Waking up with a numb arm is more than just an inconvenience—it can disrupt sleep, cause discomfort, and raise concerns about long-term nerve health. While occasional tingling might seem harmless, recurring numbness during sleep often signals underlying postural, neurological, or musculoskeletal issues. Understanding the root causes and applying targeted solutions can prevent chronic discomfort and support better overall nerve function.
The sensation of a \"dead arm\" typically stems from compression of nerves or reduced blood flow, most commonly in the brachial plexus—a network of nerves running from the neck through the shoulder and down the arm. This article explores the most frequent reasons behind nighttime arm numbness, outlines evidence-based stretches to alleviate symptoms, and provides practical strategies for preventing recurrence.
Common Causes of Arm Numbness During Sleep
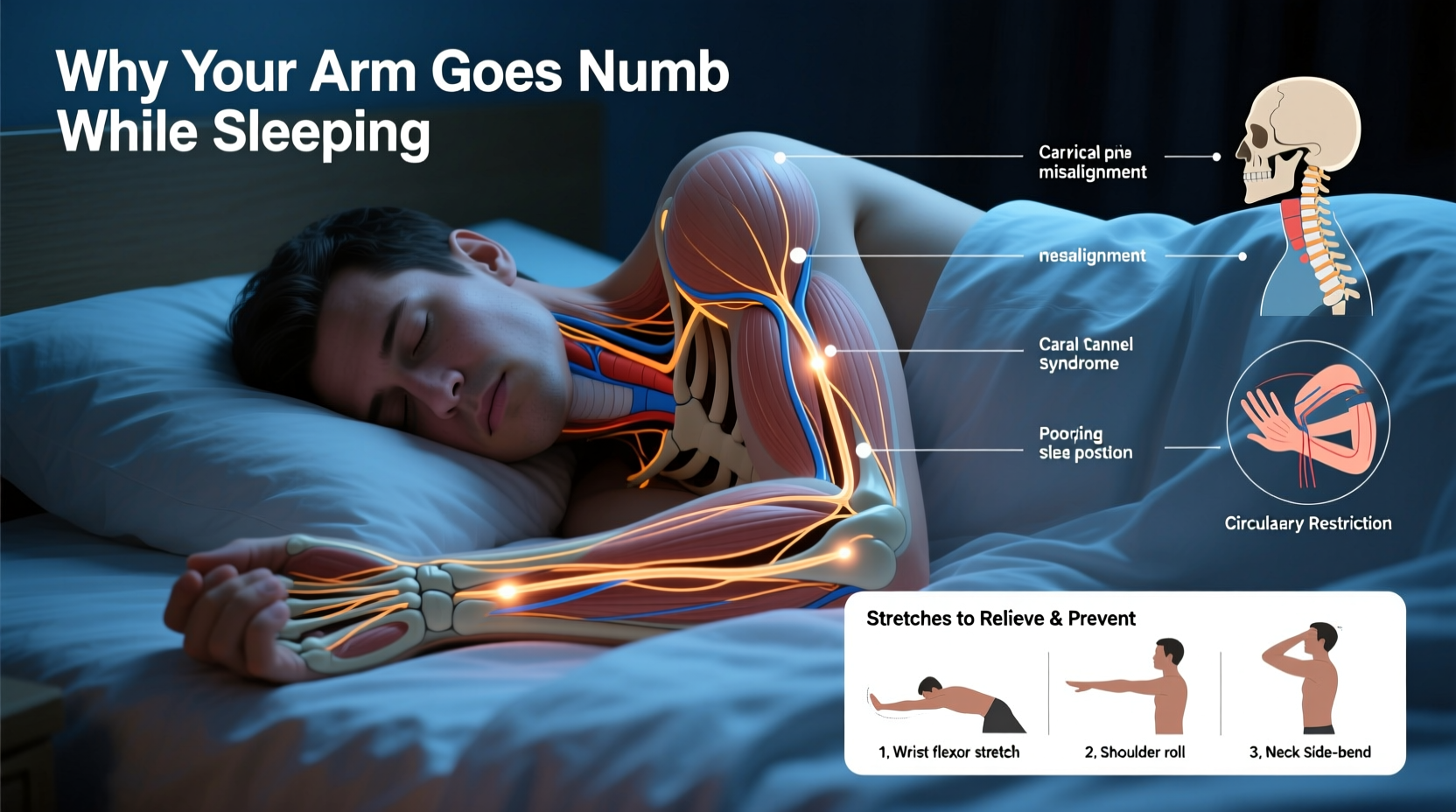
Numbness in the arm while sleeping usually results from sustained pressure on nerves or blood vessels. The position you sleep in plays a major role, but underlying medical conditions can also contribute. Below are the primary causes:
- Improper Sleeping Position: Lying on one arm or tucking it under your head or body compresses nerves and restricts circulation. Side sleepers are especially prone if they don’t use proper pillow support.
- Cervical Radiculopathy: A pinched nerve in the neck—often due to herniated discs, arthritis, or spinal stenosis—can radiate tingling or numbness into the arm, particularly during rest when certain positions exacerbate pressure.
- Thoracic Outlet Syndrome (TOS): This condition occurs when nerves or blood vessels between the collarbone and first rib are compressed. Symptoms often worsen at night due to shoulder elevation or arm positioning.
- Diabetes or Peripheral Neuropathy: Elevated blood sugar levels can damage peripheral nerves over time, leading to chronic numbness that may feel worse at night due to reduced external stimuli.
- Vitamin Deficiencies: Low levels of B vitamins—especially B12, B6, and B1—are linked to nerve dysfunction and sensory disturbances, including nighttime tingling.
- Poor Circulation: Conditions like Raynaud’s phenomenon or cardiovascular issues may reduce blood flow to extremities, contributing to coldness and numbness upon waking.
How Posture Influences Nerve Compression
Your spine and shoulder alignment directly affect nerve pathways. When the cervical spine (neck) is misaligned or strained, even slight changes in posture during sleep can trigger nerve impingement. For example, side sleepers who allow their top shoulder to roll forward may compress the brachial plexus against the chest wall.
Similarly, stomach sleepers often turn their head sharply to one side, stretching and irritating cervical nerve roots. Over time, poor spinal curvature or muscle imbalances in the neck and shoulders can make nerve compression more likely—even without extreme positions.
A study published in *The Spine Journal* found that individuals with forward head posture were 2.3 times more likely to report upper limb numbness during sleep compared to those with neutral alignment. Strengthening postural muscles and adjusting sleep ergonomics can significantly reduce this risk.
“Nighttime arm numbness is rarely random. It’s usually a sign of mechanical stress on neural structures that accumulates over hours of immobility.” — Dr. Alan Reyes, Neurologist and Sleep Medicine Specialist
Effective Stretches to Relieve Nerve Pressure
Regular stretching improves flexibility, reduces muscle tension around nerves, and enhances circulation. These five stretches target key areas involved in arm numbness: the neck, shoulders, and upper back. Perform them daily, especially before bed, to minimize compression risks.
1. Neck Side Bend Stretch
This stretch relieves tension in the scalene muscles, which can compress nerves in thoracic outlet syndrome.
- Sit upright with shoulders relaxed.
- Gently tilt your head to the right, bringing your ear toward your shoulder.
- Hold for 20–30 seconds, then switch sides.
- Repeat 2–3 times per side.
2. Shoulder Rolls and Shrugs
Loosens tight trapezius and levator scapulae muscles that contribute to nerve impingement.
- Roll shoulders backward in slow circles for 30 seconds.
- Shrug shoulders up toward ears, hold for 3 seconds, then release.
- Repeat 10 times.
3. Pectoral Doorway Stretch
Opens the front of the chest and counteracts rounded shoulders, reducing pressure on the brachial plexus.
- Stand in a doorway with elbows bent at 90 degrees and forearms on the frame.
- Step forward gently until you feel a stretch across your chest.
- Hold for 30 seconds; repeat 2–3 times.
4. Chin Tucks (Neck Retraction)
Strengthens deep neck flexors and corrects forward head posture.
- Lie on your back or sit upright.
- Gently tuck your chin as if making a “double chin.”
- Hold for 5 seconds, then release.
- Perform 10 repetitions.
5. Upper Trapezius Stretch
Targets the upper shoulder muscles that often refer pain and numbness down the arm.
- Sit with good posture.
- Place your right hand behind your back.
- Use your left hand to gently pull your head to the left.
- Hold for 20–30 seconds, then switch sides.
Prevention Checklist: Reduce Nighttime Arm Numbness
Addressing root causes requires consistent habits. Use this checklist nightly to protect nerve health and improve sleep quality.
- ✅ Choose a supportive pillow that keeps your neck aligned with your spine.
- ✅ Avoid sleeping on your stomach or with arms raised above your head.
- ✅ Use a medium-firm mattress that supports spinal alignment.
- ✅ Perform evening stretches targeting neck, shoulders, and chest.
- ✅ Limit screen time before bed to reduce forward head posture buildup.
- ✅ Stay hydrated—dehydration can increase nerve sensitivity.
- ✅ Review medications with your doctor; some drugs may contribute to neuropathy.
- ✅ Manage blood sugar levels if diabetic or prediabetic.
When to See a Doctor
While many cases resolve with lifestyle adjustments, persistent or worsening symptoms warrant medical evaluation. Seek professional care if you experience any of the following:
| Symptom | Possible Implication | Action Step |
|---|---|---|
| Numbness lasting more than 30 minutes after waking | Chronic nerve compression or structural issue | Consult neurologist or orthopedic specialist |
| Weakening grip strength or muscle atrophy | Advanced cervical radiculopathy or neuropathy | Request EMG or MRI imaging |
| Numbness spreading to both arms | Cervical spine degeneration or systemic condition | Evaluate for spinal cord involvement |
| Burning pain, especially at night | Peripheral neuropathy or diabetes complication | Check HbA1c and vitamin B12 levels |
Early diagnosis of conditions like cervical disc disease or thoracic outlet syndrome can prevent irreversible nerve damage. Don’t dismiss recurring symptoms as “just sleeping wrong”—they may be early warning signs.
Real-Life Example: Recovering from Chronic Numbness
Mark, a 42-year-old software developer, began waking up several times a week with a completely numb left arm. Initially, he dismissed it as awkward sleeping, but after three months of increasing frequency—and noticeable weakness in his hand grip—he consulted a physical therapist.
Assessment revealed tight pectoral muscles, forward head posture, and mild C6-C7 disc bulging on MRI. His habit of sleeping on his left side with his arm tucked under the pillow was aggravating the pinched nerve.
Following a six-week protocol of daily stretches, ergonomic desk adjustments, and switching to a contoured cervical pillow, Mark reported complete resolution of nighttime numbness. Follow-up testing showed improved nerve conduction velocity, confirming functional recovery.
His case underscores how combining self-care with professional guidance can reverse symptoms without surgery or medication.
Frequently Asked Questions
Can stress cause arm numbness at night?
Yes. Chronic stress leads to muscle tension, particularly in the neck and shoulders, which can compress nerves. Additionally, stress-related shallow breathing and poor sleep posture amplify the risk. Managing stress through mindfulness, breathing exercises, and regular movement can reduce these effects.
Is arm numbness during pregnancy normal?
Some women experience arm numbness during pregnancy due to fluid retention increasing pressure on nerves, especially in the third trimester. Carpal tunnel syndrome is common, but brachial plexus irritation can also occur. Using supportive pillows and performing gentle stretches often helps. Always consult your OB-GYN if symptoms are severe or asymmetric.
Why does only one arm go numb?
Unilateral numbness usually points to localized nerve compression related to sleep position or asymmetrical muscle imbalances. For example, consistently favoring one side while sleeping can irritate nerves on that side. However, if new or accompanied by dizziness, speech changes, or facial drooping, seek emergency care—these could indicate a stroke.
Conclusion: Take Control of Your Sleep and Nerve Health
Arm numbness during sleep isn’t something to simply endure. It’s a signal from your body that pressure, posture, or underlying health factors need attention. By identifying the cause—whether it’s a poor pillow, nerve compression, or a metabolic condition—you can take meaningful steps toward relief.
Incorporate targeted stretches into your nightly routine, optimize your sleep environment, and listen to your body’s cues. Small, consistent changes today can prevent chronic discomfort tomorrow. If symptoms persist, don’t hesitate to seek medical insight—early intervention protects long-term mobility and nerve function.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?