For millions of women, a familiar pattern repeats every month: just before or during their menstrual cycle, pimples appear—often along the jawline, chin, and lower cheeks. These breakouts are more than just inconvenient; they can affect confidence and daily comfort. While skincare routines may seem flawless, the root cause often lies beneath the surface, deep within the body’s hormonal fluctuations. Understanding the hormonal link between your period and acne is the first step toward managing it effectively.
Acne around menstruation isn’t random. It’s a well-documented phenomenon tied to shifts in estrogen, progesterone, and testosterone levels throughout the menstrual cycle. This article explores the science behind hormonal acne, identifies who is most affected, and provides actionable solutions grounded in dermatology and endocrinology.
The Menstrual Cycle and Hormonal Fluctuations
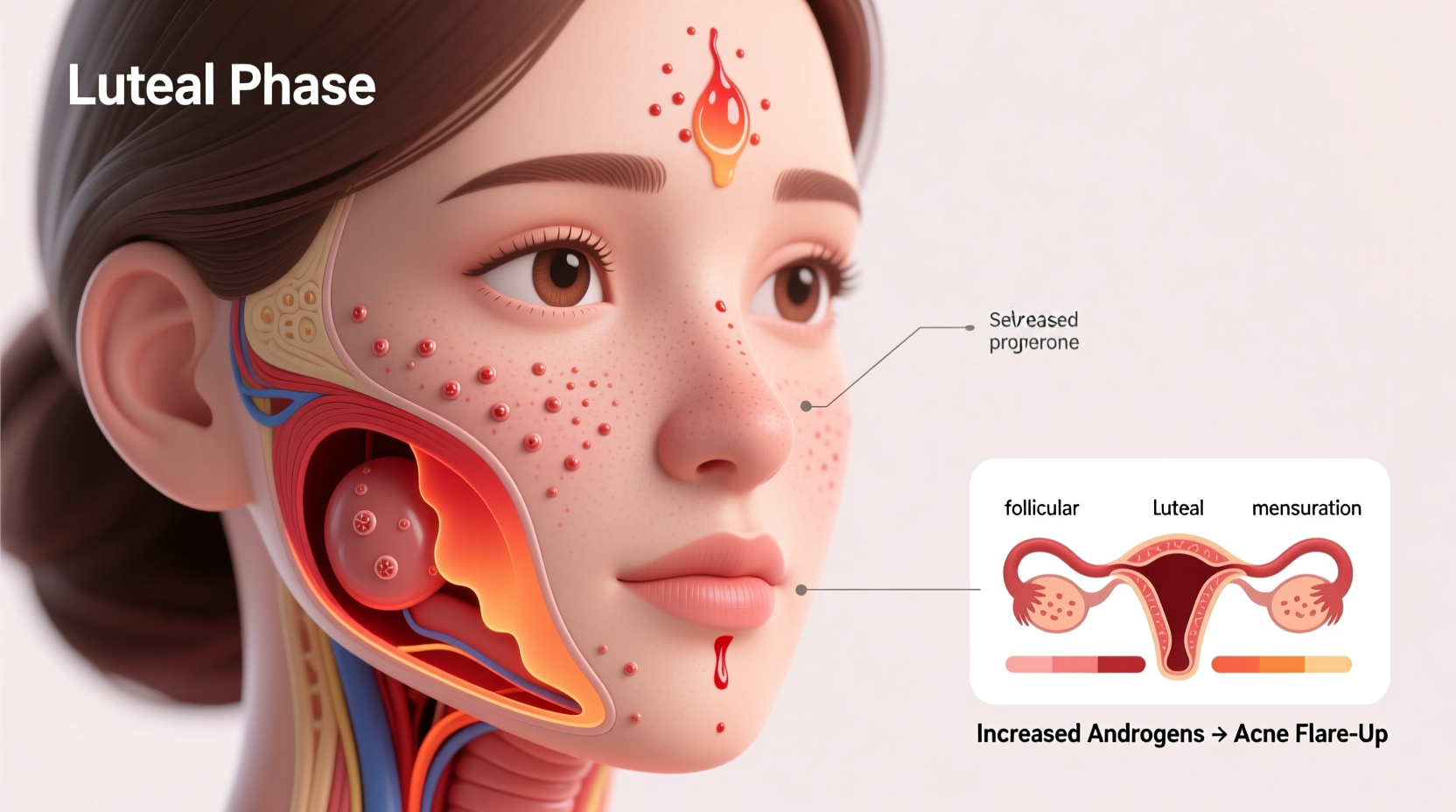
The menstrual cycle, typically lasting 28 days (though it varies), consists of four phases: menstruation, follicular phase, ovulation, and luteal phase. Each phase involves dynamic changes in hormone levels that influence skin health.
During the luteal phase—roughly days 15 to 28—progesterone and estrogen levels begin to drop if pregnancy does not occur. At the same time, testosterone remains relatively stable. This imbalance increases the relative concentration of androgens like testosterone, which stimulate the sebaceous glands in the skin to produce more sebum (oil).
Excess sebum mixes with dead skin cells and bacteria (particularly Propionibacterium acnes), clogging pores and leading to inflammation and acne. This process explains why breakouts commonly emerge 3 to 7 days before menstruation begins—a window known as premenstrual acne.
“Hormonal acne is distinct because it follows a predictable pattern linked to the menstrual cycle. It’s not poor hygiene or diet alone—it’s biochemistry.” — Dr. Lena Patel, Board-Certified Dermatologist
Why the Jawline and Chin Are Common Targets
Unlike teenage acne, which often affects the forehead and nose, hormonal acne tends to cluster on the lower third of the face—especially the jawline, chin, and upper neck. This distribution correlates with higher concentrations of androgen receptors in these areas.
Androgens bind to these receptors, triggering increased sebum production and inflammation. The result? Deep, painful cysts or pustules that are slower to heal and more likely to scar than surface-level blackheads or whiteheads.
Women with polycystic ovary syndrome (PCOS) or other endocrine disorders may experience even more severe hormonal acne due to chronically elevated androgen levels. However, even those with regular cycles can be affected by normal hormonal shifts.
Key Hormones Involved in Period Acne
Understanding the role of specific hormones helps clarify why breakouts happen and how to address them:
- Testosterone: Though present in small amounts in women, testosterone is a potent androgen that directly stimulates oil glands. Even slight increases in its activity can trigger acne.
- Progesterone: Rises after ovulation and can thicken sebum, making it more likely to clog pores.
- Estrogen: Has anti-inflammatory properties and helps regulate oil production. When estrogen drops before menstruation, this protective effect diminishes.
- Cortisol: Stress hormone levels often rise premenstrually, further exacerbating inflammation and sebum output.
The interplay between these hormones creates a perfect storm for acne development. As estrogen and progesterone decline, the skin becomes more sensitive to androgens—even if absolute hormone levels remain within normal ranges.
How to Manage Hormonal Breakouts: A Step-by-Step Guide
Managing period-related acne requires a proactive, cyclical approach rather than reactive spot treatments. Here’s a timeline-based strategy to reduce flare-ups:
- Days 1–14 (Menstrual & Follicular Phase): Focus on gentle exfoliation. Use a salicylic acid cleanser every other day to prevent pore buildup. Maintain hydration with non-comedogenic moisturizers.
- Day 14 (Ovulation): Begin monitoring skin changes. Introduce a topical retinoid (like adapalene) at night to accelerate cell turnover and prevent clogged pores.
- Days 15–28 (Luteal Phase): Ramp up preventive care. Add a benzoyl peroxide spot treatment to target bacteria. Avoid heavy makeup or comedogenic products.
- Pre-Period Window (3–7 Days Before Flow): Start using an anti-inflammatory serum containing niacinamide. Consider over-the-counter pain relief like ibuprofen, which may also reduce inflammatory acne lesions.
- During Menstruation: Simplify routine. Stick to mild cleansers and soothing ingredients like aloe vera or centella asiatica to support healing.
This cyclical skincare method aligns with your body’s natural rhythm, offering protection when vulnerability is highest.
Medical and Long-Term Treatment Options
When lifestyle and topical treatments aren’t enough, medical interventions can offer significant improvement. These should be discussed with a dermatologist or gynecologist:
| Treatment | How It Works | Best For |
|---|---|---|
| Oral Contraceptives | Regulate hormone fluctuations; reduce free testosterone | Women seeking birth control + acne control |
| Spironolactone | Blocks androgen receptors in the skin | Severe hormonal acne unresponsive to topicals |
| Topical Retinoids | Promote cell turnover, unclog pores | Moderate acne prevention |
| Anti-inflammatory Antibiotics | Reduce bacterial load and swelling | Short-term use for acute flare-ups |
Not all treatments suit everyone. For example, spironolactone is highly effective but not recommended for pregnant women or those planning pregnancy. Oral contraceptives require careful evaluation of personal and family medical history.
Do’s and Don’ts for Hormonal Acne Management
Avoid common pitfalls that worsen breakouts. Follow this practical checklist:
| Do’s | Don’ts |
|---|---|
| Wash face twice daily with a gentle, pH-balanced cleanser | Over-wash or scrub aggressively—this irritates skin and increases oil production |
| Use non-comedogenic moisturizers and sunscreens | Skip moisturizer—dry skin signals glands to produce more oil |
| Change pillowcases weekly to reduce bacterial transfer | Touch or pick at acne—this spreads bacteria and causes scarring |
| Manage stress through yoga, meditation, or breathing exercises | Ignore persistent acne—seek professional help early |
Mini Case Study: Sarah’s Journey with Hormonal Acne
Sarah, a 29-year-old graphic designer, had struggled with monthly breakouts for over a decade. Despite trying countless cleansers and serums, her chin would erupt with painful cysts a week before her period. Frustrated, she consulted a dermatologist who asked about her cycle timing.
After confirming the pattern, the doctor prescribed a low-dose combined oral contraceptive containing drospirenone—an anti-androgenic progestin known to improve acne. Within three months, Sarah noticed a dramatic reduction in both frequency and severity of breakouts. She paired this with a nightly adapalene gel and weekly salicylic acid masks, maintaining clear skin with minimal effort.
Her case highlights the importance of diagnosing acne correctly. What looked like inconsistent skincare was actually a hormonal issue requiring systemic treatment.
Frequently Asked Questions
Can diet affect hormonal acne before my period?
Yes. High-glycemic foods (like sugar, white bread, and processed snacks) can spike insulin levels, which in turn may increase androgen activity and sebum production. Dairy, particularly skim milk, has also been linked to acne in some studies due to its hormonal content. Reducing these foods during the luteal phase may help minimize breakouts.
Is hormonal acne permanent?
No. While it can persist for years, especially during reproductive age, it often improves with age or appropriate treatment. Many women find relief after pregnancy, while others benefit from hormonal therapies. With consistent management, flare-ups can become rare and mild.
Can I prevent period breakouts without medication?
Some women successfully manage mild hormonal acne with lifestyle adjustments: consistent sleep, stress reduction, and targeted skincare. However, moderate to severe cases often require medical intervention. Prevention without medication is possible but depends on individual biology and severity.
Expert Insight: The Role of Inflammation
Beyond hormones, inflammation plays a critical role in acne development. Dr. Alan Wu, a clinical dermatologist, emphasizes this connection:
“Hormones set the stage, but inflammation drives the breakout. That’s why treating hormonal acne isn’t just about drying out oil—it’s about calming the immune response in the skin.” — Dr. Alan Wu, Clinical Dermatologist
This insight supports the use of anti-inflammatory ingredients such as niacinamide, green tea extract, and azelaic acid, which can reduce redness and swelling even during high-risk phases.
Conclusion: Take Control of Your Skin Health
Breakouts around your period are not a failure of hygiene or willpower—they are a physiological response to natural hormonal shifts. Recognizing this empowers you to respond strategically rather than reactively.
By tracking your cycle, adjusting your skincare routine in advance, and seeking medical advice when needed, you can significantly reduce or even eliminate monthly flare-ups. Whether through topical treatments, hormonal regulation, or lifestyle changes, effective solutions exist.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?