If you’ve ever stood up from a chair, swung your leg in a lunge, or finished a yoga session only to hear a loud snap or click in your hip, you’re not alone. This phenomenon—commonly referred to as “snapping hip syndrome”—affects athletes, dancers, office workers, and weekend warriors alike. While often painless at first, persistent popping can signal underlying biomechanical imbalances that, if ignored, may lead to discomfort or injury over time.
Snapping hip syndrome isn’t just a quirky bodily sound—it’s a mechanical event with identifiable causes, patterns, and solutions. Understanding what’s happening inside your joint and surrounding tissues is the first step toward restoring smooth, silent movement.
What Is Snapping Hip Syndrome?
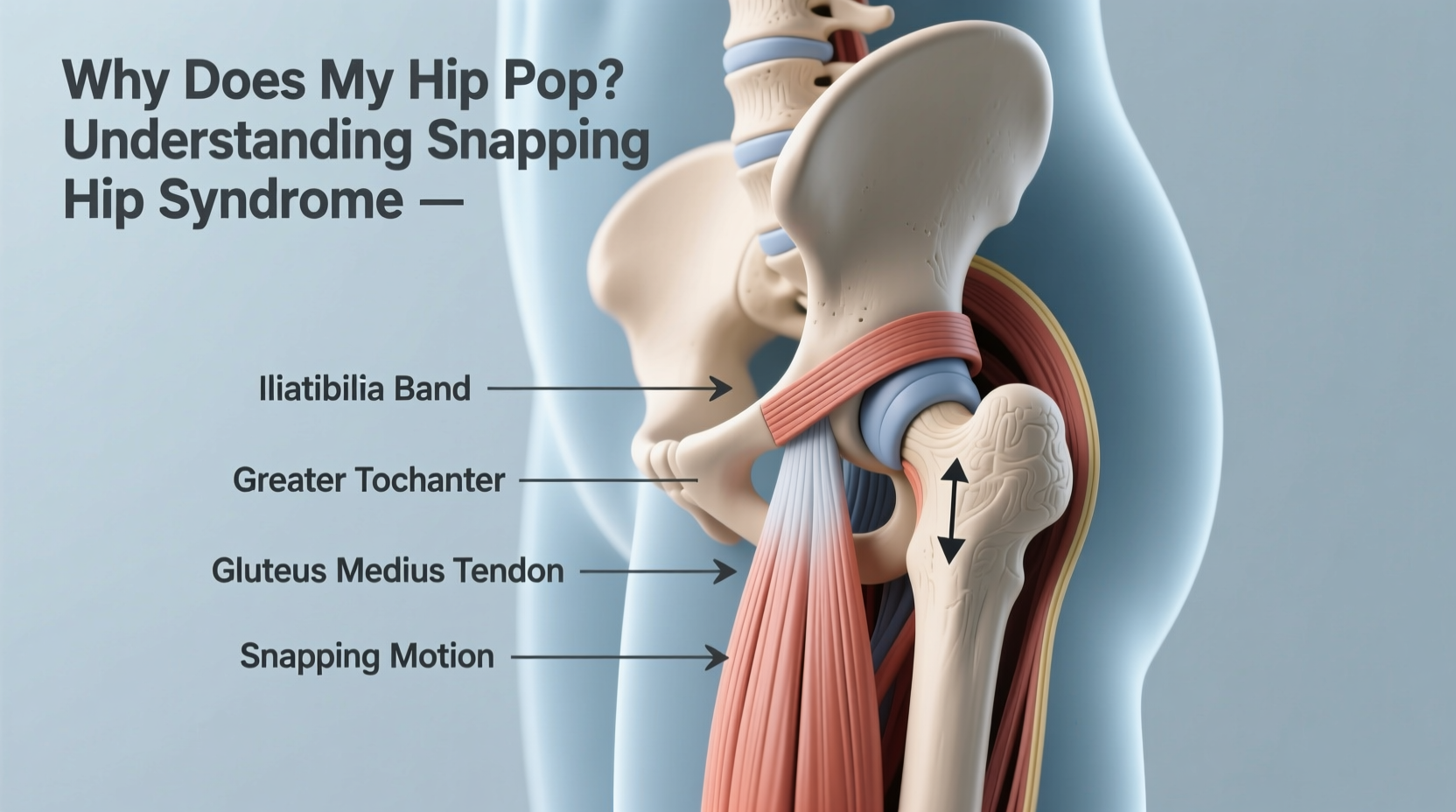
Snapping hip syndrome (also known as coxa saltans) refers to a sensation or audible snap felt around the hip joint during movement. It typically occurs when a tendon or muscle slides over a bony prominence in the hip, creating a flicking motion. The condition is classified into three types based on location:
- External snapping: Caused by the iliotibial (IT) band or gluteus maximus tendon moving over the greater trochanter (the bony point on the side of the hip).
- Internal snapping: Results from the iliopsoas tendon sliding over the iliopectineal eminence or femoral head at the front of the hip.
- Intra-articular snapping: Originates within the joint itself, often due to labral tears, cartilage damage, or loose bodies.
External and internal forms are usually benign and mechanical, while intra-articular causes require medical evaluation because they involve structural damage.
Common Causes Behind the Snap
The root cause of snapping hip syndrome often lies in muscle imbalances, repetitive motions, or anatomical variations. Key contributors include:
- Tightness in major muscle groups: Overly tight IT bands, hip flexors (especially iliopsoas), hamstrings, or glutes increase friction across bony landmarks.
- Muscle weakness: Weak gluteus medius or core muscles force other structures to compensate, altering hip mechanics.
- Repetitive movements: Activities like running, dancing, cycling, or weightlifting can exacerbate repetitive tendon gliding.
- Anatomical factors: Slight variations in bone shape or tendon insertion points make some individuals more prone to snapping.
- Previous injuries: Untreated sprains, strains, or joint instability may predispose someone to altered movement patterns.
Dancers and gymnasts experience snapping hips at higher rates due to extreme ranges of motion. However, sedentary individuals aren't immune—prolonged sitting shortens hip flexors, setting the stage for internal snapping when they stand or stretch.
“Over 70% of dancers report experiencing hip snapping at some point. In most cases, it starts painlessly but can evolve into inflammation if biomechanics aren’t addressed.” — Dr. Lena Reyes, Sports Medicine Physician
How to Identify Your Type of Hip Snap
Pinpointing where the snap occurs helps determine whether it’s muscular-tendon related or requires imaging. Use this guide to self-assess:
| Location of Snap | Possible Cause | Associated Movements |
|---|---|---|
| Side of hip | IT band or gluteus maximus over greater trochanter | Standing up, walking, climbing stairs |
| Front of hip/groin | Iliopsoas tendon over pelvic brim or femoral head | Lunging, lifting knee, transitioning from sit to stand |
| Deep in groin or central hip | Intra-articular issue (labral tear, cartilage defect) | Rotational movements, squatting, pivoting |
| Back of hip | Rare; possibly hamstring origin or ischial tuberosity involvement | Bending forward, sprinting |
A simple test: Lie on your side and slowly extend and flex your top leg. If you feel a snap near the bony point on the side of your hip, it’s likely external snapping. For front-side snapping, lie on your back and bring one knee toward your chest—listen and feel for a pop near the groin.
Mini Case Study: The Dancer’s Dilemma
Maya, a 24-year-old contemporary dancer, began noticing a sharp snap on the outside of her right hip during développé movements. Initially painless, it progressed to soreness after rehearsals. An assessment revealed excessive tightness in her IT band and weakness in her gluteus medius. After six weeks of targeted stretching, foam rolling, and strength training focused on hip stabilization, the snapping reduced significantly. Her case highlights how early intervention prevents progression from mechanical noise to painful tendinopathy.
Effective Treatment and Prevention Strategies
Most cases of snapping hip syndrome respond well to conservative care. A multi-pronged approach addresses both symptoms and root causes.
Step-by-Step Recovery Plan
- Reduce aggravating activities: Modify exercises that provoke snapping (e.g., deep lunges, high kicks) temporarily.
- Stretch tight structures: Focus on the IT band, hip flexors, and hamstrings daily. Hold each stretch for 30–45 seconds, repeat 2–3 times per side.
- Strengthen stabilizers: Perform clamshells, side planks, bridges, and banded walks to activate gluteus medius and maximus.
- Improve neuromuscular control: Practice single-leg balance drills and controlled squats to enhance hip alignment.
- Use soft tissue release: Foam roll the outer thigh and quadriceps cautiously—avoid direct pressure on painful areas.
- Gradual return to activity: Reintroduce dynamic movements slowly, monitoring for recurrence.
When to Seek Medical Evaluation
While most snapping is benign, red flags warrant professional assessment:
- Pain accompanying the snap
- Swelling or warmth around the hip
- Sensation of locking or catching
- Reduced range of motion
- History of trauma or dislocation
In such cases, diagnostic tools like MRI or ultrasound can detect labral tears or cartilage damage. Physical therapy remains the cornerstone of treatment, though corticosteroid injections or surgery may be considered for severe intra-articular issues.
Frequently Asked Questions
Is snapping hip syndrome dangerous?
Not inherently. Many people live with painless snapping their entire lives. However, chronic friction can lead to bursitis or tendon irritation over time, so monitoring changes is important.
Can I continue exercising with a snapping hip?
Yes, if it’s pain-free. Modify high-risk movements and prioritize form. Incorporate corrective exercises to prevent deterioration. Stop any activity causing pain.
Will snapping hip go away on its own?
Sometimes. Mild cases resolve with rest and improved mobility. But without addressing muscle imbalances, recurrence is common. Long-term resolution usually requires consistent corrective work.
Putting It All Together: A Checklist for Action
To manage and prevent snapping hip syndrome, follow this practical checklist:
- ✅ Assess where and when the snap occurs
- ✅ Rule out pain, swelling, or joint dysfunction
- ✅ Stretch hip flexors and IT band daily
- ✅ Strengthen glutes and core 3x per week
- ✅ Avoid prolonged sitting; take standing breaks every 30 minutes
- ✅ Warm up properly before physical activity
- ✅ Consult a physical therapist if symptoms persist beyond 4–6 weeks
Conclusion: Listen to Your Body’s Signals
Your body communicates through movement. A popping hip might seem trivial, but it’s feedback—a sign that something in your kinetic chain is working harder than it should. Whether you're an elite athlete or someone who walks daily, maintaining hip health ensures longevity in motion.
By integrating mindful stretching, intelligent strengthening, and timely intervention, you can silence the snap and move with confidence. Don’t wait for pain to act. Start today—your hips carry you through life. Treat them with the attention they deserve.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?