental adjustments with consistent skincare can break the itch-scratch cycle.
When to See a Doctor
While many cases of itching resolve with home care, certain symptoms warrant medical evaluation:
- Itching all over the body with no rash
- Nighttime itching that disrupts sleep
- Signs of infection (pus, warmth, swelling)
- Associated symptoms like fatigue, weight loss, or jaundice
- Persistent itching lasting more than four weeks
A physician may order blood tests, liver function panels, or skin biopsies to determine if an internal condition is responsible.
Frequently Asked Questions
Can stress cause itching?
Yes. Emotional stress activates the nervous system and can trigger or worsen itching, especially in conditions like eczema or psoriasis. Stress reduction techniques such as mindfulness, yoga, or cognitive behavioral therapy may help reduce flare-ups.
Is it safe to use antihistamines every day?
Second-generation antihistamines (like cetirizine or fexofenadine) are generally safe for daily use under medical supervision. However, long-term reliance without diagnosing the underlying cause is not recommended.
Why do I itch more at night?
Nighttime itching increases due to natural circadian rhythms—body temperature rises, cortisol (an anti-inflammatory hormone) drops, and distractions decrease, making sensations more noticeable. Bedding allergens or nocturnal pests like mites may also contribute.
Conclusion: Take Control of Your Comfort
Itching is more than a passing annoyance—it’s a signal from your body that something needs attention. Whether it's adjusting your skincare routine, identifying allergens, or seeking treatment for an underlying illness, proactive steps make a significant difference. By understanding the causes and applying targeted relief strategies, you can restore comfort and protect your skin’s health. Don’t ignore persistent itch; address it early, treat it wisely, and reclaim your peace of mind.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?