If you’ve ever looked in the mirror and noticed a familiar bump forming exactly where it always does—perhaps near your chin, beside your nose, or along your jawline—you’re not alone. Persistent acne in the same facial location is more common than many realize, and while occasional breakouts are normal, recurring ones signal deeper imbalances. Understanding the root causes can transform how you manage your skin and prevent future flare-ups.
Repetitive acne isn’t just bad luck; it’s often the result of consistent triggers tied to hormones, hygiene habits, bacteria buildup, or even lifestyle patterns. The key to breaking the cycle lies in identifying what keeps reactivating that specific pore or follicle. This article explores the science behind localized, recurring breakouts and offers actionable strategies to address them at the source.
Anatomy of a Recurring Breakout
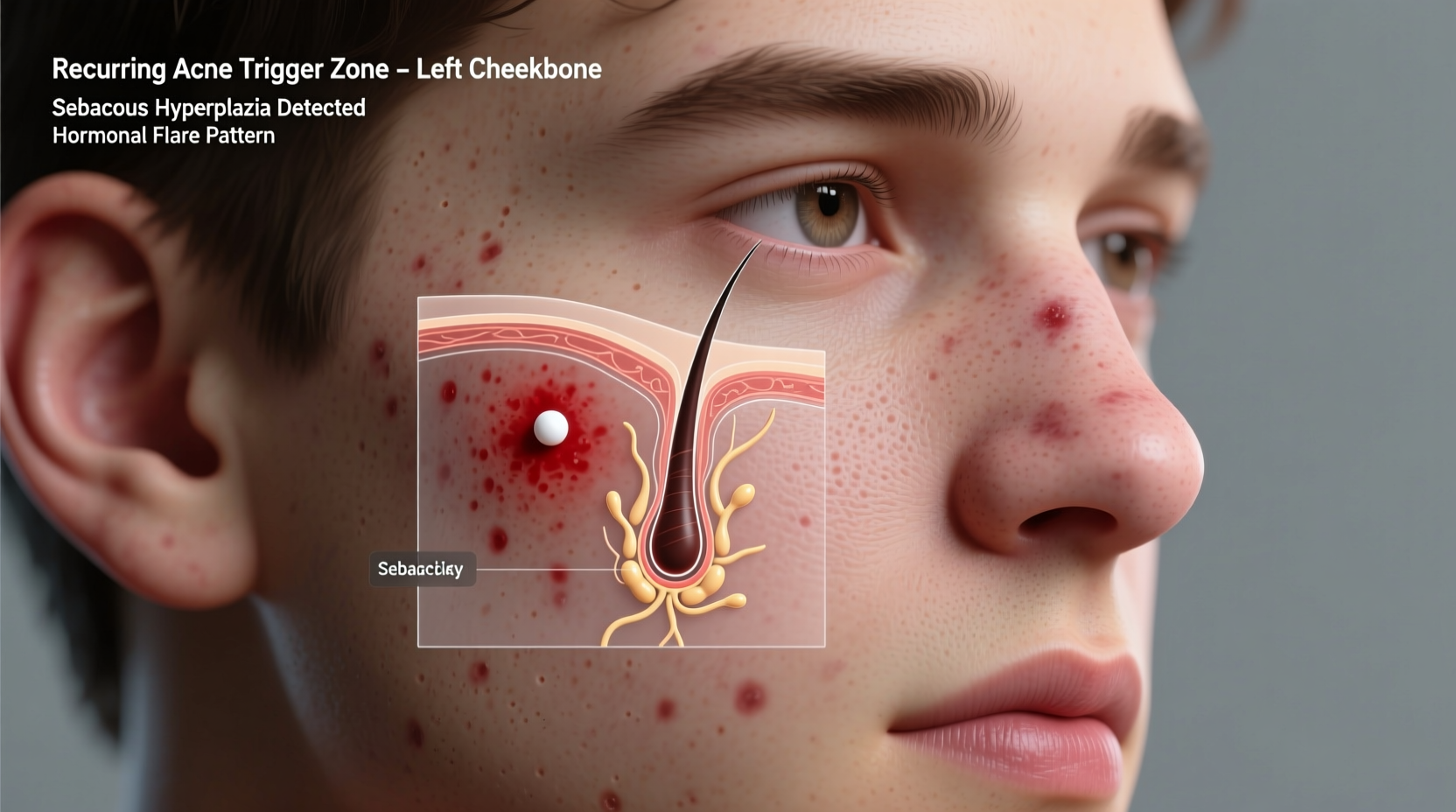
Acne forms when hair follicles become clogged with oil (sebum), dead skin cells, and bacteria. While this process can happen anywhere on the face, some areas are more prone to chronic issues due to higher sebaceous gland concentration, friction, or hormonal sensitivity. When the same spot flares up repeatedly, it usually means one or more contributing factors remain unaddressed.
The lifecycle of a pimple involves inflammation, bacterial colonization (often by Propionibacterium acnes), and immune response. If the environment around a particular pore remains conducive to these conditions—due to trapped oils, irritation, or ongoing stress—the area becomes a hotspot for recurrence.
Hormonal Imbalance: The Silent Instigator
Hormones play a major role in acne development, especially in adult women. Areas like the lower face—jawline, chin, and upper neck—are particularly sensitive to hormonal fluctuations. Androgens, such as testosterone (even in small amounts in women), stimulate sebum production, which can overwhelm pores in susceptible zones.
Many individuals experience monthly breakouts before menstruation due to rising progesterone levels, which increase oiliness and inflammation. Over time, this creates a pattern: if hormone-driven oil spikes occur consistently, the same pores may struggle month after month.
“Hormonal acne tends to cluster in the lower third of the face because those sebaceous glands have more androgen receptors.” — Dr. Nina Patel, Dermatologist and Skin Health Specialist
Polycystic ovary syndrome (PCOS) and other endocrine disorders can also amplify this effect. Blood tests measuring DHEA-S, testosterone, and insulin resistance markers may help identify underlying causes when topical treatments fail.
Friction and Mechanical Irritation
Physical pressure on the skin can trigger a condition known as acne mechanica—acne caused by heat, rubbing, or occlusion. Common culprits include:
- Resting your cheek on your hand while working
- Wearing tight helmets, headbands, or face masks
- Using phones pressed against the same side of the face
- Sleeping position that favors one side
These actions create microtrauma, trap sweat and bacteria, and disrupt the skin barrier. A pore already weakened by past inflammation is especially vulnerable. For example, someone who frequently cradles their phone against their jaw may develop stubborn cysts on that side over time.
Common Sources of Facial Friction
| Source | Affected Area | Prevention Strategy |
|---|---|---|
| Phone contact | Jawline, ear-to-cheek | Use speakerphone or clean screen daily |
| Sports helmets/straps | Forehead, temples | Wash gear regularly; apply breathable barrier cream |
| Pillowcase contact | One-sided cheek breakouts | Change pillowcases every 2–3 days; consider silk fabric |
| Frequent touching | Chin, nose crease | Break habit; wash hands often |
Bacterial Colonization and Pore Memory
Some dermatologists refer to \"pore memory\"—a concept suggesting that once a pore has experienced severe inflammation, it may be structurally altered, making it easier for debris to accumulate again. Additionally, certain strains of acne-causing bacteria can colonize specific regions, creating a reservoir that reinfects the same site.
This is especially true if you've popped or picked at a blemish, introducing surface bacteria deeper into the follicle. Even after healing, residual biofilm—a slimy layer formed by bacteria—can linger beneath the skin, priming the area for relapse.
Antibacterial ingredients like benzoyl peroxide, salicylic acid, or topical antibiotics (when prescribed) help reduce bacterial load. However, long-term reliance on antibiotics can lead to resistance, so targeted use is essential.
Lifestyle and Environmental Triggers
Daily routines often contribute unknowingly to recurrent breakouts. Diet, stress, sleep quality, and skincare product choices all influence skin health. Consider the following real-life scenario:
Mini Case Study: Sarah’s Chin Breakouts
Sarah, a 28-year-old graphic designer, struggled with painful cysts on her right chin every month. Despite trying various creams and cleansers, they kept returning. After tracking her habits, she realized she always rested her right hand on her chin while designing. Her phone was also habitually held against that side during calls. She switched to voice commands, changed her posture, and began cleaning her phone nightly. Within two months, breakouts decreased significantly.
Environmental factors like pollution, humidity, and product buildup also play roles. Hair products containing oils or silicones can drip onto the forehead or hairline, clogging pores. Similarly, heavy moisturizers or comedogenic makeup may settle into the same creases or folds where acne recurs.
Checklist: Reduce Recurrent Acne Triggers
- Identify physical contact points (phone, hands, pillow)
- Clean devices and accessories daily
- Avoid sharing towels or using dirty makeup brushes
- Switch to non-comedogenic skincare and hair products
- Track breakouts alongside menstrual cycle or stress levels
- Wash pillowcases and hats twice weekly
- Apply spot treatments early, before full inflammation develops
Step-by-Step: Breaking the Cycle of Recurring Acne
Addressing persistent breakouts requires consistency and precision. Follow this timeline to reset your skin and prevent repeat flare-ups:
- Week 1: Audit Your Routine
Document everything that touches your face: phone, glasses, hands, hair, clothing. Note any patterns in timing—do breakouts align with your period, work stress, or dietary changes? - Week 2: Eliminate Mechanical Stressors
Change habits that cause friction. Use a hands-free device for calls, adjust your workstation to avoid leaning on your face, and switch to silk pillowcases to reduce nighttime irritation. - Week 3: Optimize Skincare
Introduce a gentle exfoliant (like salicylic acid) 2–3 times a week to clear dead skin from the affected zone. Pair with a lightweight, non-comedogenic moisturizer. Avoid over-drying, which can worsen oil production. - Week 4: Target Bacteria and Inflammation
Apply a benzoyl peroxide spot treatment (2.5%–5%) directly to the trouble area every other night. If sensitive, buffer with moisturizer. Monitor for improvement without excessive dryness. - Month 2+: Evaluate and Adjust
If no improvement, consult a dermatologist. You may need prescription retinoids (like tretinoin), oral contraceptives (for hormonal balance), or spironolactone to regulate androgen activity.
When to See a Professional
Over-the-counter solutions work for mild cases, but chronic, deep, or scarring acne warrants medical attention. A board-certified dermatologist can perform a comprehensive evaluation and recommend advanced treatments such as:
- Topical retinoids to normalize cell turnover
- Oral antibiotics (short-term) for inflammatory control
- Hormonal therapy for cyclical breakouts
- Chemical peels or laser treatments to remodel scarred tissue
Early intervention prevents post-inflammatory hyperpigmentation and permanent textural changes. If your breakout pattern persists beyond three months despite consistent care, professional guidance is strongly advised.
Frequently Asked Questions
Can a single pore get acne repeatedly?
Yes. Once a pore experiences significant inflammation, its lining can become irregular, making it easier for oil and dead skin to accumulate again. Plus, lingering bacteria or biofilm can reignite infection in the same location.
Does diet affect recurring acne in one spot?
Indirectly. High-glycemic foods (like sugar and refined carbs) and dairy have been linked to increased systemic inflammation and insulin spikes, which can boost sebum production. While they don’t target one spot specifically, they lower overall skin resilience, allowing localized triggers to take hold more easily.
Is it safe to extract recurring pimples at home?
No. Repeated squeezing damages surrounding tissue, spreads bacteria, and increases the risk of scarring. Even if pus appears, forcing drainage prolongs healing. Use warm compresses and spot treatments instead, and seek professional extraction if necessary.
Conclusion: Take Control of Your Skin’s Story
Recurring facial breakouts aren’t random—they’re signals. Each flare-up in the same spot is an invitation to examine your habits, environment, and internal health. Whether it’s a hormonal shift, unnoticed friction, or a bacterial stronghold, the solution begins with awareness and ends with consistent action.
You don’t have to live with predictable pimples. By mapping your triggers, refining your routine, and seeking expert help when needed, you can restore balance and finally break free from the cycle. Your skin deserves clarity—not repetition.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?