Bad breath, or halitosis, affects millions of people worldwide. Many assume that brushing twice a day is enough to keep their breath fresh. Yet, persistent odor lingers for some—despite diligent oral hygiene. If you're asking, \"Why does my breath smell even after brushing?\" the answer may extend beyond your toothbrush. While poor dental care is a common cause, systemic health issues involving major organs can also contribute. Understanding the deeper causes—from the mouth to the gut and beyond—is essential for effective, long-term solutions.
The Oral Cavity: First Suspect, But Not Always the Culprit
The mouth is home to over 700 species of bacteria. While many are harmless or even beneficial, certain types thrive on food particles left behind after meals. These microbes produce volatile sulfur compounds (VSCs), such as hydrogen sulfide and methyl mercaptan, which emit a rotten-egg-like odor. Even with regular brushing, areas like the back of the tongue, gum pockets, and between teeth often harbor bacteria.
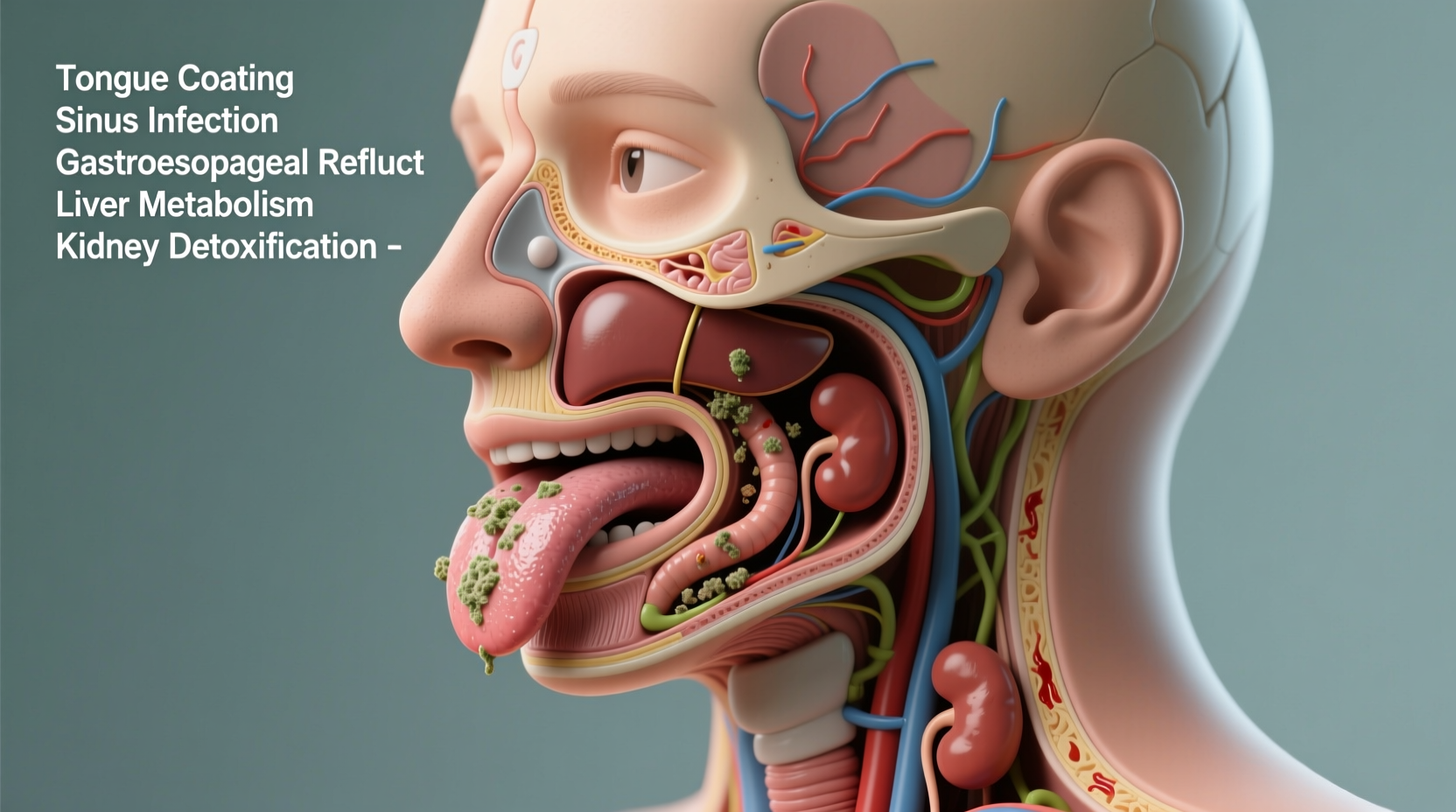
Tongue coating, especially at the base, is a major reservoir for odor-causing bacteria. A 2020 study in the *Journal of Breath Research* found that individuals with thick tongue coatings had significantly higher levels of VSCs. Brushing alone doesn’t remove this biofilm effectively—tongue scraping is necessary.
Dry mouth, or xerostomia, further exacerbates the issue. Saliva naturally cleanses the mouth and neutralizes acids. When saliva flow decreases—due to medications, dehydration, or breathing through the mouth—bacteria multiply rapidly, increasing odor risk.
Beyond the Mouth: Sinus and Respiratory Contributions
Nasal and sinus infections are frequently overlooked sources of bad breath. Postnasal drip occurs when mucus drips down the back of the throat, creating a breeding ground for anaerobic bacteria. These microbes break down proteins in mucus, releasing foul-smelling gases.
Chronic sinusitis, allergies, or deviated septum can lead to persistent postnasal drip. In such cases, breath may carry a musty or fecal-like odor due to stagnant mucus. Tonsil stones—small calcified deposits in the tonsillar crypts—are another related cause. They form from trapped debris and bacteria and often emit a pungent, rotting-cheese smell when dislodged.
“Halitosis isn't always dental. I’ve diagnosed patients with chronic sinusitis solely based on breath odor and history of nasal congestion.” — Dr. Lena Patel, Otolaryngologist
Symptoms Suggesting Sinonasal Involvement
- Frequent throat clearing
- Constant nasal drip
- Recurrent sore throats
- Visible white spots on tonsils
- Mouth breathing, especially at night
Digestive System: How Gut Health Influences Breath
The digestive tract plays a surprisingly direct role in breath quality. Gastroesophageal reflux disease (GERD) allows stomach acid and partially digested food to rise into the esophagus and mouth. This regurgitated material carries an acidic, sour, or fermented odor—distinct from typical bacterial halitosis.
Moreover, small intestinal bacterial overgrowth (SIBO) can lead to excessive gas production, including methane and hydrogen sulfide, which may escape via the breath. A 2016 study published in *The American Journal of Gastroenterology* found that 50% of patients with unexplained halitosis tested positive for SIBO.
H. pylori infection, a bacterium linked to ulcers and gastritis, has also been associated with bad breath. Though not all carriers experience odor, the metabolic byproducts of H. pylori can contribute to a metallic or ammonia-like scent.
| Condition | Odor Type | Associated Symptoms |
|---|---|---|
| GERD | Sour, acidic | Heartburn, regurgitation, bloating |
| SIBO | Rotten eggs, fermented | Gas, diarrhea, abdominal pain |
| H. pylori | Metallic, ammonia | Stomach pain, nausea, loss of appetite |
Liver and Kidney: Hidden Organ Contributors to Breath Odor
When breath smells persist despite excellent oral hygiene and no obvious respiratory or digestive issues, internal organ dysfunction should be considered. The liver and kidneys are critical detoxifiers—when impaired, they allow toxins to accumulate in the bloodstream, some of which are exhaled through the lungs.
Liver failure, particularly in advanced stages like cirrhosis, can result in a distinctive breath odor known as “fetor hepaticus.” This is described as a sweet, musty, or slightly sulfuric smell—sometimes compared to rotten eggs or moldy grain. It results from the liver’s inability to filter dimethyl sulfide and other sulfur-containing compounds, allowing them to enter the breath.
Kidney disease, especially in end-stage renal failure, leads to “uremic breath”—a fishy or ammonia-like odor. This occurs because urea accumulates in the blood and is broken down into ammonia in the saliva. Patients undergoing dialysis often report improved breath once treatment begins, confirming the link.
These conditions are rare but serious. Persistent odd breath combined with symptoms like yellowing skin, swelling in the legs, confusion, or reduced urine output requires urgent testing.
Real-Life Example: When Breath Revealed a Silent Condition
Mark, a 54-year-old teacher, brushed and flossed daily and visited his dentist every six months. Still, coworkers subtly avoided close conversations. His wife mentioned a “sweet, odd” smell on his breath. Initially dismissed as stress-related dry mouth, the odor worsened over months. After a routine blood test revealed elevated liver enzymes, further imaging showed early cirrhosis linked to undiagnosed fatty liver disease. Treatment and lifestyle changes not only improved his liver function but eliminated the breath issue within weeks.
This case illustrates how breath can serve as an early warning sign—long before more obvious symptoms appear.
Systematic Approach to Diagnosing and Treating Persistent Bad Breath
Addressing chronic halitosis requires a step-by-step strategy that evaluates both local and systemic factors. Jumping straight to mouthwash or mints only masks the problem. Instead, follow this structured approach:
- Assess oral hygiene practices: Are you brushing for two minutes twice daily? Flossing? Cleaning your tongue?
- Check for dry mouth: Consider hydration, medications (antihistamines, antidepressants), and breathing habits.
- Evaluate ENT symptoms: Look for signs of sinus infection, postnasal drip, or tonsil stones.
- Review digestive health: Note any acid reflux, bloating, or irregular bowel movements.
- Monitor systemic symptoms: Fatigue, nausea, changes in skin or urine may point to liver or kidney issues.
- Consult professionals: See a dentist, ENT specialist, or gastroenterologist as needed.
- Order diagnostic tests: Blood work, liver/kidney panels, H. pylori breath test, or SIBO testing if indicated.
Actionable Checklist for Fresh Breath
- Brush teeth and tongue for two minutes, twice daily
- Floss or use interdental brushes daily
- Scrape your tongue every morning
- Stay hydrated—aim for 2–2.5 liters of water per day
- Avoid alcohol-based mouthwashes (they dry the mouth)
- Reduce intake of garlic, onions, and coffee
- Quit smoking or vaping
- Treat underlying conditions like GERD or sinusitis
- Visit your dentist every 6 months
- See a doctor if breath persists despite good hygiene
Frequently Asked Questions
Can diabetes cause bad breath?
Yes. Uncontrolled diabetes can lead to ketoacidosis, a dangerous condition where the body burns fat for fuel, producing ketones. One of these, acetone, is exhaled and gives breath a fruity or nail-polish-like odor. This is a medical emergency and requires immediate attention.
Is bad breath contagious?
No, halitosis itself is not contagious. However, the bacteria that cause gum disease or H. pylori can be transmitted through saliva—such as by sharing utensils or kissing. This doesn’t mean you’ll develop bad breath, but it increases the risk if oral hygiene is poor.
Why does my breath stink in the morning even if I brushed before bed?
Overnight, saliva production drops significantly, creating a dry environment where bacteria multiply unchecked. This is normal, but severe morning breath may indicate sleep apnea, mouth breathing, or inadequate evening cleaning. Using a humidifier or nighttime mouthwash may help.
Conclusion: Breath as a Window to Whole-Body Health
Bad breath is more than a social inconvenience—it can be a signal from your body. While most cases stem from oral bacteria or dietary choices, persistent odor despite proper brushing may reflect deeper issues involving the sinuses, digestive tract, liver, or kidneys. Recognizing the connection between breath and systemic health empowers you to seek timely care.
Don’t ignore recurring bad breath. Track your symptoms, improve your hygiene routine, and consult a healthcare provider if the problem persists. Early detection of conditions like liver dysfunction or H. pylori infection can prevent serious complications down the line. Your breath might just be telling you something important—listen closely.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?