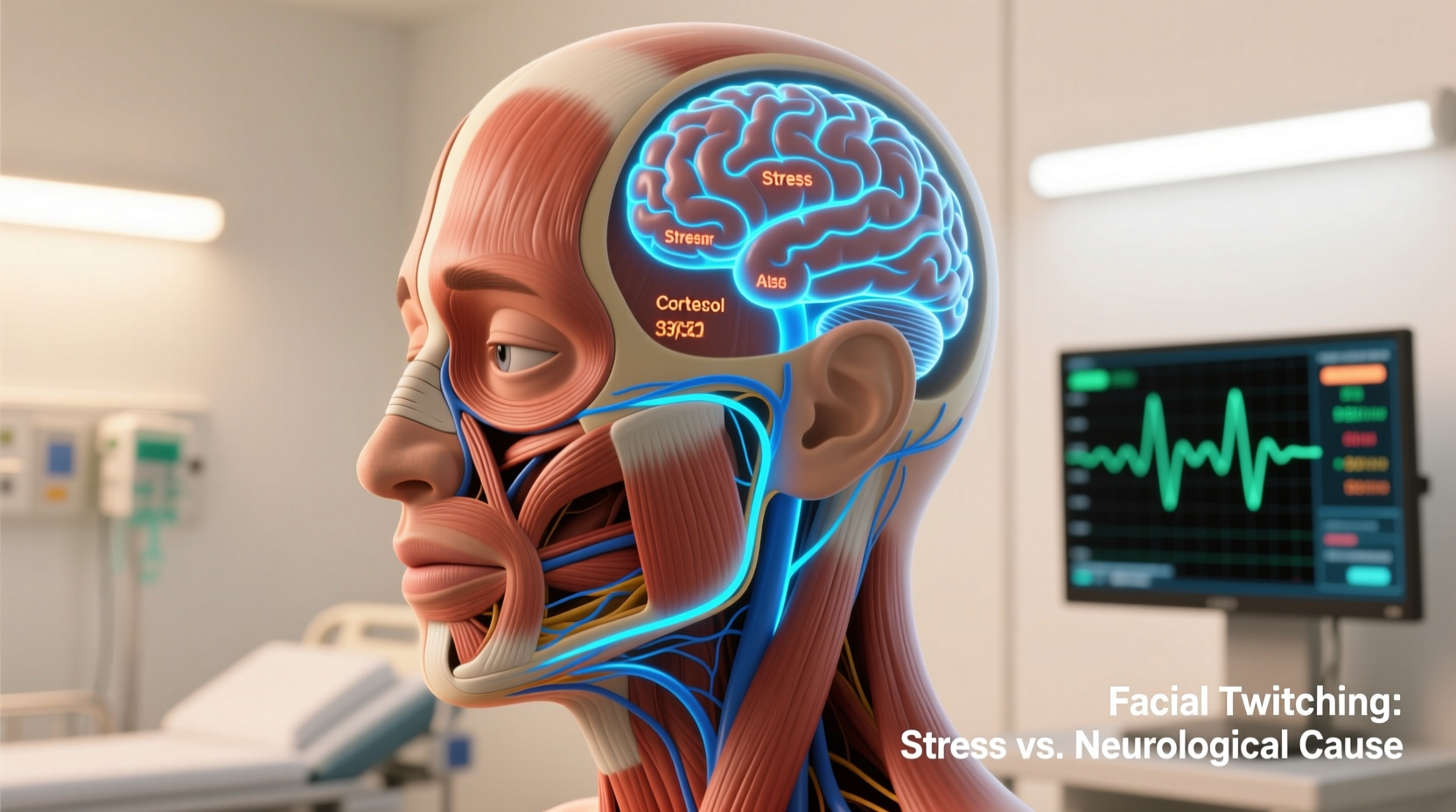
Facial twitching—brief, involuntary contractions of the muscles around the eye, mouth, or cheek—is something most people experience at least once. While often harmless and fleeting, persistent or recurring twitches can raise concerns. Is it just stress? Fatigue? Or could it signal an underlying neurological condition? Understanding the causes, triggers, and warning signs helps determine whether your facial twitch is a temporary annoyance or a symptom that warrants medical attention.
Common Causes of Facial Twitching
Facial muscle spasms are usually benign and resolve on their own. The most frequent causes are related to lifestyle factors rather than serious health conditions.
- Stress and Anxiety: High cortisol levels from chronic stress disrupt nervous system balance, increasing nerve excitability and triggering muscle twitches.
- Sleep Deprivation: Lack of quality sleep affects neurotransmitter regulation, leading to overactive motor neurons.
- Caffeine Overconsumption: Excessive intake of coffee, energy drinks, or stimulants can overstimulate the central nervous system.
- Dry Eyes or Eye Strain: Prolonged screen time or uncorrected vision issues may cause eyelid twitching (myokymia).
- Nutritional Deficiencies: Low levels of magnesium, calcium, or potassium impair normal muscle function and nerve signaling.
- Dehydration: Electrolyte imbalances affect neuromuscular communication, potentially causing random contractions.
When Facial Twitching Signals a Neurological Issue
While most cases are benign, certain patterns suggest possible neurological involvement. These conditions require evaluation by a neurologist.
Benign Fasciculation Syndrome (BFS)
This condition involves persistent muscle twitching without progressive weakness or degeneration. It’s often linked to anxiety, fatigue, or physical exertion but lacks identifiable structural damage in nerves or muscles.
Hemifacial Spasm
A rarer condition where involuntary contractions affect one side of the face, typically starting near the eye and spreading to the mouth. It's commonly caused by compression of the facial nerve (cranial nerve VII) by a blood vessel. Unlike simple eyelid twitching, hemifacial spasm doesn’t stop during sleep and tends to worsen over time.
“Persistent unilateral facial twitching beyond a few weeks should prompt imaging like an MRI to rule out vascular compression or tumors.” — Dr. Lena Patel, Neurologist, Johns Hopkins Medicine
Bell’s Palsy
An acute facial nerve paralysis that may be preceded or followed by muscle twitching during recovery as nerves regenerate. Often associated with sudden facial droop, altered taste, and ear pain.
Multiple Sclerosis (MS) or Parkinson’s Disease
In rare instances, facial twitching can be an early sign of MS or Parkinson’s, especially if accompanied by other symptoms such as tremors, coordination problems, vision changes, or cognitive shifts. However, isolated twitching alone is not diagnostic.
Do’s and Don’ts: Managing Facial Twitches
| Do’s | Don’ts |
|---|---|
| Maintain consistent sleep (7–9 hours per night) | Consume more than 400mg of caffeine daily |
| Practice stress-reduction techniques (meditation, breathing exercises) | Ignore worsening or spreading twitching |
| Stay hydrated and eat magnesium-rich foods (spinach, almonds, avocado) | Rub or press the twitching area aggressively |
| Use lubricating eye drops if experiencing dry eyes | Self-diagnose using online symptom checkers |
| Keep a symptom journal tracking frequency and triggers | Delay seeing a doctor if twitching lasts over 3 weeks |
Real-Life Example: Recognizing When to Seek Help
Sarah, a 38-year-old graphic designer, began noticing her left eyelid twitching after a particularly intense project deadline. She dismissed it initially, attributing it to long hours and increased coffee intake. Over the next two weeks, the twitching spread to her cheek and didn’t subside even after improving her sleep and cutting back on caffeine. Concerned, she visited a neurologist who ordered an MRI. The scan revealed a small artery pressing against her facial nerve—a diagnosis of hemifacial spasm. With early intervention, including Botox injections and monitoring, Sarah avoided further progression.
This case illustrates how a seemingly minor symptom can escalate. Early professional assessment prevented potential complications like chronic muscle tightness or functional impairment.
Step-by-Step Guide to Addressing Facial Twitching
If you're experiencing random facial twitches, follow this practical timeline to assess and manage the issue effectively:
- Week 1: Monitor and Document
Note when the twitch occurs, its duration, location, and any possible triggers (e.g., stress, lack of sleep, screen time). Use a notebook or mobile app to log entries daily. - Week 2: Adjust Lifestyle Factors
Reduce caffeine intake, aim for 7–9 hours of sleep, incorporate relaxation techniques (like box breathing or yoga), and increase water and magnesium-rich food consumption. - Week 3: Evaluate Progress
If the twitch has diminished or stopped, continue healthy habits. If unchanged or worsening, prepare to consult a healthcare provider. - Week 4: Schedule Medical Consultation
Visit your primary care physician or a neurologist. Bring your symptom log and be ready to discuss family history, medications, and overall health. - Follow-Up: Diagnostic Testing (if needed)
Depending on clinical suspicion, your doctor may recommend electromyography (EMG), MRI, or blood tests to check electrolytes and thyroid function.
Checklist: When to See a Doctor
Use this checklist to determine whether your facial twitch requires medical evaluation:
- ✅ Twitch persists longer than three weeks despite lifestyle changes
- ✅ Affects multiple areas of the face or spreads to other regions
- ✅ Occurs on only one side of the face consistently
- ✅ Accompanied by facial weakness, drooping, or difficulty closing the eye
- ✅ Happens during rest or sleep (not typical of benign twitches)
- ✅ Associated with headaches, dizziness, hearing changes, or vision disturbances
- ✅ You have a history of neurological disorders or recent head trauma
If you check two or more items, schedule a visit with a neurologist promptly.
Frequently Asked Questions
Can anxiety really cause facial twitching?
Yes. Anxiety increases sympathetic nervous system activity, which heightens muscle tension and nerve firing. This hyperexcitability can manifest as facial twitches, especially around the eyes. Managing anxiety through therapy, mindfulness, or medication often reduces or eliminates these symptoms.
Is facial twitching a sign of a stroke?
Isolated facial twitching is not typically a sign of stroke. Strokes usually present with sudden-onset facial droop, arm weakness, and speech difficulties occurring together. However, any new neurological symptom should be evaluated promptly to rule out serious conditions.
Can children get facial tics or twitching?
Yes. Children may develop transient tics—such as eye blinking, nose wrinkling, or shoulder shrugging—often related to stress, fatigue, or mild neurological immaturity. Most resolve within months. Persistent or disruptive tics may indicate Tourette syndrome and warrant pediatric neurology consultation.
Conclusion: Take Control of Your Health
Random facial twitching is usually a temporary response to stress, fatigue, or nutritional imbalance. In most cases, simple lifestyle adjustments bring relief within days or weeks. But when twitching becomes persistent, asymmetric, or accompanied by other neurological symptoms, it’s crucial not to ignore it. Early evaluation can differentiate between benign causes and conditions requiring targeted treatment.
Your body sends signals for a reason. Listening carefully—tracking symptoms, making informed changes, and seeking expert guidance when needed—is the best way to maintain both neurological health and peace of mind.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?