Many people notice a clicking, popping, or cracking sound in their jaw when chewing, speaking, or opening their mouth wide. While occasional noise might seem harmless, persistent jaw popping can signal an underlying issue—most commonly related to the temporomandibular joint (TMJ). Left unaddressed, this condition may lead to pain, limited jaw movement, and chronic discomfort. Understanding the root causes and knowing how to manage symptoms can make a significant difference in daily comfort and long-term oral health.
Understanding the Temporomandibular Joint (TMJ)
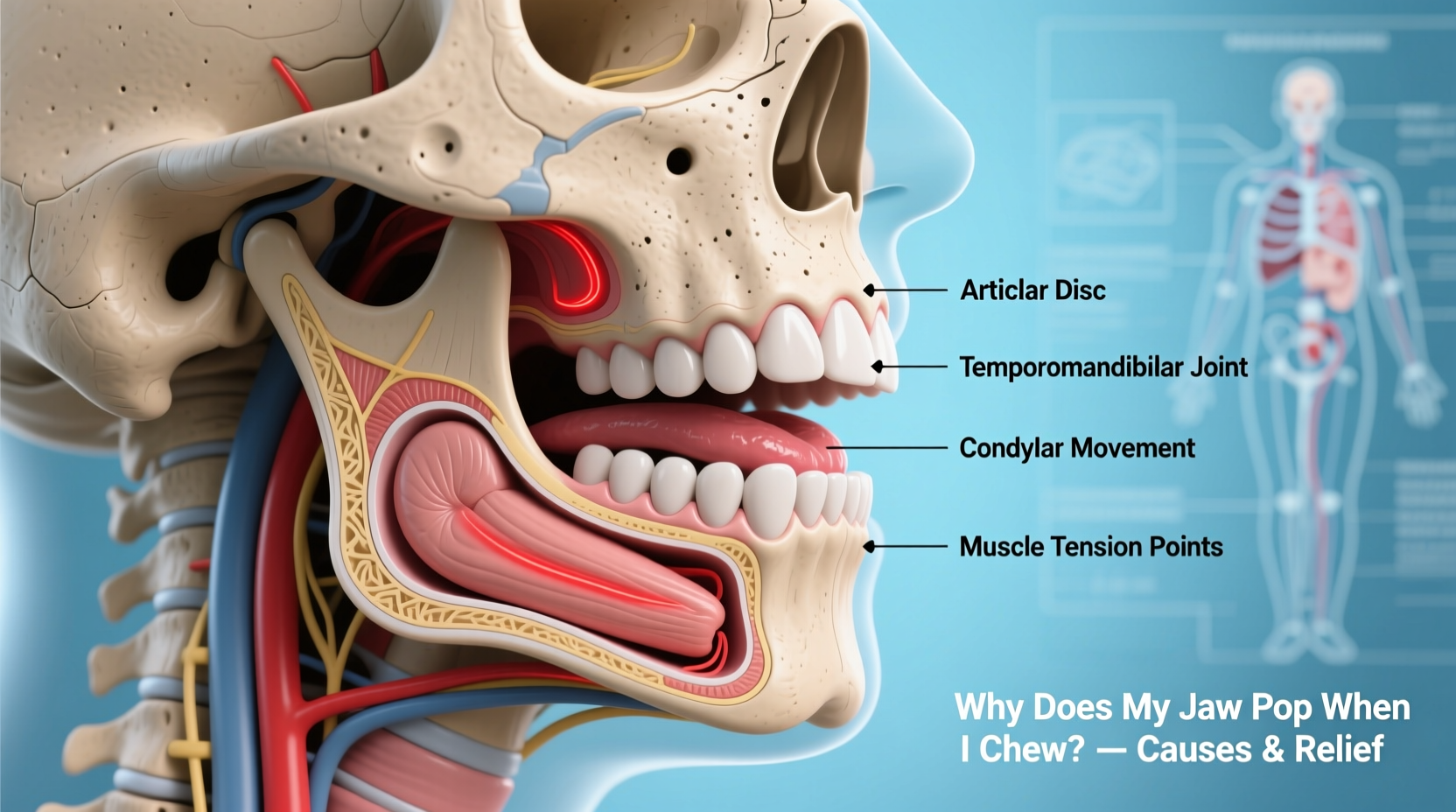
The temporomandibular joint connects your jawbone to your skull, just in front of each ear. These two joints work in tandem to allow smooth up-and-down and side-to-side motion necessary for chewing, talking, and yawning. A small disc of cartilage sits between the bones of the joint, acting as a cushion and enabling fluid movement.
When this disc becomes misaligned, inflamed, or damaged, it can result in abnormal sounds such as popping, clicking, or grating during jaw movement. The phenomenon is often referred to as \"crepitus.\" While not always painful, consistent popping may indicate developing dysfunction that could progress without intervention.
Anatomy plays a key role: because the TMJ is one of the most frequently used joints in the body and performs complex movements, it's particularly susceptible to strain and wear. Factors like muscle tension, joint degeneration, trauma, or habitual behaviors can all contribute to instability in the joint structure.
Common Causes of Jaw Popping During Chewing
Jaw popping isn’t a standalone diagnosis—it’s a symptom of mechanical changes within the joint or surrounding musculature. Several conditions and habits are known contributors:
- Misalignment of the articular disc: The most frequent cause. This shock-absorbing disc can shift out of place, causing a pop when it snaps back into position during jaw movement.
- Bruxism (teeth grinding or clenching): Often occurs at night and increases pressure on the TMJ, leading to inflammation and disc displacement over time.
- Arthritis: Osteoarthritis or rheumatoid arthritis can degrade the joint surfaces, resulting in friction and audible joint noise.
- Trauma or injury: A blow to the jaw or whiplash-type incident can damage the joint components directly.
- Poor posture: Forward head posture from prolonged screen use alters neck and jaw alignment, increasing stress on the TMJ.
- Stress-related tension: Emotional stress triggers unconscious jaw clenching, tightening the muscles around the joint.
- Dental malocclusion: Misaligned bite can unevenly distribute chewing forces, straining one side of the joint more than the other.
In many cases, jaw popping starts subtly—perhaps only noticeable during hard chewing—and worsens with continued strain. Early recognition allows for non-invasive management before structural damage sets in.
How to Relieve Pressure and Reduce Jaw Popping
Relief begins with reducing strain on the joint and supporting natural healing processes. Most mild-to-moderate cases respond well to conservative, at-home strategies combined with lifestyle adjustments.
1. Apply Warmth to Relax Muscles
Heat therapy improves blood flow and loosens tight jaw muscles. Use a warm towel or heating pad on the affected side for 10–15 minutes, twice daily—especially in the morning or after periods of stress.
2. Practice Gentle Jaw Stretching Exercises
Controlled exercises help restore range of motion and reposition the joint disc gradually. Try these simple routines:
- Resisted Opening: Place thumb under chin and gently press upward while slowly opening your mouth against light resistance. Hold for 5 seconds, repeat 5 times.
- Lateral Excursion: Slide jaw slowly to the left and right without tilting head. Perform 10 reps per side.
- Finger-Assisted Yawn: Insert two fingers vertically between front teeth and gently push downward to stretch the joint, mimicking a yawn. Do not force.
3. Modify Your Diet Temporarily
Give your jaw a rest by avoiding tough, chewy, or large-bite foods. Opt for soft meals like soups, stews, mashed potatoes, yogurt, and smoothies. Cut food into small pieces and chew evenly on both sides to prevent overloading one joint.
4. Manage Stress and Limit Clenching
Since emotional tension often manifests physically in the jaw, incorporate relaxation techniques such as deep breathing, meditation, or progressive muscle relaxation. Consider journaling or mindfulness apps if nighttime bruxism is suspected.
5. Improve Posture and Ergonomics
Sitting with your head forward shifts the mandible backward, compressing the TMJ. Adjust your workstation so monitors are at eye level, shoulders relaxed, and spine aligned. Take breaks every hour to reset posture.
“Patients who combine postural correction with targeted jaw exercises see faster improvement in joint stability and reduced clicking.” — Dr. Lena Patel, Physical Therapist Specializing in Orofacial Pain
When to See a Healthcare Professional
While self-care helps many individuals, certain warning signs indicate the need for medical assessment:
- Pain that radiates to the ear, temple, or neck
- Jaw locking open or closed
- Noticeable facial swelling near the joint
- Worsening frequency or intensity of popping
- Dental wear patterns suggesting grinding
A dentist, oral surgeon, or physical therapist trained in TMJ disorders can perform a clinical exam, possibly including imaging like MRI or panoramic X-rays, to assess disc position and joint integrity.
Treatment options may include:
- Custom night guards: Prevents tooth wear and reduces muscle strain during sleep.
- Physical therapy: Includes manual manipulation, ultrasound therapy, and neuromuscular retraining.
- Dental correction: Orthodontics or bite adjustment if malocclusion is contributing.
- Medication: Short-term use of anti-inflammatories or muscle relaxants under supervision.
- Injections: Corticosteroid or Botox injections in severe cases to reduce inflammation or spasm.
| Symptom | Self-Care Approach | Professional Treatment Needed? |
|---|---|---|
| Occasional pop, no pain | Monitor, apply heat, avoid gum | No |
| Frequent pop with mild ache | Stretching, diet change, stress reduction | Consider evaluation |
| Jaw locks or severe pain | Soft diet, avoid wide openings | Yes – seek care promptly |
| Clicking + ear ringing or headache | Posture correction, rest | Yes – likely linked dysfunction |
Real-Life Example: Recovery Through Consistent Care
Sarah, a 34-year-old graphic designer, began noticing her jaw popped loudly every time she ate apples or yawned. At first, she ignored it—until one morning she couldn’t open her mouth fully without sharp pain near her right ear. After a telehealth consultation, she was referred to a TMJ-specialized physical therapist.
Her diagnosis revealed anterior disc displacement with reduction—a common cause of popping. She started a regimen of daily heat application, gentle stretching, and ergonomic adjustments to her desk setup. She also received a custom-fitted night guard to address undiagnosed bruxism.
Within six weeks, the popping decreased significantly, and full mobility returned. By month three, the sound had nearly disappeared. Sarah continues preventive exercises twice weekly and avoids chewing gum—a habit she hadn’t realized contributed to her symptoms.
Prevention Checklist: Protect Your Jaw Long-Term
- ✅ Avoid chewing gum or biting nails/pens
- ✅ Chew food evenly on both sides of the mouth
- ✅ Limit wide yawning; support jaw when needed
- ✅ Practice daily posture checks (ears over shoulders)
- ✅ Use a supportive pillow to maintain neck alignment
- ✅ Schedule dental checkups to monitor bite and wear
- ✅ Incorporate stress-management practices regularly
Frequently Asked Questions
Is jaw popping dangerous?
Not always. Occasional, painless popping is common and often benign. However, if it becomes frequent, painful, or limits function, it may reflect progressive joint damage and should be evaluated.
Can a dentist fix jaw popping?
Yes. Dentists, especially those trained in TMJ disorders or neuromuscular dentistry, can diagnose the cause and offer treatments like occlusal splints, bite adjustments, or referrals to specialists for advanced care.
Will jaw popping go away on its own?
Sometimes. If caused by temporary strain or minor disc displacement, symptoms may resolve with rest and self-care. Chronic or worsening cases typically require intervention to prevent long-term complications like degenerative joint disease.
Conclusion: Take Action Before Discomfort Escalates
Your jaw is designed for thousands of movements each day, but it’s not indestructible. Popping during chewing is more than just a quirk—it’s a signal that something in the joint mechanism needs attention. Whether due to clenching, poor posture, or unnoticed dental issues, early action can prevent minor irritation from becoming chronic pain.
Start with simple, sustainable changes: apply warmth, modify your diet, stretch gently, and stay mindful of habits that strain your jaw. If symptoms persist beyond a few weeks or interfere with eating and speaking, don’t wait—consult a healthcare provider with experience in TMJ disorders.
With proper care, most people regain smooth, silent jaw function and avoid long-term complications. Listen to your body, act proactively, and protect one of your most essential daily functions.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?