Lower back pain during menstruation is a common experience for many people who menstruate. While cramps in the abdomen are widely recognized, back pain often receives less attention—despite affecting up to 70% of individuals during their cycle. This discomfort can range from a dull, persistent ache to sharp, radiating pain that interferes with daily activities. Understanding the underlying causes and learning practical strategies for relief can make a significant difference in managing this monthly challenge.
The Science Behind Menstrual Back Pain
Menstrual-related back pain is primarily linked to hormonal fluctuations and uterine contractions. During your period, the body releases prostaglandins—hormone-like compounds that trigger the uterus to contract and shed its lining. High levels of prostaglandins can cause intense contractions, not only in the uterus but also in surrounding muscles, including those in the lower back and pelvis.
These contractions may compress nearby nerves, particularly the sciatic nerve or sacral plexus, leading to referred pain in the lower back, hips, and even down the legs. Additionally, the position of the uterus can influence pain patterns. A tilted or retroverted uterus may place added pressure on the lower spine, increasing the likelihood of back discomfort.
“Prostaglandins play a central role in menstrual pain. Higher levels correlate with more severe cramping and associated symptoms like backache.” — Dr. Lena Patel, Gynecologist and Hormonal Health Specialist
Common Causes of Period-Related Back Pain
- Hormonal shifts: Estrogen and progesterone drop sharply before menstruation, which can increase inflammation and muscle sensitivity.
- Uterine contractions: Strong contractions can radiate pain to the back via shared nerve pathways.
- Endometriosis: A condition where endometrial tissue grows outside the uterus, potentially causing chronic back pain, especially during periods.
- Adenomyosis: When endometrial tissue invades the uterine muscle wall, it can lead to heavy bleeding and deep pelvic/back pain.
- Poor posture and muscle tension: Hormonal changes can affect ligament laxity and core stability, making the back more vulnerable to strain.
- Stress and fatigue: Elevated cortisol during your period can amplify pain perception and reduce pain tolerance.
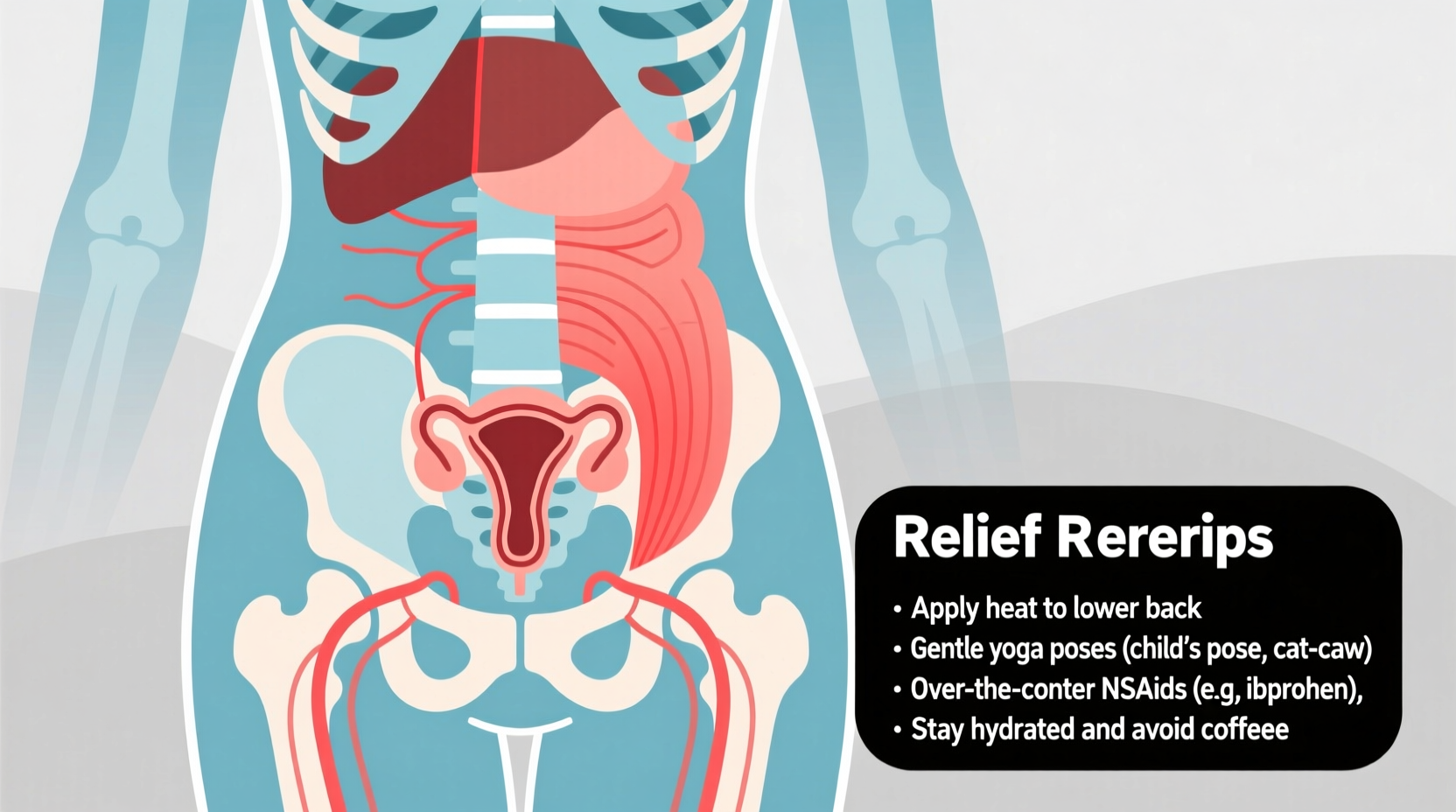
Effective Relief Strategies
While some level of discomfort may be expected, debilitating back pain isn’t something you have to accept as inevitable. A combination of lifestyle adjustments, physical techniques, and medical support can provide meaningful relief.
1. Heat Therapy
Applying heat to the lower back increases blood flow, relaxes tight muscles, and reduces muscle spasms. Use a heating pad, hot water bottle, or take a warm bath for 15–20 minutes at a time.
2. Gentle Exercise and Stretching
Movement helps release endorphins—natural painkillers—and prevents stiffness. Focus on low-impact activities such as walking, swimming, or yoga. Specific stretches like child’s pose, cat-cow, and seated forward bends can alleviate tension in the lower back and pelvis.
3. Over-the-Counter Pain Relief
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen reduce prostaglandin production, directly targeting the source of menstrual pain. For best results, start taking them at the first sign of pain or just before your period begins.
4. Hydration and Anti-Inflammatory Diet
Dehydration can worsen muscle cramps. Drink plenty of water and limit intake of inflammatory foods such as processed sugars, caffeine, and trans fats. Increase consumption of omega-3 fatty acids (found in salmon, flaxseeds, and walnuts), magnesium-rich foods (like spinach and almonds), and antioxidant-packed fruits and vegetables.
5. Posture and Ergonomic Support
Sitting for long periods, especially with poor posture, can exacerbate back pain. Use lumbar support when sitting, avoid slouching, and take frequent breaks to stand and stretch.
“Many patients report dramatic improvement simply by correcting their sitting posture and adding daily stretching. It’s not always about medication.” — Dr. Alan Zhou, Physical Therapist
When to Seek Medical Advice
Occasional back pain during your period is normal, but certain red flags warrant evaluation by a healthcare provider:
- Pain that disrupts daily life or requires strong painkillers regularly
- Back pain occurring outside of your period
- Pain accompanied by irregular bleeding, painful intercourse, or digestive issues
- Gradual worsening of symptoms over time
These could indicate conditions like endometriosis, fibroids, pelvic inflammatory disease, or musculoskeletal disorders. Diagnostic tools such as pelvic ultrasounds, MRI scans, or laparoscopy may be recommended for further investigation.
Step-by-Step Guide to Managing Period Back Pain
- Day Before Your Period Starts: Begin taking magnesium supplements (200–400 mg) and stay hydrated. Light stretching or yoga can prep your body.
- First Day of Period: Start NSAIDs if needed. Apply heat to lower back. Avoid caffeine and alcohol.
- Mid-Period (Days 2–3): Continue gentle movement. Use a supportive seat cushion if working from home or commuting.
- As Bleeding Tapers Off: Gradually resume regular activity. Incorporate strength training for core and back muscles to improve long-term resilience.
- Post-Period: Reflect on what worked. Adjust your approach next cycle. Consider seeing a pelvic floor therapist if pain persists.
Do’s and Don’ts: Quick Reference Table
| Do’s | Don’ts |
|---|---|
| Use heat therapy on the lower back | Apply ice unless advised by a doctor (heat is usually better for menstrual pain) |
| Stay moderately active with walking or stretching | Remain sedentary all day |
| Take NSAIDs early in the cycle | Wait until pain becomes severe to medicate |
| Eat anti-inflammatory foods (leafy greens, berries, nuts) | Consume excess salt, sugar, or processed foods |
| Practice relaxation techniques (deep breathing, meditation) | Ignore signs of chronic or worsening pain |
Real-Life Example: Sarah’s Journey with Period Back Pain
Sarah, a 29-year-old teacher, experienced severe lower back pain every month that left her bedridden for the first two days of her period. She assumed it was normal until she missed a school event due to pain. After consulting a gynecologist, she was diagnosed with mild endometriosis. Her treatment plan included starting ibuprofen earlier in her cycle, using a heating pad daily, and attending weekly pelvic floor physical therapy. Within three months, her pain decreased by over 60%. She now manages her symptoms proactively and educates others about the importance of seeking help early.
Frequently Asked Questions
Can birth control help with period-related back pain?
Yes. Hormonal contraceptives like the pill, patch, or IUD can regulate or suppress ovulation and reduce prostaglandin production, often decreasing both cramping and back pain. Consult your doctor to determine the best option for your health profile.
Is it normal for back pain to get worse with age?
Not necessarily. While some women find symptoms improve after childbirth or with lifestyle changes, others may experience worsening pain due to conditions like fibroids or adenomyosis, which are more common in the 30s and 40s. Tracking symptoms helps distinguish normal variation from concerning trends.
Can stress really make my period back pain worse?
Absolutely. Stress activates the sympathetic nervous system, increasing muscle tension and lowering pain thresholds. Chronic stress can also disrupt hormonal balance, potentially intensifying menstrual symptoms. Mindfulness, adequate sleep, and breathing exercises can help mitigate these effects.
Take Control of Your Comfort
Menstrual back pain doesn’t have to dictate your monthly rhythm. By understanding the physiological causes and applying targeted relief strategies, you can significantly reduce discomfort and regain control. Whether it’s adjusting your diet, incorporating mindful movement, or seeking medical guidance when needed, small consistent actions lead to lasting change. Listen to your body, advocate for your health, and remember—you’re not alone in this experience.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?