Itching on the back that worsens at night is a surprisingly common complaint, yet one that many people hesitate to discuss. Unlike daytime discomfort, nighttime itching can disrupt sleep, increase stress, and create a cycle of irritation that feels impossible to break. While occasional itching is normal, persistent or severe back itchiness during sleep may point to underlying causes ranging from environmental factors to systemic health conditions. Understanding the root triggers is the first step toward effective relief.
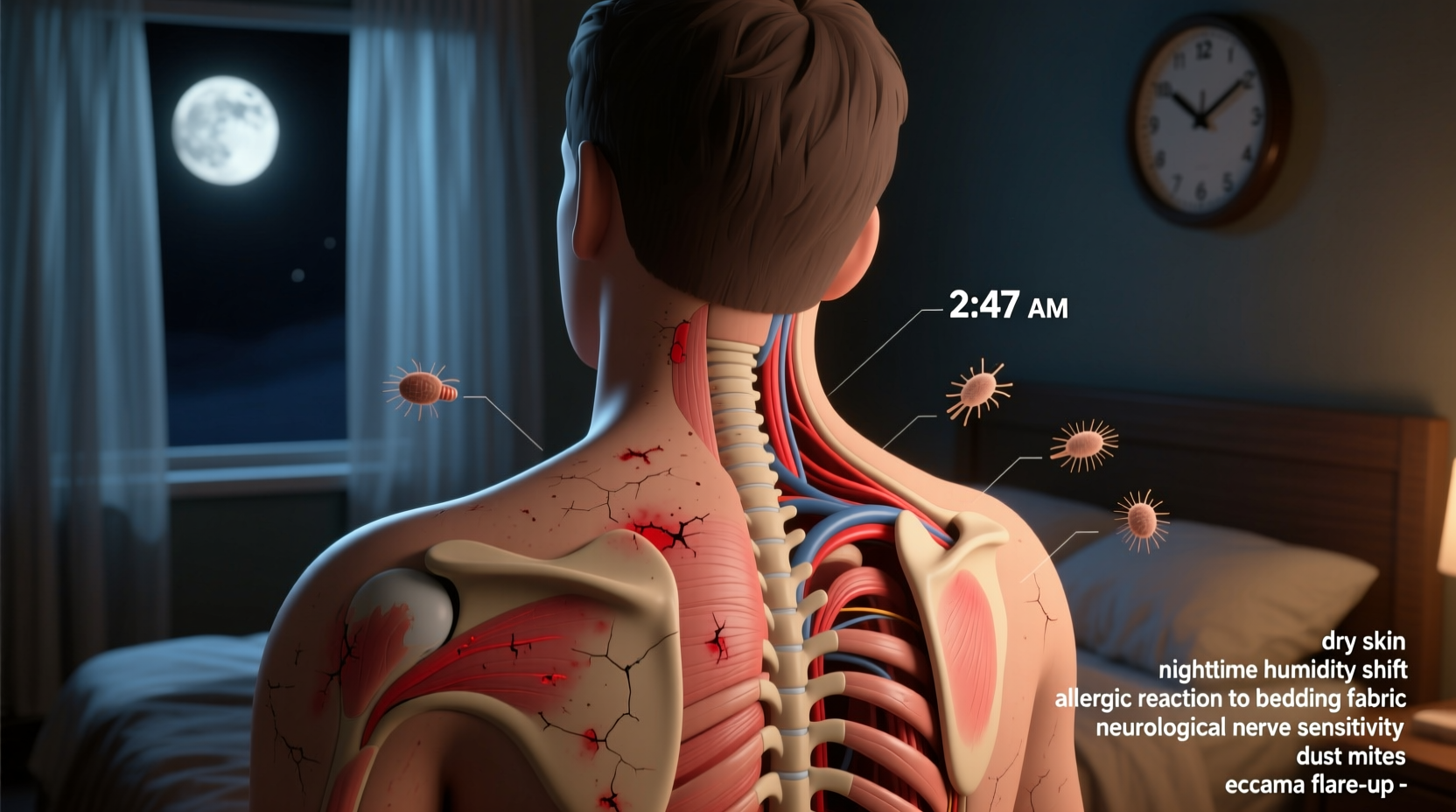
The human body undergoes numerous physiological changes at night—skin temperature rises, cortisol levels drop, and nerve signals become more pronounced. These shifts can amplify sensations like itchiness, particularly in areas like the back that are difficult to monitor or scratch without waking. This article explores the most likely causes of nocturnal back itching, backed by medical insight and real-world patterns, and offers actionable strategies to restore restful nights.
Common Environmental Triggers
Your sleeping environment plays a crucial role in skin comfort. The materials you lie against, the air quality in your bedroom, and even laundry habits can contribute to nighttime itching.
- Detergent residue: Harsh chemicals or fragrances left in bed linens after washing can irritate sensitive skin, especially if not rinsed thoroughly.
- Bedding materials: Synthetic fabrics like polyester trap heat and moisture, creating an ideal environment for irritation and micro-sweating that triggers itch receptors.
- Dust mites and allergens: Mattresses and pillows accumulate dust mites over time. Their droppings are a known allergen and can cause localized itching, particularly on the back where contact is prolonged.
- Dry indoor air: Especially in winter, heated rooms reduce humidity, leading to dry skin (xerosis), which often manifests as intense itching at night.
Skin Conditions That Worsen at Night
Certain dermatological conditions exhibit a circadian pattern, meaning symptoms intensify during the evening and night due to hormonal and neurological fluctuations.
Eczema (Atopic Dermatitis): A chronic condition causing dry, inflamed, and itchy skin. At night, reduced distractions make itch sensations more noticeable, and natural dips in cortisol (an anti-inflammatory hormone) allow inflammation to increase.
Psoriasis: Though primarily associated with scaling plaques, psoriasis can cause significant itching, especially when lesions form on the upper or lower back. Heat from bedding can exacerbate this sensation.
Notalgia Paresthetica: A lesser-known but increasingly recognized condition characterized by localized itching between the shoulder blades. It's believed to stem from nerve compression in the spine, often due to postural strain or degenerative changes.
“Many patients report that their back itch starts subtly but becomes unbearable by midnight. In cases of notalgia paresthetica, there’s often no visible rash—just relentless itching due to sensory nerve dysfunction.” — Dr. Lena Torres, Neurologist & Pain Specialist
Hormonal and Nervous System Influences
The body’s internal clock regulates more than just sleep—it modulates immune responses, hormone release, and nerve activity, all of which influence skin sensitivity.
At night, the body produces less cortisol and more melatonin. While melatonin supports sleep, it may also enhance histamine release, increasing itch perception. Additionally, core body temperature rises slightly in the evening, leading to mild sweating that can activate itch nerves, particularly under tight clothing or heavy blankets.
Peripheral neuropathy—nerve damage often linked to diabetes, vitamin deficiencies, or autoimmune disorders—can also manifest as isolated itching. Since nerve signals become more erratic at rest, the brain may misinterpret them as itch rather than pain or tingling.
Step-by-Step Guide to Identifying the Cause
Pinpointing the source of nighttime back itching requires a methodical approach. Follow this timeline over 7–10 days to gather meaningful insights:
- Day 1–2: Document symptoms. Note when the itching starts, its intensity, location, and whether scratching provides relief. Record any rashes, redness, or skin changes.
- Day 3: Change laundry routine. Wash all bedding and pajamas with a gentle, fragrance-free detergent. Use an extra rinse cycle.
- Day 4: Adjust room environment. Introduce a humidifier and keep bedroom temperature below 70°F (21°C).
- Day 5: Switch sleepwear. Wear loose, breathable cotton instead of synthetic fabrics.
- Day 6: Apply moisturizer before bed. Use a thick, fragrance-free emollient like ceramide-based cream on your back.
- Day 7: Eliminate potential allergens. Vacuum mattress, rotate pillow, and consider using allergen-proof covers.
- Day 8–10: Evaluate results. If itching improves, one of the above factors was likely contributing. If not, consult a dermatologist or neurologist.
Medical Conditions Linked to Nocturnal Back Itch
While environmental and dermatological factors are common, some systemic illnesses present with itching as an early or primary symptom.
| Condition | How It Causes Itching | Other Symptoms to Watch For |
|---|---|---|
| Diabetes | Nerve damage (diabetic neuropathy) can cause localized or generalized itching, often on limbs or back. | Frequent urination, fatigue, blurred vision, slow-healing wounds |
| Liver Disease (e.g., cholestasis) | Bile salts accumulate in the bloodstream and deposit in skin, triggering intense itch without rash. | Jaundice, dark urine, fatigue, abdominal swelling |
| Kidney Failure | Uremic pruritus occurs when toxins build up in the blood, irritating nerve endings. | Dry skin, fatigue, swelling in legs, difficulty concentrating |
| Thyroid Disorders | Hypothyroidism leads to dry, flaky skin; hyperthyroidism increases sweat and skin sensitivity. | Weight changes, hair loss, mood swings, temperature intolerance |
| Shingles (Pre-Rash Phase) | Viral reactivation affects nerve pathways, often causing burning or itching before rash appears. | Tingling, fever, headache, sensitivity to touch |
If itching persists despite environmental adjustments and is accompanied by any of the above symptoms, medical evaluation is essential. Blood tests for liver function, kidney markers, glucose levels, and thyroid hormones can rule out systemic causes.
Real-Life Example: Sarah’s Persistent Back Itch
Sarah, a 42-year-old office worker, began experiencing intense itching between her shoulder blades every night around 10:30 PM. She initially blamed new laundry soap, but switching brands didn’t help. Over several weeks, she tried antihistamines, moisturizers, and even changed her mattress, with little relief.
During a routine physical, her doctor noticed elevated liver enzymes. Further testing revealed early-stage primary biliary cholangitis—a chronic liver condition that commonly presents with severe nocturnal itching. With treatment, including ursodeoxycholic acid and lifestyle changes, Sarah’s symptoms resolved within two months.
Her case highlights how a seemingly simple issue like back itching can signal a deeper health concern, especially when it defies typical remedies.
Do’s and Don’ts: Managing Nighttime Back Itch
“Patients often scratch until they bleed, worsening the problem. Breaking the itch-scratch cycle is critical.” — Dr. Rajiv Mehta, Dermatologist
| Do’s | Don’ts |
|---|---|
| Use fragrance-free moisturizers nightly | Scratch aggressively—even if it brings temporary relief |
| Wear loose, breathable sleepwear | Use scented lotions or harsh soaps on affected areas |
| Keep nails short to minimize skin damage | Ignore systemic symptoms like fatigue or weight changes |
| Apply cool compresses before bed | Self-diagnose or delay seeing a doctor if symptoms persist |
| Track symptoms in a journal | Assume it’s “just dry skin” without investigating further |
FAQ: Common Questions About Nighttime Back Itching
Can stress really make my back itch at night?
Yes. Stress activates the nervous system and increases inflammatory markers, both of which can amplify itch signals. Anxiety about not sleeping can create a feedback loop: stress causes itching, which disrupts sleep, leading to more stress. Mindfulness techniques, such as deep breathing or guided meditation before bed, may help reduce neurogenic itch.
Is it normal to itch only on one side of the back?
Localized itching on one side—especially between the shoulder blades—can be a sign of notalgia paresthetica or early shingles. It may also result from uneven pressure on the spine during sleep. If unilateral itching persists or evolves into a rash, see a healthcare provider promptly.
Are over-the-counter creams effective?
For mild cases caused by dry skin or minor irritation, OTC hydrocortisone cream (1%) or antihistamine gels can provide temporary relief. However, long-term use of steroid creams on thin back skin can cause thinning and discoloration. Antihistamines like diphenhydramine may help due to their sedative effect, but they don’t address the root cause in non-allergic cases.
Action Plan Checklist
Use this checklist to systematically address your nighttime back itch:
- ☐ Switch to fragrance-free, dye-free laundry detergent
- ☐ Wash bedding weekly in hot water (130°F/54°C or higher)
- ☐ Replace synthetic sleepwear with 100% cotton
- ☐ Install a humidifier in the bedroom, especially in winter
- ☐ Apply a thick, hypoallergenic moisturizer before bed
- ☐ Keep bedroom cool (65–68°F / 18–20°C)
- ☐ Examine your back in a mirror for rashes, bumps, or discoloration
- ☐ Track symptoms for 7–10 days (time, severity, triggers)
- ☐ Schedule a doctor’s visit if no improvement or other symptoms arise
Conclusion: Reclaim Your Rest
An uncontrollably itchy back at night is more than a nuisance—it’s a signal from your body that something needs attention. Whether the cause is as simple as detergent residue or as complex as a metabolic disorder, identifying and addressing the trigger is essential for restoring comfort and sleep quality. Ignoring persistent itching risks worsening skin damage, emotional distress, and missed opportunities to detect underlying illness early.
You don’t have to endure another sleepless night. Start with small, evidence-based changes to your sleep environment and hygiene routine. Track your progress, listen to your body, and seek professional guidance when needed. Relief is possible—and better sleep is within reach.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?