Many people notice a clicking, popping, or cracking sound in their jaw when chewing, yawning, or speaking. While occasional noise from the jaw joint is common and usually harmless, persistent or painful cracking can signal an underlying issue. Understanding the mechanics behind this phenomenon—and knowing when it’s time to seek medical advice—can help prevent complications and maintain long-term oral health.
The temporomandibular joint (TMJ) connects your jawbone to your skull, just in front of each ear. It’s one of the most complex joints in the body, allowing for smooth up-and-down and side-to-side movement necessary for talking, chewing, and swallowing. When this joint functions normally, it operates silently. But when something disrupts its alignment or function, audible signs like cracking may appear.
What Causes Jaw Cracking During Chewing?
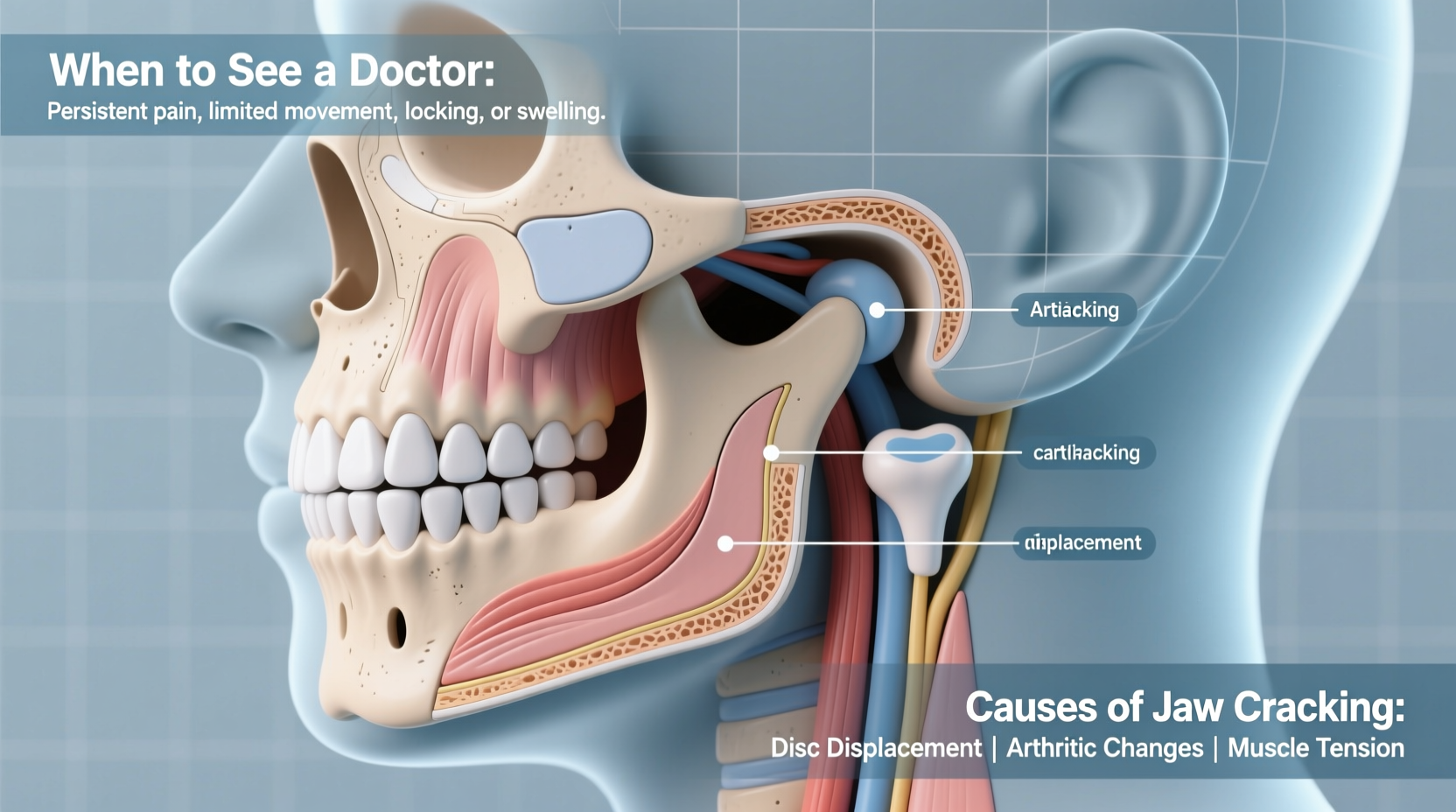
Jaw cracking typically results from irregular movement within the TMJ. Several anatomical and behavioral factors contribute to these sounds:
- Disc displacement: The TMJ contains a small disc of cartilage that cushions the joint. If this disc slips out of place, it can cause a pop or click as the jaw moves.
- Gas release: Like knuckles, synovial joints such as the TMJ contain fluid and gases. A sudden change in pressure can create a bubble that pops, producing a harmless cracking sound.
- Muscle tension: Stress-induced clenching or teeth grinding (bruxism) tightens the muscles around the jaw, increasing strain on the joint and potentially leading to noise.
- Arthritis: Osteoarthritis or rheumatoid arthritis can degrade joint tissue, causing rough surfaces to rub together and produce grating sounds.
- Injury or trauma: Past jaw injuries—even minor ones—can alter joint mechanics and lead to long-term dysfunction.
For many individuals, jaw cracking occurs without pain or limitation and resolves on its own. However, when accompanied by discomfort, limited motion, or worsening symptoms, it may indicate a temporomandibular disorder (TMD).
When Is Jaw Cracking Normal vs. a Sign of Trouble?
Not all jaw noises are concerning. In fact, studies suggest that up to 36% of healthy adults experience some form of TMJ sound without pain or functional impairment. The key distinction lies in whether the sound is isolated or part of a broader pattern of dysfunction.
Occasional, painless cracking during wide mouth opening or chewing tough food is generally benign. It becomes problematic when:
- The sound becomes frequent or constant
- Pain develops in the jaw, face, neck, or ears
- Jaw movement feels stiff or locks open/closed
- Headaches, especially near the temples, accompany the noise
- Chewing becomes difficult or uncomfortable
If any of these red flags appear, the condition may progress beyond simple joint noise into clinically significant TMD, which affects over 10 million Americans annually.
“While joint sounds alone don’t always require treatment, we start paying close attention when patients report pain, reduced range of motion, or interference with daily activities.” — Dr. Alan Foster, Oral & Maxillofacial Specialist
Common Risk Factors for Problematic Jaw Cracking
Certain lifestyle habits and health conditions increase the likelihood of developing symptomatic TMD. Recognizing these risk factors allows for early intervention and prevention.
| Risk Factor | Description | Prevention Strategy |
|---|---|---|
| Teeth Grinding (Bruxism) | Often occurs at night; increases pressure on TMJ | Use a night guard prescribed by a dentist |
| High Stress Levels | Leads to muscle tension and jaw clenching | Practice relaxation techniques like deep breathing or meditation |
| Poor Posture | Slouching shifts head forward, straining jaw alignment | Maintain ergonomic workspace setup |
| Jaw Trauma | Previous injury can misalign the joint | Wear protective gear during contact sports |
| Connective Tissue Disorders | Conditions like Ehlers-Danlos affect joint stability | Monitor joint symptoms with a specialist |
Real-Life Example: Sarah’s Experience with Jaw Pain
Sarah, a 32-year-old graphic designer, began noticing her jaw cracked every time she chewed apples or yawned widely. At first, it didn’t hurt, so she ignored it. Over six months, however, the cracking became louder and was followed by dull aching near her right ear. One morning, her jaw locked mid-yawn, requiring gentle manipulation to close her mouth.
After visiting an orofacial pain specialist, Sarah learned she had anterior disc displacement with reduction—a condition where the TMJ disc temporarily slips forward and snaps back into place during movement. Her job-related stress and nighttime teeth grinding were major contributors. With a custom night guard, physical therapy exercises, and stress management strategies, her symptoms improved significantly within three months.
When Should You See a Doctor?
Knowing when to seek professional help is crucial. Early diagnosis improves outcomes and prevents chronic pain or permanent joint damage.
You should schedule an appointment with a healthcare provider—preferably a dentist, oral surgeon, or TMJ specialist—if you experience:
- Pain during jaw movement: Discomfort while chewing, speaking, or opening your mouth wide.
- Locking or catching: Your jaw gets stuck open or closed, even briefly.
- Swelling around the joint: Visible inflammation near the ear or temple area.
- Clicking that worsens over time: Sounds become more frequent, louder, or painful.
- Associated symptoms: Headaches, earaches, tinnitus (ringing in ears), or facial numbness.
Diagnostic evaluation typically includes a physical exam of jaw motion and muscle tenderness, along with imaging such as panoramic X-rays, MRI, or CT scans to assess soft tissues and bone structure.
Step-by-Step Guide to Initial Self-Care
Before seeing a doctor, you can take proactive steps to reduce strain on the TMJ and possibly alleviate mild symptoms:
- Rest the jaw: Eat soft foods, avoid gum, and limit wide yawning or loud singing.
- Apply warmth: Use a warm compress for 15 minutes several times a day to relax tight muscles.
- Practice gentle stretching: Slowly open and close your mouth without forcing motion.
- Manage stress: Engage in mindfulness, yoga, or breathing exercises to reduce clenching.
- Improve posture: Sit upright with shoulders back and chin slightly tucked to align the head properly.
- Use over-the-counter pain relief: NSAIDs like ibuprofen can reduce inflammation and discomfort temporarily.
Treatment Options for Persistent Jaw Cracking
If self-care doesn’t improve symptoms, medical or dental interventions may be necessary. Treatment depends on the underlying cause and severity.
- Occlusal appliances (night guards): Custom-fitted mouthguards prevent teeth grinding and reposition the jaw to relieve pressure.
- Physical therapy: Specialized exercises strengthen jaw muscles and improve coordination.
- Medications: Muscle relaxants, anti-inflammatories, or low-dose antidepressants may be prescribed for pain and muscle spasm.
- Injections: Corticosteroid or Botox injections can reduce inflammation and relax overactive muscles.
- Surgery: Reserved for severe cases involving structural damage unresponsive to conservative care.
Most patients respond well to non-invasive treatments. According to the American Academy of Orofacial Pain, about 85% of TMD cases improve with conservative management within six to eight weeks.
Frequently Asked Questions
Is jaw cracking dangerous?
Not necessarily. Occasional, painless cracking is common and often harmless. However, if it’s associated with pain, limited movement, or locking, it could indicate a developing joint disorder that warrants evaluation.
Can cracked teeth cause jaw popping?
Indirectly, yes. Damaged or uneven teeth alter your bite, forcing the jaw to compensate during chewing. This misalignment can strain the TMJ and contribute to abnormal sounds or discomfort.
Will jaw cracking go away on its own?
In many cases, yes—especially if triggered by temporary stress, fatigue, or minor strain. But if the issue persists beyond a few weeks or worsens, professional assessment is recommended to prevent chronic issues.
Action Plan: What to Do Next
If you're experiencing jaw cracking when chewing, start by observing patterns. Is it isolated? Pain-free? Infrequent? Then evaluate your habits: Are you stressed? Grinding your teeth? Chewing on one side only?
Implement the self-care steps outlined above for two to three weeks. If there’s no improvement—or if symptoms escalate—schedule a consultation with a dentist experienced in TMJ disorders. Early action can prevent long-term joint degeneration and chronic pain.
“The earlier we intervene in TMJ dysfunction, the better the chances of avoiding irreversible changes to the joint.” — Dr. Lena Patel, Dentist and TMJ Therapist
Conclusion
Jaw cracking when chewing is a common occurrence, often benign but sometimes a warning sign of deeper joint issues. By understanding the causes, recognizing red flags, and taking timely action, you can protect your jaw health and maintain comfortable daily function. Don’t dismiss persistent symptoms as “just a quirk”—your jaw plays a vital role in communication, nutrition, and overall well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?